Abstract
Background
Drug use among parenting women is a significant risk factor for a range of negative child outcomes, including exposure to violence, child maltreatment, and child behavior problems. Implementation of brief interventions with this population may be greatly facilitated by computer-based interventions.
Design
Randomized clinical trial with 4-month follow-up.
Setting/participants
Participants were 107 postpartum women recruited from an urban obstetric hospital primarily serving a low-income population. Women were randomized into assessment only versus assessment plus brief intervention conditions; 76 (71%) returned for follow-up evaluation.
Intervention
A 20-minute, single-session computer-based brief motivational intervention (based on Motivational Interviewing methods) combined with two nontailored mailings and voucher-based reinforcement of attendance at an initial intake/treatment session.
Main outcome measures
Illicit drug use as measured by qualitative urinalysis and self-report.
Results
Frequency of illicit drug use other than marijuana increased slightly for the control group, but declined among intervention group participants (p <0.05, between-groups Mann-Whitney U; d = 0.50); the magnitude of intervention effects on changes in marijuana use frequency was similar, but did not reach statistical significance. Point-prevalence analysis at follow-up did not show significant group differences in drug use. However, trends under a range of assumptions regarding participants lost to follow-up all favored the intervention group, with most effect sizes in the moderate range (ORs 1.4 to 4.7).
Conclusions
Results tentatively support the efficacy of this high-reach, replicable brief intervention. Further research should seek to replicate these findings and to further develop the computer as a platform for validated brief interventions.
INTRODUCTION
Data from the 2004 and 2005 National Survey on Drug Use and Health suggest that at least 3.9% of pregnant women report using an illicit drug in the past month1; the consequences of this prenatal drug use have been the focus of much attention and controversy.2 Drug use among parenting women, however, is much more prevalent (9.9% of nonpregnant women of childbearing age reported past month illicit drug use in the 2004–2005 National Survey on Drug Use and Health) and is also associated with a range of clear negative sequelae. Drug use among parenting women is an important risk factor for negative child outcomes such as exposure to violence,3 maltreatment,4–6 depression,7 behavioral problems,8 and substance use in adolescence.9–11
Several factors make the postpartum period an ideal point at which to address drug use among parenting women, including (1) the near-universality with which women give birth in hospitals, (2) the possible benefits of this period as a “teachable moment,”12 and (3) the efficacy of even very brief interventions for substance use disorders.13–17 However, the widespread implementation of brief interventions in primary care settings has been hindered by time limitations, with one estimate suggesting that conducting all recommended prevention-related activities would take a primary care physician 4.4 hours per working day.18 Additional obstacles have included logistical difficulties,19 discomfort with or lack of interest in behavioral interventions,20 and poor adherence to brief intervention guidelines even after training.21, 22
Computer-based approaches to primary care–based screening and intervention offer the possibility of inexpensive, replicable, upgradeable, and definable intervention processes that take advantage of the ubiquitous wait times in primary care settings.23 They also offer advantages in terms of disclosure of sensitive information, in that participants tend to disclose drug use more freely to computers than to live interviewers.24 However, it is currently unclear whether such interventions—particularly given the absence of human empathy and other relationship factors often seen as crucial to the behavior change process25—can lead to meaningful behavior change. Evidence from trials of tailored self-help mailings, which also do not involve individual therapeutic interactions, are largely encouraging.26–29 While a number of brief computer/Internet-based interventions are available, few have been rigorously evaluated.30 Two randomized trials with general adult samples found encouraging results for brief computer-based interventions with regard to smoking31 and problem alcohol use.32
It was predicted that a single computer-based intervention session combined with follow-up mailings would lead to reductions in drug use among urban postpartum women. In secondary analyses, the ability of motivation to change (as in previous reports33, 34), severity of substance abuse (given the brevity of the intervention), or IQ (due to the requirement of interaction with a computer) to moderate treatment effects was also explored. Given the cost effectiveness, reach, and replicability of brief computer-based interventions, even very small effect sizes could have tremendous population-level implications.23, 35, 36
METHODS
Participants
Participants in this study were 107 postpartum women recruited from an obstetric hospital in Detroit, Michigan that is affiliated with Wayne State University. Recruitment and baseline data collection took place between March of 2004 and April of 2005; follow-up data collection took place between June of 2004 and July of 2005. The primary criterion for inclusion in the study was self-report of any illicit drug use in the month prior to pregnancy. Women were excluded if they were aged <18 years; if they had not slept since giving birth (in order to reduce the influence of fatigue); if their infant was in the Neonatal Intensive Care Unit (in order to avoid seeking informed consent from distressed or grieving mothers); or if they had recently been administered narcotic pain medication.
Two procedures were implemented to provide additional participant protection and facilitate accurate self-report. First, the computer randomly selected a subset of women who did not report drug use or correlates of drug use (such as smoking or problem alcohol use) for inclusion in the study. This group was selected in a proportion programmed to equal approximately 10% of the study sample; this proportion, selected after consultation with colleagues and the Wayne State University Institutional Review Board (IRB), was deemed high enough to raise sufficient uncertainty regarding any particular participant’s drug use status. That is, this procedure removed any possibility of a woman’s drug use status being clear simply because of her participation in the study. Non–drug using participants (n =14) completed a modified assessment battery of equivalent length as other participants and were not considered in analyses. They did not contribute to the reported N of 107. Importantly, even the research assistant was blind to the drug use status of study participants throughout data collection, and had no ability to access research data.
Second, there was no table linking participant names with research data, thus making anonymous the participation in the study. Experimental condition was recorded along with research data and with names, allowing proper classification of data at both time points as either control or intervention. Between-groups analyses were therefore unaffected by this procedure. Within-groups analyses were facilitated through the use of multiple “non-identifying personal cues,” or questions regarding, for example, last digit of birth year or first initial of mother’s first name. None of these cues are included in the Department of Health and Human Services Privacy Rule. In research validating this approach, combinations of such cues allowed approximately 95% accurate matching of individuals over time without the use of identifying information.37
Procedures
Baseline data collection took place between March 2004 and April 2005, follow-up data collection took place between June 2004 and July 2005, and data analysis took place between August 2005 and April of 2006. Participants were approached in their private hospital rooms and given a brief description of the study. Those expressing interest were asked to provide verbal consent (using an information sheet) for a brief, anonymous, computer-based screening to determine eligibility. Those who were eligible on the computer-based screening were asked to provide written informed consent. All those providing consent completed the approximately 45-minute assessment, with a randomly determined half of participants also completing the 20-minute intervention. Randomization was conducted by the computer, did not involve stratification, and was not known a priori by any research personnel. As noted above, research assistants were blind to participants’ drug use status at all times. Research assistants were also kept blind to experimental condition until the completion of baseline data collection. All participants worked with the Tablet PC (a laptop with integrated touch screen, eliminating the need to use a keyboard or mouse) while in their hospital bed, using headphones for privacy. Participants were given a $30 gift certificate to Target stores (which do not sell alcohol or tobacco products), as compensation for their time and effort. All procedures were approved by the Wayne State University IRB.
Following completion of all baseline data-collection/intervention procedures, the computer informed the research assistant which participants were in the intervention condition; a randomly determined half of the non drug-using participants was also included in this group. These participants were told that, if they were interested and if such assistance were at all relevant for them, they could receive free taxi transportation and a $20 gift certificate by electing to attend a treatment intake/substance abuse evaluation at a local family-centered agency. All of these participants were also mailed attractive and easy-to-read brochures at four and nine weeks post-intervention. These brochures addressed infant and maternal health in general, with an emphasis on making or maintaining behavior change; drug use was briefly addressed along with smoking and other less stigmatizing behaviors. Given the risk that someone other than the participant might open the mailing, and thus obtain confidential information about the participant’s illicit drug use, the brochures were not tailored and did not imply or assume that the intended recipient was a user of illicit drugs.
Follow-up evaluations took place in the investigators’ offices at approximately 4 months post-baseline, and were conducted by a research assistant blind to experimental group as well as drug use status of the participant. Participants were contacted repeatedly by mail and later by phone following published tracking guidelines.38 Participants completing follow-up evaluation received a $60 gift certificate and assistance with transportation (either a $10 gas card or a taxi). In addition, participants who completed follow-up assessment were also eligible for a lottery-style drawing for an additional prize (ranging from hand lotion to a single $100 gift card).
Intervention
The software developed for this study was designed to be engaging, interactive, and easy to use. Initial versions were iteratively modified based on feedback from a panel of experts as well as from representative samples of low-income postpartum women. In a prior series of development studies, across all three development samples (total n = 47) and using a 1–5 rating scale in which 1 = not at all and 5 = very much, the mean rating for ease of use was 5 and the mean rating for overall liking was 4.7.23 The intervention also appeared to be associated with clear increases in state motivation to change drug use.23
The final software features a three-dimensional, mobile, and emotionally expressive animated narrator who reads all material (such that no reading literacy is required). The single-session intervention itself consists of three components based on motivational interviewing and brief intervention principles25: (1) feedback regarding the negative consequences of drug use that the participant reported, as well as self-reported readiness to change, and drug use as compared to that of all adult women; (2) pros and cons of drug use and related change, in which the participant chooses from lists of positive and negative aspects of drug use from their perspective; and (3) a summary and query regarding the participant’s interest in change, followed by optional goal-setting regarding drug use. Throughout the intervention section, the animated narrator “reflects” back the participant’s answers, emphasizes that whether or not to change is up to the participant, and expresses optimism regarding the possibility of success.
Measures
At both baseline and follow-up, all participants completed the Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST), a well-validated brief measure developed by the World Health Organization, that evaluates frequency of use as well as consequences of use for all categories of substances separately.39–41 The ASSIST has previously shown an internal consistency estimate of 0.80 and strong evidence of concurrent, predictive, construct, and discriminative validity (e.g., sensitivity of 0.80 to 0.97, and specificity of 0.71 to 0.96, in predicting structured interview-based determinations of drug abuse).42 Given the unreliability of self-report of drug use prior to pregnancy, the need for participant protection, and the tendency for women to eliminate or reduce drug use during pregnancy, the baseline ASSIST was completed with respect to the 3 months preceding pregnancy; at follow-up the ASSIST tapped drug use during the past 3 months. At follow-up qualitative urinalysis testing was conducted for methamphetamines, cocaine, marijuana, opiates, and benzodiazepines using the Redwood Biotech Redi Cup.™ All urinalysis results, which are displayed on the Redi CupTM as bars indicating that drug use is either present or not present, were read by a research assistant blind to participant experimental condition.
Baseline data collection also included eight self-report visual analogue scale items, developed for this study, tapping factors related to overall readiness to change. Factor analysis on these eight items using data provided by all 107 drug-using participants revealed a three-factor solution explaining 73.7% of the variance in total score. Factors included an intent to quit factor (e.g., “How ready are you to quit using drugs…?); a problem recognition factor (e.g., “How much of a problem do you think your drug use is?”); and a quitting self-efficacy factor (e.g., How confident are you that you could avoid drugs…if you really wanted to?”). Overall Cronbach’s alpha for the full eight-item measure was 0.76. Given the very small number of items in each factor and the adequate internal consistency of the full measure, analyses examining group equivalence utilized the mean of all eight items as a global indicator of motivation. Exploratory analyses utilized factor-based subscales as well as the global score.
Finally, participant IQ was measured using the two-subtest version of the Wechsler Abbreviated Scale of Intelligence.43 This brief measure was administered by trained and blinded research assistants at follow-up only. The Wechsler Abbreviated Scale of Intelligence utilizes similar procedures as the full Wechsler IQ test, and has demonstrated substantial associations with the full measure (r = 0.87).
Analyses
Effect size estimation was the primary concern in this study. Precision analyses suggested that an N of 107 was likely to be sufficient for allowing effect size estimation with continuous outcomes. Three primary analytic strategies were utilized. First, intervention-related changes in frequency of drug use were analyzed using Mann–Whitney U tests on changes in response to frequency items on the ASSIST (either none, once or twice, monthly, weekly, or daily). Responses to frequency items were averaged for all drug classes and for all drugs other than marijuana; the single Likert-scaled item was utilized for marijuana alone. Baseline values were carried forward for the 36 (29%) participants who did not complete follow-up evaluation.
Second, chi-square analyses were used to evaluate intervention-related differences
in point-prevalence abstinence from drugs. For these analyses, participants were considered
positive for drug use at follow-up if (1) urine testing indicated the presence of
metabolites of an illicit drug; or (2) their completed ASSIST protocol indicated illicit
drug use. Supplemental analyses were also run using qualitative urinalysis data alone.
Magnitude of effects was calculated via Odds Ratios and Logit d, an
equivalent to Cohen’s d for dichotomous outcomes (derived using the
formula: 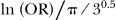 where ln (OR) = the natural logarithm of the odds ratio, and pi/3.5 = approximately 1.8138).44 Sensitivity/attrition analyses followed published guidelines for clinical trials with dichotomous outcomes and used “Attrition Analyzer” software developed by Shadish, Hu, and colleagues.45
where ln (OR) = the natural logarithm of the odds ratio, and pi/3.5 = approximately 1.8138).44 Sensitivity/attrition analyses followed published guidelines for clinical trials with dichotomous outcomes and used “Attrition Analyzer” software developed by Shadish, Hu, and colleagues.45
Third, the extent to which intervention effects were moderated by baseline severity of drug use (based primarily on ASSIST total score), IQ, or the three factors making up the motivation measure (intent to quit, self-efficacy, and problem recognition) was also examined. These analyses followed accepted guidelines for analyses of moderation.46
Overall, it was predicted that the computer-based intervention would yield significant changes in drug use relative to the control condition. The expectation was that effect sizes would be similar in magnitude to those found for traditional brief interventions.13, 14
RESULTS
See Figure 1 for a visual depiction of participant flow. The final group of 107 participants (52 control, 55 intervention) was almost exclusively African American and low income (Table 1). Mean age was 25.1 years. A total of 37 control group participants and 39 intervention group participants (71% overall) returned for follow-up at a mean delay of 119.8 days. There were no significant differences between intervention and control groups on any baseline substance use or readiness to change variables (Table 1). There were also no significant differences for these measures, either across or within experimental conditions, between participants lost to follow-up and those who completed follow-up.
Figure 1. Participant flow.
*Approximately 10% (n =14) of baseline participants were selected for lack of drug use reporting or risk, and removed at follow-up, in order to enhance participant protection. Flow diagram shows drug-using participants only.
Table 1.
Sample characteristics at baseline, by group (N = 107)
| Total (N = 107) | Control group (n = 52) | Intervention group (n = 55) | p value | |
|---|---|---|---|---|
| African American (%) | 104 (97.2) | 49 (94.2) | 55 (100) | 0.11 |
| Less than high school education (%) | 44 (41.1) | 22 (42.3) | 22 (40) | 0.81 |
| Public assistance in past year (%) | 95 (88.8) | 46 (88.5) | 50 (90.9) | 0.70 |
| Married (%) | 8 (7.5) | 5 (9.6) | 3 (5.5) | 0.41 |
| Full-time work in past 6 months (%) | 31 (29.0) | 12 (23.1) | 19 (34.5) | 0.19 |
| Infrequent marijuana use (monthly or less) in 3 months prior to pregnancy (%) | 29 (27.1) | 14 (26.9) | 15 (27.3) | 0.97 |
| Weekly or daily marijuana use in 3 months prior to pregnancy (%) | 67 (62.6) | 31 (59.6) | 36 (65.5) | 0.53 |
| Drug use other than marijuana in three months prior to pregnancy (%) | 13 (12.1) | 7 (13.5) | 6 (10.9) | 0.69 |
| Age (SD) | 25.1 (5.6) | 24.2 (5.4) | 25.9 (5.7) | 0.12 |
| IQ (SD) | 86.5 (10.3) | 86.8 (9.8) | 86.3 (11.1) | 0.83 |
| Motivation to change (SD) | 61.7 (18.9) | 63.0 (17.2) | 60.7 (20.4) | 0.54 |
Note. Significance values for dichotomous data are based on Chi-square analyses or Fisher’s exact test (with race, for which Chi-square assumptions are violated); t-tests used for IQ and motivation to change. “Public assistance” refers to receipt of food stamps, Women, Infants, and Children food supplements (WIC), or Temporary Assistance for Needy Families (TANF).
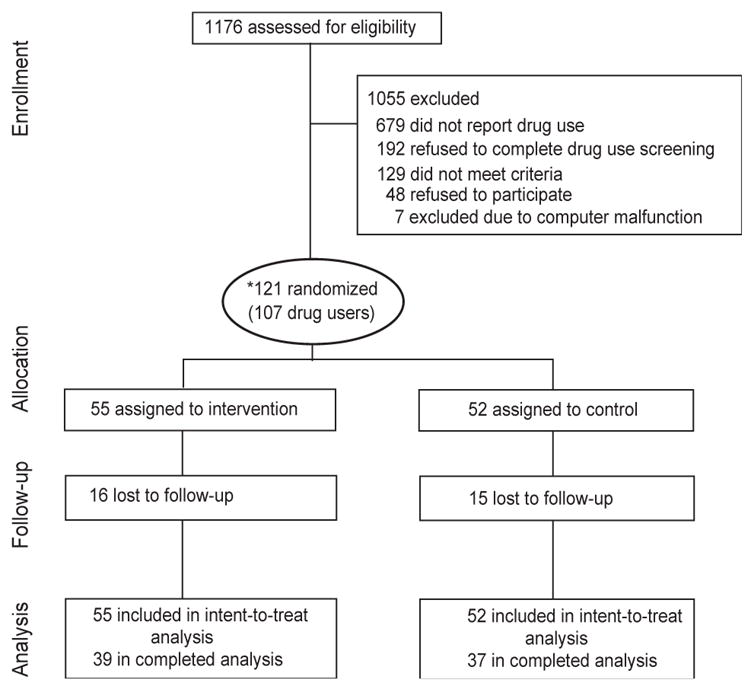
No participants in the intervention condition received the additional gift certificate for attendance at a treatment intake/substance abuse evaluation, and only one participant in the intervention group reported receiving any services during the follow-up period. Despite this, change score analysis of self-report data indicated significant between-group differences in changes in drug use over time (Figure 2). This effect was significant for drug use frequency averaged across all substances (p =0.042, Mann Whitney U test, Cohen’s d =0.46, 95% CI =0.15, 1.53) and for illicit drugs other than marijuana (p =0.032, Mann Whitney U test, Cohen’s d =0.40, 95% CI =0.02, 0.78), but not for marijuana alone (p =0.202, Mann Whitney U test, Cohen’s d =0.39, 95% CI =0.01, 0.97). As noted above, these analyses were conducted with the full sample of 107 using a last-observation-carried-forward approach for those lost to follow-up; results did not differ when data were analyzed using completers only.
Figure 2. Mean self-reported drug use frequency at baseline and 4-month follow-up.
Note. N =107; data missing at follow-up were replaced with baseline values. Frequency was reported on a 0–4 scale, where 0 = “Never” and 4 = “Daily or almost daily.”
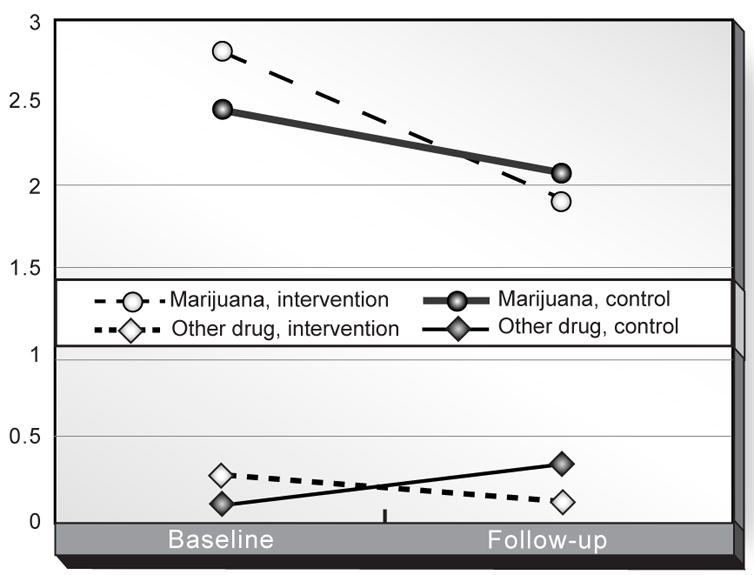
In contrast, no group differences reached statistical significance in analysis of dichotomous drug-use data (which, in order to maximize variance, reflected either marijuana use at least weekly or use of drugs other than marijuana at any point in the last 3 months). However, as predicted, trends consistently favored the intervention group (Figure 3), with effect sizes in the small to moderate range (Table 2).
Figure 3. Proportion of participants using drugs at 4-month follow-up, per self-report and/or urinalysis, by group (n =76).
Note. All comparisons were nonsignificant; a trend was observed for “any drug use,” χ (1) = 3.0, p =0.085.
Table 2.
Intervention effect sizes for any drug use, marijuana use, and drugs other than marijuana, for observed data and hypothetical scenarios for those lost to follow-up
| Any drug use | Marijuana only | Cocaine, opiates, or amphetamines | |
|---|---|---|---|
| Observed data | |||
| Odds ratio (95% CI) | 2.48 (0.59, 10.42) | 2.13 (0.58, 7.78) | 2.41 (0.66, 8.83) |
| Logit d | 0.50 | 0.42 | 0.48 |
| N | 76 | 76 | 76 |
| Urinalysis data only | |||
| Odds ratio (95% CI) | 1.93 (0.65, 5.69) | 1.63 (0.57, 4.66) | 4.67 (0.49, 44.05) |
| Logit d | 0.36 | 0.27 | 0.85 |
| N | 70 | 70 | 70 |
| Presuming 0% success in all lost to f/u | |||
| Odds Ratio (95% CI) | 2.38 (0.58, 5.90) | 2.04 (0.58, 7.24) | 1.39 (0.64, 3.01) |
| Logit d | 0.48 | 0.39 | 0.18 |
| N | 107 | 107 | 107 |
| Applying observed success rates for control and intervention groups to participants lost to attrition | |||
| Odds ratio (95% CI) | 2.67 (0.78, 9.11) | 1.92 (0.65, 5.63) | 2.19 (0.75, 6.44) |
| Logit d | 0.54 | 0.36 | 0.43 |
| N | 107 | 107 | 107 |
| Switching observed success rates for control and intervention groups | |||
| Odds ratio (95% CI) | 1.3 (0.42, 4.06) | 1.43 (0.50, 4.08) | 1.23 (0.44, 3.47) |
| Logit d | 0.14 | 0.20 | 0.11 |
| N | 107 | 107 | 107 |
Note. Marijuana use reflects use weekly or greater by self-report, and/or qualitative urinalysis. Other drug use reflects self-reported use in the past 3 months and/or a positive urinalysis, except where specified (urinalysis data only).
Sensitivity/attrition analysis, considering various assumptions regarding the drug use status of participants lost to follow-up, is also presented in Table 2. Nearly all projected outcome scenarios for participants lost to follow-up yielded lower effects, but small to moderate positive effects were present across all assumptions. Further, similar effect sizes (although somewhat weaker for marijuana and stronger for other drugs) were obtained when analyses were conducted using urinalysis data only (Table 2).
Moderator analyses revealed no interaction between intervention and potential moderators of intervention efficacy (baseline severity of drug use, IQ, motivation, or self-efficacy) in predicting dichotomous drug use outcomes (collapsing across all drug classes).
DISCUSSION
This late Phase-I trial was conducted to provide preliminary evaluation of the efficacy of a brief intervention consisting primarily of a single computer-based intervention session. Findings suggest that the combined intervention—under a range of assumptions regarding attrition, and using various outcomes—had a small to moderate effect on frequency of cocaine, opiate, or amphetamine use in this sample. Findings with respect to other drug use outcomes were not significant, but effect sizes were all in the small to medium range and consistently favored the intervention group. This finding is consistent with the larger literature on brief interventions utilizing a single motivational session.16, 47, 48
How such brief encounters could lead to measurable changes in substance use is unclear. Motivational Interviewing, the approach most influential in the development of this intervention, is thought to work by resolving ambivalence (a process facilitated by accurate empathy) and by selective elicitation and reinforcement of movements toward change49; the feedback element often included with this approach is thought to work by increasing perceived discrepancies between goals and current behavior in a process similar to cognitive dissonance.25 The efficacy of similar approaches such as brief advice,16, 50 which often lack the heavy emphasis on empathy present in Motivational Interviewing, suggests that other mechanisms may be at play as well. Evidence that even extended assessment can lead to effects similar to those found for brief interventions51, 52 raises the parsimonious possibility that the simple act of focusing on the problem (perhaps particularly or only when resistance is not elicited) may be associated with change. Such nonthreatening, nonjudgmental focusing on one’s substance use and its consequences may be quite rare for individuals with substance use disorders. Formal attention to the substance use was rare in this group; only 4 of 76 (5.3%) of participants reported receiving any formal substance abuse services during the follow-up period, and only 10 (9.3%) reported ever having received any substance abuse counseling.
The use of a computerized brief intervention focusing on drug abuse in the immediate postpartum period is unique. Most women who use drugs either quit or cut down during pregnancy, and return to pre-pregnancy levels of use relatively soon after delivery.53 Consistent with this, women in the control group of this sample, at follow-up, reported using drugs other than marijuana at rates similar to those reported for the period preceding pregnancy. In contrast, women in the intervention condition reported less such drug use than in the pre-pregnancy period, suggesting that they may have been more likely to maintain pregnancy-related reductions in use. This suggestion is consistent with anecdotal evidence obtained during baseline data collection: many women in the intervention condition indicated that they had planned to “party” immediately upon returning home, but that the intervention was leading them to re-think those plans.
Interventions based on contingency management have a strong record of success.54–57 The contingent reinforcement component of this study was small in value ($25 on one occasion), could not be provided until days after completion of the targeted behavior, and the targeted behavior (attending a substance abuse treatment intake session) was a major step rather than an incremental one. It was hoped that the reinforcement combined with the free transportation might help tip the balance in individuals already considering treatment. However, the results suggest that few participants in this study were considering treatment: at follow-up, only 4 of 76 women (5%) reported having received any form of treatment (including 12-step involvement) in the past month.
Several limitations of this study should be noted. First, generalizability may be limited due to the relatively small N, attrition of 29%, and restriction to low-income urban mothers. Sensitivity/attrition analysis suggests that while most possible patterns of results in participants lost to follow-up still support the present findings, there are scenarios in which the present findings are dramatically reduced in magnitude. Second, power limitations prevented verification of treatment effects on the dichotomous outcomes, despite effect sizes in the small to moderate range. These power limitations appear to have resulted from the relatively small N but also from restricted variability in drug use: relatively few participants reported using cocaine, opiates, or amphetamines, but the majority did use marijuana. A final limitation is that the study design did not allow evaluation of the relative influence of the computer-based session versus the two nontailored mailings. Such dismantling of components is an appropriate strategy for later in the intervention development process.
Despite these limitations, the present findings are encouraging. This is the first known experimental evidence that a brief computer-based intervention can reduce illicit drug use. While prospective users of such technology may often be unlikely to return for multiple sequential sessions, opportunistic single-session approaches such as that used in this study may prove to be easily integrated into ongoing primary care or other high-reach settings. Further, the approach utilized in this study is but one of a nearly infinite range of approaches that could be investigated. This is a rich area for further study.
Acknowledgments
Funding for this study was provided by grants DA00516 and DA14621 from the National Institute on Drug Abuse (PI, Ondersma). The authors gratefully acknowledge the assistance of Jessica R. Beatty, Sara K. Chase, Aulesha V. Harris, Laura Strathdee, and Andrea Sumpter in participant recruitment and data collection.
No financial conflict of interest was reported by the authors of this paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Substance Abuse and Mental Health Services Administration. Overview of Findings from the 2004 National Survey on Drug Use and Health. Office of Applied Studies, NSDUH Series H-27, DHHS Publication No. SMA 05-4061; Rockville, MD: 2005. [Google Scholar]
- 2.Lester BM, Andreozzi L, Appiah L. Substance use during pregnancy: time for policy to catch up with research. Harm Reduct J. 2004 Apr 20;1(1):5. doi: 10.1186/1477-7517-1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ondersma SJ, Delaney-Black V, Covington CY, Nordstrom B, Sokol RJ. The Association Between Caregiver Substance Abuse and Self-Reported Violence Exposure Among Young Urban Children. J Trauma Stress. 2006;19:107–18. doi: 10.1002/jts.20105. [DOI] [PubMed] [Google Scholar]
- 4.Ondersma SJ. Predictors of neglect within low-SES families: The importance of substance abuse. Am J Orthopsychiatry. 2002 Jul;72(3):383–91. doi: 10.1037/0002-9432.72.3.383. [DOI] [PubMed] [Google Scholar]
- 5.Besinger BA, Garland AF, Litrownik AJ, Landsverk JA. Caregiver substance abuse among maltreated children placed in out-of- home care. Child Welfare. 1999;78(2):221–39. 3/1999. [PubMed] [Google Scholar]
- 6.Chaffin M, Kelleher K, Hollenberg J. Onset of physical abuse and neglect: psychiatric, substance abuse, and social risk factors from prospective community data. Child Abuse & Neglect. 1996;20(3):191–203. doi: 10.1016/s0145-2134(95)00144-1. [DOI] [PubMed] [Google Scholar]
- 7.Reinherz HZ, Giaconia RM, Hauf AM, Wasserman MS, Paradis AD. General and specific childhood risk factors for depression and drug disorders by early adulthood. J Am Acad Child Adolesc Psychiatry. 2000;39(2):223–31. doi: 10.1097/00004583-200002000-00023. [DOI] [PubMed] [Google Scholar]
- 8.Weissman MM, Warner V, Wickramaratne PJ, Kandel DB. Maternal smoking during pregnancy and psychopathology in offspring followed to adulthood. J Am Acad Child Adolesc Psychiatry. 1999;38(7):892–9. doi: 10.1097/00004583-199907000-00020. [DOI] [PubMed] [Google Scholar]
- 9.Hoffmann JP, Su SS. Parental substance use disorder, mediating variables and adolescent drug use: a nonrecursive model. Addiction. 1998;93(9):1351–64. doi: 10.1046/j.1360-0443.1998.93913516.x. [DOI] [PubMed] [Google Scholar]
- 10.Jacob T, Waterman B, Heath A, et al. Genetic and Environmental Effects on Offspring Alcoholism: New Insights Using an Offspring-of-Twins Design. Arch Gen Psychiatry. 2003;60(12):1265–72. doi: 10.1001/archpsyc.60.12.1265. December 1, 2003. [DOI] [PubMed] [Google Scholar]
- 11.Kilpatrick DG, Acierno R, Saunders B, Resnick HS, Best CL, Schnurr PP. Risk factors for adolescent substance abuse and dependence: data from a national sample. J Consult Clin Psychol. 2000;68(1):19–30. doi: 10.1037//0022-006x.68.1.19. [DOI] [PubMed] [Google Scholar]
- 12.McBride CM, Emmons KM, Lipkus IM. Understanding the potential of teachable moments: the case of smoking cessation. Health Educ Res. 2003 Apr;18(2):156–70. doi: 10.1093/her/18.2.156. [DOI] [PubMed] [Google Scholar]
- 13.Moyer A, Finney JW, Swearingen CE, Vergun P. Brief interventions for alcohol problems: a meta-analytic review of controlled investigations in treatment-seeking and nontreatment-seeking populations. Addiction. 2002 Mar;97(3):279–92. doi: 10.1046/j.1360-0443.2002.00018.x. [DOI] [PubMed] [Google Scholar]
- 14.Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: a meta-analysis of controlled clinical trials. J Consult Clin Psychol. 2003 Oct;71(5):843–861. doi: 10.1037/0022-006X.71.5.843. [DOI] [PubMed] [Google Scholar]
- 15.Hettema J, Steele J, Miller WR. Motivational Interviewing. Annual Review of Clinical Psychology. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- 16.Lancaster T, Stead L. Physician advice for smoking cessation. Cochrane Database Syst Rev. 2004;(4):CD000165. doi: 10.1002/14651858.CD000165.pub2. [DOI] [PubMed] [Google Scholar]
- 17.Wilk AI, Jensen NM, Havighurst TC. Meta-analysis of randomized control trials addressing brief interventions in heavy alcohol drinkers. J Gen Intern Med. 1997;12(5):274–283. doi: 10.1046/j.1525-1497.1997.012005274.x. 5/1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yarnall KS, Pollak KI, Ostbye T, Krause KM, Michener JL. Primary care: is there enough time for prevention? Am J Public Health. 2003 Apr;93(4):635–41. doi: 10.2105/ajph.93.4.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aalto M, Pekuri P, Seppa K. Obstacles to carrying out brief intervention for heavy drinkers in primary health care: a focus group study. Drug Alcohol Rev. 2003 Jun;22(2):169–73. doi: 10.1080/09595230100100606. [DOI] [PubMed] [Google Scholar]
- 20.Beich A, Gannik D, Malterud K. Screening and brief intervention for excessive alcohol use: qualitative interview study of the experiences of general practitioners. BMJ. 2002 Oct 19;325(7369):870. doi: 10.1136/bmj.325.7369.870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.DePue JD, Goldstein MG, Schilling A, et al. Dissemination of the AHCPR clinical practice guideline in community health centres. Tob Control. 2002 Dec;11(4):329–35. doi: 10.1136/tc.11.4.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aalto M, Pekuri P, Seppa K. Primary health care professionals' activity in intervening in patients' alcohol drinking during a 3-year brief intervention implementation project. Drug Alcohol Depend. 2003 Jan 24;69(1):9–14. doi: 10.1016/s0376-8716(02)00228-4. [DOI] [PubMed] [Google Scholar]
- 23.Ondersma SJ, Chase SK, Svikis DS, Schuster CR. Computer-based brief motivational intervention for perinatal drug use. J Subst Abuse Treat. 2005 Jun;28(4):305–12. doi: 10.1016/j.jsat.2005.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Newman JC, Des Jarlais DC, Turner CF, Gribble J, Cooley P, Paone D. The differential effects of face-to-face and computer interview modes. Am J Public Health. 2002;92(2):294–7. doi: 10.2105/ajph.92.2.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2. New York: Guilford; 2002. [Google Scholar]
- 26.Strecher VJ. Computer-tailored smoking cessation materials: a review and discussion. Patient Educ Couns. 1999;36(2):107–17. doi: 10.1016/s0738-3991(98)00128-1. [DOI] [PubMed] [Google Scholar]
- 27.Sobell LC, Sobell MB, Leo GI, Agrawal S, Johnson-Young L, Cunningham JA. Promoting self-change with alcohol abusers: a community-level mail intervention based on natural recovery studies. Alcohol Clin Exp Res. 2002 Jun;26(6):936–48. [PubMed] [Google Scholar]
- 28.Prochaska JO, Velicer WF, Redding C, et al. Stage-based expert systems to guide a population of primary care patients to quit smoking, eat healthier, prevent skin cancer, and receive regular mammograms. Prev Med. 2005 Aug;41(2):406–16. doi: 10.1016/j.ypmed.2004.09.050. [DOI] [PubMed] [Google Scholar]
- 29.Lancaster T, Stead LF. Self-help interventions for smoking cessation. Cochrane Database Syst Rev. 2002;(3):CD001118. doi: 10.1002/14651858.CD001118. [DOI] [PubMed] [Google Scholar]
- 30.Copeland J, Martin G. Web-based interventions for substance use disorders; A qualitative review. J Subst Abuse Treat. 2004 Mar;26(2):109–16. doi: 10.1016/S0740-5472(03)00165-X. [DOI] [PubMed] [Google Scholar]
- 31.Etter JF, Perneger TV. Effectiveness of a computer-tailored smoking cessation program: a randomized trial. Arch Intern Med. 2001;161(21):2596–601. doi: 10.1001/archinte.161.21.2596. [DOI] [PubMed] [Google Scholar]
- 32.Hester RK, Squires DD, Delaney HD. The Drinker's Check-up: 12-month outcomes of a controlled clinical trial of a stand-alone software program for problem drinkers. J Subst Abuse Treat. 2005 mar;28(2):159–69. doi: 10.1016/j.jsat.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 33.Rohsenow DJ, Monti PM, Martin RA, et al. Motivational enhancement and coping skills training for cocaine abusers: effects on substance use outcomes. Addiction. 2004 Jul;99(7):862–74. doi: 10.1111/j.1360-0443.2004.00743.x. [DOI] [PubMed] [Google Scholar]
- 34.Stotts AL, Schmitz JM, Rhoades HM, Grabowski J. Motivational interviewing with cocaine- dependent patients: a pilot study. J Consult Clin Psychol. 2001;69(5):858–62. doi: 10.1037//0022-006x.69.5.858. [DOI] [PubMed] [Google Scholar]
- 35.Heller RF, Dobson AJ. Disease impact number and population impact number: population perspectives to measures of risk and benefit. BMJ. 2000 Oct 14;321(7266):950–953. doi: 10.1136/bmj.321.7266.950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rosnow RL, Rosenthal R. Statistical procedures and the justification of knowledge in psychological science. Am Psychol. 1989;44:1276–84. [Google Scholar]
- 37.Strathdee LA, Ondersma SJ, Beatty JR, Moore D. A Novel Methodology for "Anonymous" Clinical Trials: Better Data and Better Participant Protection without Certificates of Confidentiality?; Poster presented at the 67th Annual Scientific Meeting of the College of Problems on Drug Dependence; Orlando, FL. 2005. [Google Scholar]
- 38.Scott CK. A replicable model for achieving over 90% follow-up rates in longitudinal studies of substance abusers. Drug Alcohol Depend. 2004 Apr 9;74(1):21–36. doi: 10.1016/j.drugalcdep.2003.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Newcombe D, Humeniuk R, Hallet C, Ali R. Parkside, Australia: Drug & Alcohol Services Council of Australia; 2003. Validation of the World Health Organization Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) and Pilot Brief Intervention. [Google Scholar]
- 40.WHO ASSIST Working Group. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility. Addiction. 2002 Sep;97(9):1183–94. doi: 10.1046/j.1360-0443.2002.00185.x. [DOI] [PubMed] [Google Scholar]
- 41.Newcombe DA, Humeniuk RE, Ali R. Validation of the World Health Organization Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): report of results from the Australian site. Drug Alcohol Rev. 2005 May;24(3):217–26. doi: 10.1080/09595230500170266. [DOI] [PubMed] [Google Scholar]
- 42.Humeniuk R, Ali R. A technical report of phase II findings of the WHO ASSIST Project; World Health Organization: 2006. Validation of the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) and pilot brief intervention. [Google Scholar]
- 43.The Psychological Corporation. WASI Manual. San Antonio: The Psychological Corporation; 1999. [Google Scholar]
- 44.Hasselblad V, Hedges LV. Meta-analysis of screening and diagnostic tests. Psychol Bull. 1995;117:167–78. doi: 10.1037/0033-2909.117.1.167. [DOI] [PubMed] [Google Scholar]
- 45.Shadish WR, Hu X, Glaser RR, Kownacki R, Wong S. A method for exploring the effects of attrition in randomized experiments with dichotomous outcomes. Psychological Methods. 1998;3:3–22. [Google Scholar]
- 46.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–82. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 47.Ferreira-Borges C. Effectiveness of a brief counseling and behavioral intervention for smoking cessation in pregnant women. Prev Med. 2005 Jul;41(1):295–302. doi: 10.1016/j.ypmed.2004.11.013. [DOI] [PubMed] [Google Scholar]
- 48.Bertholet N, Daeppen JB, Wietlisbach V, Fleming M, Burnand B. Reduction of alcohol consumption by brief alcohol intervention in primary care: systematic review and meta-analysis. Arch Intern Med. 2005 May 9;165(9):986–95. doi: 10.1001/archinte.165.9.986. [DOI] [PubMed] [Google Scholar]
- 49.Miller WR. [Accessed January 18, 2006.];Toward a theory of Motivational Interviewing Online slide presentation. doi: 10.1037/a0016830. Available at: http://www.motivationalinterview.org/library/MItheory_files/v3_document.htm. [DOI] [PMC free article] [PubMed]
- 50.Fleming MF, Mundt MP, French MT, Manwell LB, Stauffacher EA, Barry KL. Brief physician advice for problem drinkers: long-term efficacy and benefit–cost analysis. Alcohol Clin Exp Res. 2002;26(1):36–43. [PubMed] [Google Scholar]
- 51.Wells EA, Beadnell B, Calsyn DA, et al. Motivational enhancement to decrease drug use among cocaine users: Six-month follow-up results; Poster presented at the Sixty-Sixth Annual Scientific Meeting of the College of Problems on Drug Dependence; San Juan, Puerto Rico. 2004. [Google Scholar]
- 52.Epstein EE, Drapkin ML, Yusko DA, Cook SM, McCrady BS, Jensen NK. Is alcohol assessment therapeutic? Pretreatment change in drinking among alcohol-dependent women. J Stud Alcohol. 2005 May;66(3):369–78. doi: 10.15288/jsa.2005.66.369. [DOI] [PubMed] [Google Scholar]
- 53.Office of Applied Studies. Pregnancy and substance use. The NSDUH Report [ http://www.oas.samhsa.gov/2k3/pregnancy/pregnancy.htm.
- 54.Rhodes GL, Saules KK, Helmus TC, et al. Improving on-time counseling attendance in a methadone treatment program: a contingency management approach. Am J Drug Alcohol Abuse. 2003;29(4):759–73. doi: 10.1081/ada-120026259. [DOI] [PubMed] [Google Scholar]
- 55.Jones HE, Haug N, Silverman K, Stitzer M, Svikis D. The effectiveness of incentives in enhancing treatment attendance and drug abstinence in methadone-maintained pregnant women. Drug Alcohol Depend. 2001;61(3):297–306. doi: 10.1016/s0376-8716(00)00152-6. [DOI] [PubMed] [Google Scholar]
- 56.Silverman K, Preston KL, Stitzer ML, Schuster CR. Efficacy and versatility of voucher-based reinforcement in drug abuse treatment. In: Higgins ST, Silverman K, editors. Motivating behavior change among illicit-drug abusers: Research on contingency management interventions. Washington, DC: American Psychological Association; 1999. pp. 163–81. [Google Scholar]
- 57.Silverman K, Higgins ST, Brooner RK, et al. Sustained cocaine abstinence in methadone maintenance patients through voucher-based reinforcement therapy. Arch Gen Psychiatry. 1996;53(5):409–15. doi: 10.1001/archpsyc.1996.01830050045007. [DOI] [PubMed] [Google Scholar]


