Abstract
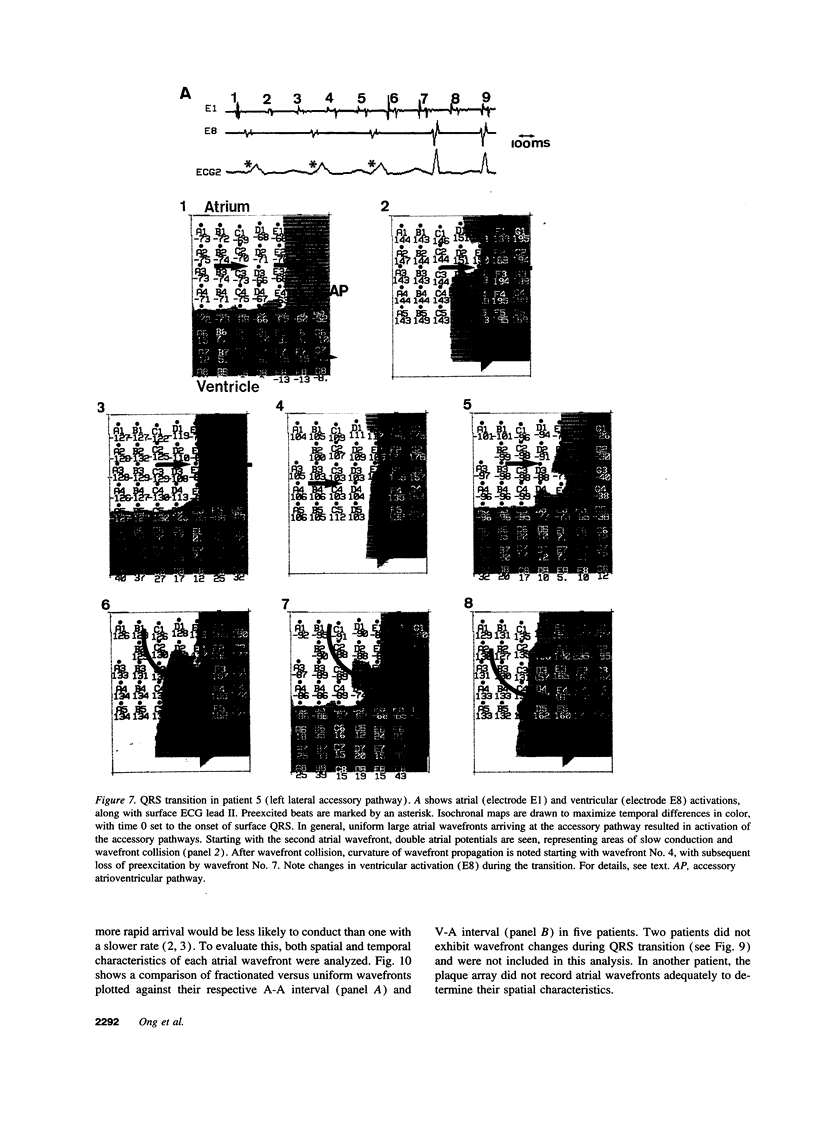
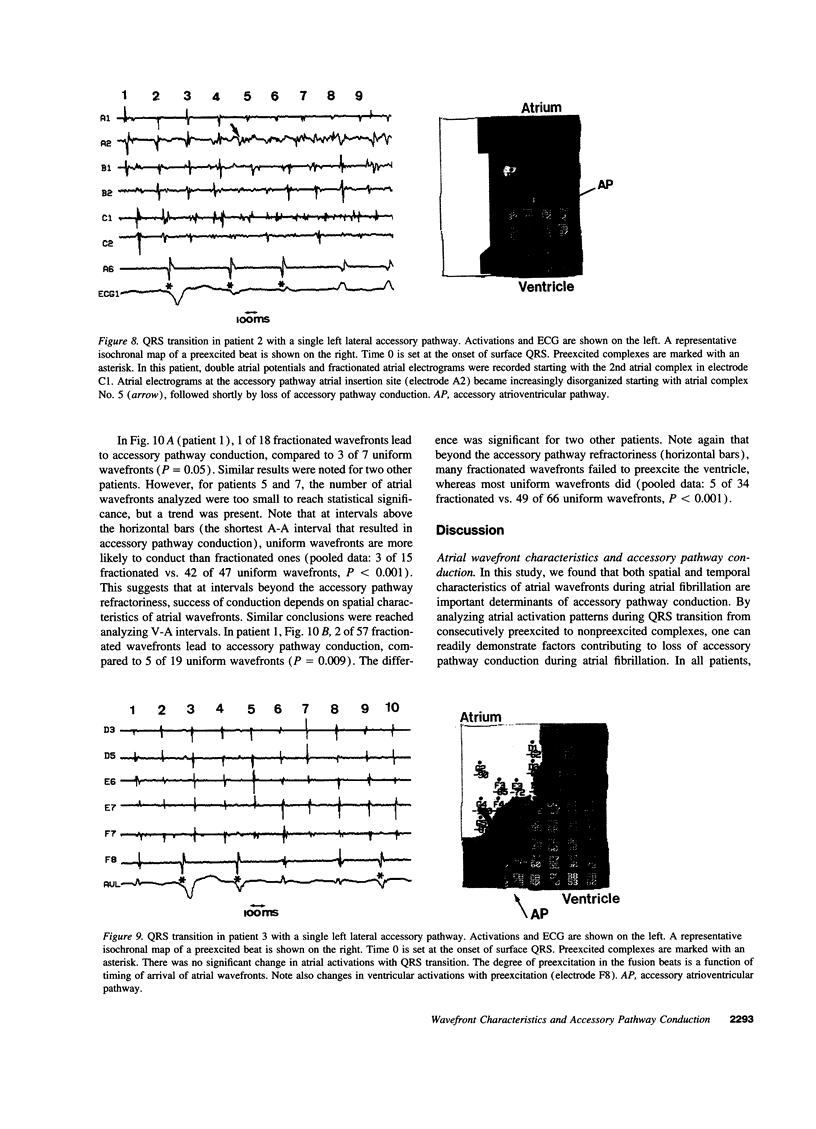
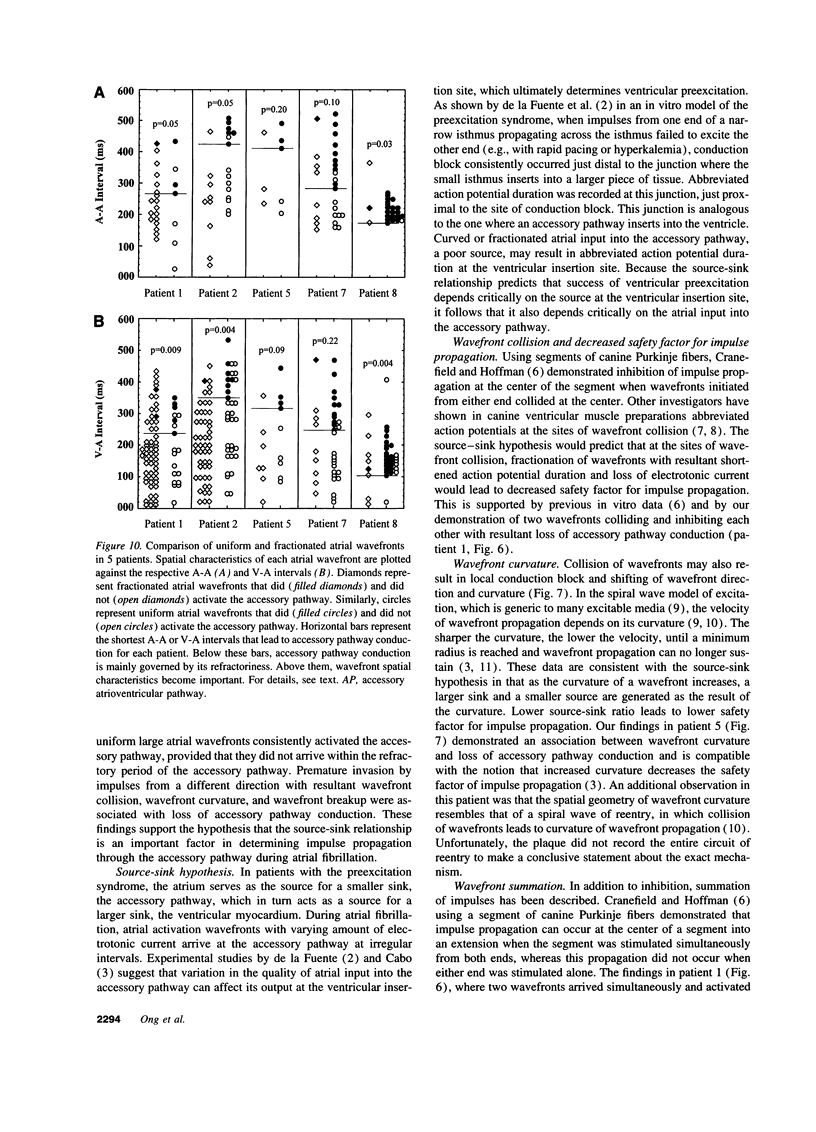
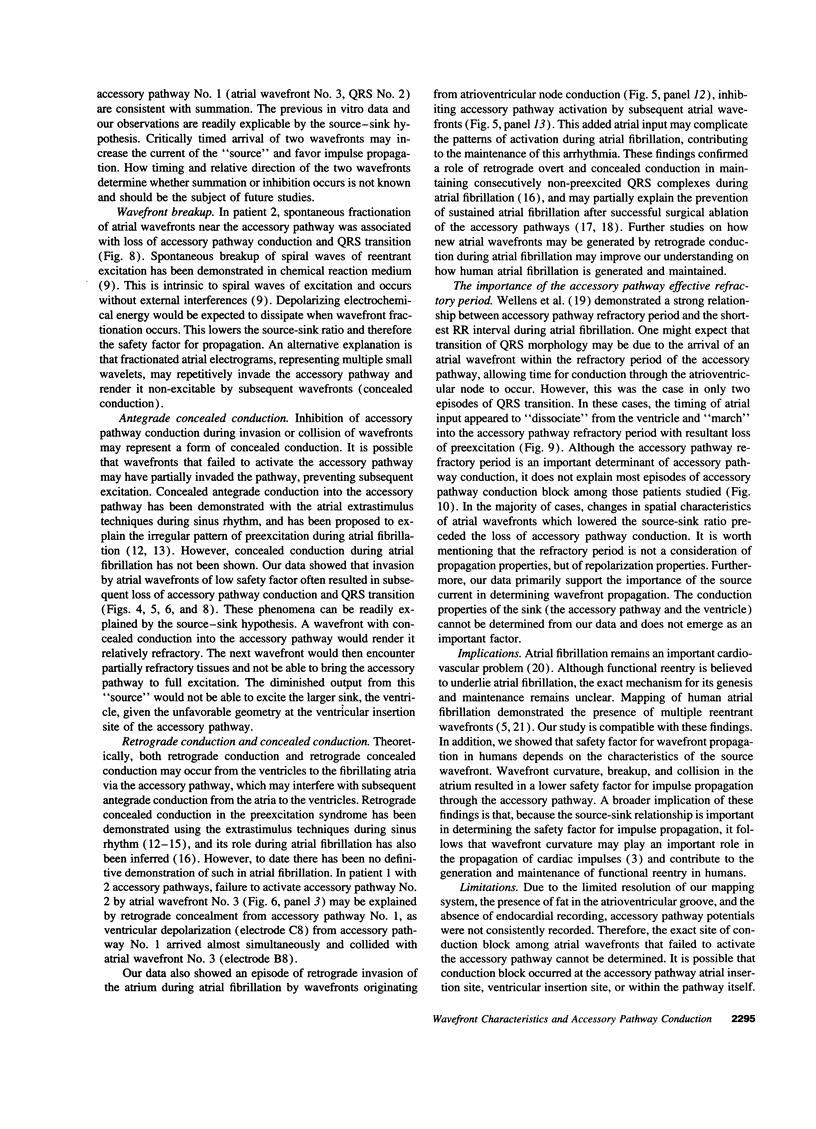
Although the source-sink relationship for impulse propagation in cardiac tissues has been demonstrated in vitro, there has been no verification of this hypothesis in humans. Accordingly, eight patients undergoing surgical division of their accessory pathways were studied. A 56-channel (7 x 8) bipolar plaque electrode array was placed over the atrioventricular groove on the accessory pathway and atrial fibrillation electrically induced. 10 episodes of QRS transition from consecutively preexcited to nonpreexcited complexes were analyzed. This showed that consecutively preexcited QRS complexes were always associated with uniform large atrial wavefronts. Immediately prior to QRS transition, four general types of changes were observed: (a) premature invasion by secondary wavefronts creating local conduction block (n = 5); (b) wavefront collision leading to wavefront curvature (n = 2); (c) transition from a uniform large atrial wavefront to multiple fractionated small wavefronts (n = 1); and (d) uniform atrial wavefronts "marching" into the accessory pathway refractory period (n = 2). We conclude that local atrial wavefront characteristics are important factors influencing impulse propagation through the accessory pathway. The findings that local wavefront collision, curvature, or fractionation often precede loss of accessory pathway conduction support the notion that source-sink relationship is an important determinant of the safety factor for impulse propagation in the human heart.
Full text
PDF


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Cabo C., Pertsov A. M., Baxter W. T., Davidenko J. M., Gray R. A., Jalife J. Wave-front curvature as a cause of slow conduction and block in isolated cardiac muscle. Circ Res. 1994 Dec;75(6):1014–1028. doi: 10.1161/01.res.75.6.1014. [DOI] [PubMed] [Google Scholar]
- Chen P. S., Dembitsky W. P., Fleck R. P., Calisi C. M., Feld G. K. Demonstration of accessory pathway interaction by computerized mapping in preexcitation syndrome. Pacing Clin Electrophysiol. 1990 Jul;13(7):839–844. doi: 10.1111/j.1540-8159.1990.tb02119.x. [DOI] [PubMed] [Google Scholar]
- Chen P. S., Pressley J. C., Tang A. S., Packer D. L., Gallagher J. J., Prystowsky E. N. New observations on atrial fibrillation before and after surgical treatment in patients with the Wolff-Parkinson-White syndrome. J Am Coll Cardiol. 1992 Apr;19(5):974–981. doi: 10.1016/0735-1097(92)90281-q. [DOI] [PubMed] [Google Scholar]
- Chen P. S., Prystowsky E. N. Role of concealed and supernormal conductions during atrial fibrillation in the preexcitation syndrome. Am J Cardiol. 1991 Nov 15;68(13):1329–1334. doi: 10.1016/0002-9149(91)90240-l. [DOI] [PubMed] [Google Scholar]
- Cox J. L., Canavan T. E., Schuessler R. B., Cain M. E., Lindsay B. D., Stone C., Smith P. K., Corr P. B., Boineau J. P. The surgical treatment of atrial fibrillation. II. Intraoperative electrophysiologic mapping and description of the electrophysiologic basis of atrial flutter and atrial fibrillation. J Thorac Cardiovasc Surg. 1991 Mar;101(3):406–426. [PubMed] [Google Scholar]
- Cranefield P. F., Hoffman B. F. Conduction of the cardiac impulse. II. Summation and inhibition. Circ Res. 1971 Feb;28(2):220–233. doi: 10.1161/01.res.28.2.220. [DOI] [PubMed] [Google Scholar]
- De la Fuente D., Sasyniuk B., Moe G. K. Conduction through a narrow isthmus in isolated canine atrial tissue. A model of the W-P-W syndrome. Circulation. 1971 Nov;44(5):803–809. doi: 10.1161/01.cir.44.5.803. [DOI] [PubMed] [Google Scholar]
- Foerster P., Müller S. C., Hess B. Critical size and curvature of wave formation in an excitable chemical medium. Proc Natl Acad Sci U S A. 1989 Sep;86(18):6831–6834. doi: 10.1073/pnas.86.18.6831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foerster P., Müller S. C., Hess B. Curvature and propagation velocity of chemical waves. Science. 1988 Aug 5;241(4866):685–687. doi: 10.1126/science.241.4866.685. [DOI] [PubMed] [Google Scholar]
- Gerhardt M., Schuster H., Tyson J. J. A cellular automation model of excitable media including curvature and dispersion. Science. 1990 Mar 30;247(4950):1563–1566. doi: 10.1126/science.2321017. [DOI] [PubMed] [Google Scholar]
- Klein G. J., Yee R., Sharma A. D. Concealed conduction in accessory atrioventricular pathways: an important determinant of the expression of arrhythmias in patients with Wolff-Parkinson-White syndrome. Circulation. 1984 Sep;70(3):402–411. doi: 10.1161/01.cir.70.3.402. [DOI] [PubMed] [Google Scholar]
- Konings K. T., Kirchhof C. J., Smeets J. R., Wellens H. J., Penn O. C., Allessie M. A. High-density mapping of electrically induced atrial fibrillation in humans. Circulation. 1994 Apr;89(4):1665–1680. doi: 10.1161/01.cir.89.4.1665. [DOI] [PubMed] [Google Scholar]
- Mendez C., Mueller W. J., Urguiaga X. Propagation of impulses across the Prukinje fiber-muscle junctions in the dog heart. Circ Res. 1970 Feb;26(2):135–150. doi: 10.1161/01.res.26.2.135. [DOI] [PubMed] [Google Scholar]
- Osaka T., Kodama I., Tsuboi N., Toyama J., Yamada K. Effects of activation sequence and anisotropic cellular geometry on the repolarization phase of action potential of dog ventricular muscles. Circulation. 1987 Jul;76(1):226–236. doi: 10.1161/01.cir.76.1.226. [DOI] [PubMed] [Google Scholar]
- Prystowsky E. N., Pritchett E. L., Gallagher J. J. Concealed conduction preventing anterograde preexcitation in Wolff-Parkinson-White syndrome. Am J Cardiol. 1984 Mar 15;53(7):960–961. doi: 10.1016/0002-9149(84)90537-x. [DOI] [PubMed] [Google Scholar]
- Sharma A. D., Klein G. J., Guiraudon G. M., Milstein S. Atrial fibrillation in patients with Wolff-Parkinson-White syndrome: incidence after surgical ablation of the accessory pathway. Circulation. 1985 Jul;72(1):161–169. doi: 10.1161/01.cir.72.1.161. [DOI] [PubMed] [Google Scholar]
- Svinarich J. T., Tai D. Y., Mickelson J., Keung E. C., Sung R. J. Electrophysiologic demonstration of concealed conduction in anomalous atrioventricular bypass tracts. J Am Coll Cardiol. 1985 Apr;5(4):898–903. doi: 10.1016/s0735-1097(85)80430-7. [DOI] [PubMed] [Google Scholar]
- Toyoshima H., Burgess M. J. Electrotonic interaction during canine ventricular repolarization. Circ Res. 1978 Sep;43(3):348–356. doi: 10.1161/01.res.43.3.348. [DOI] [PubMed] [Google Scholar]
- Wellens H. J. Atrial fibrillation--the last big hurdle in treating supraventricular tachycardia. N Engl J Med. 1994 Oct 6;331(14):944–945. doi: 10.1056/NEJM199410063311413. [DOI] [PubMed] [Google Scholar]
- Wellens H. J., Durrer D. Wolff-Parkinson-White syndrome and atrial fibrillation. Relation between refractory period of accessory pathway and ventricular rate during atrial fibrillation. Am J Cardiol. 1974 Dec;34(7):777–782. doi: 10.1016/0002-9149(74)90695-x. [DOI] [PubMed] [Google Scholar]
- Zipes D. P., DeJoseph R. L., Rothbaum D. A. Unusual properties of accessory pathways. Circulation. 1974 Jun;49(6):1200–1211. doi: 10.1161/01.cir.49.6.1200. [DOI] [PubMed] [Google Scholar]