Abstract
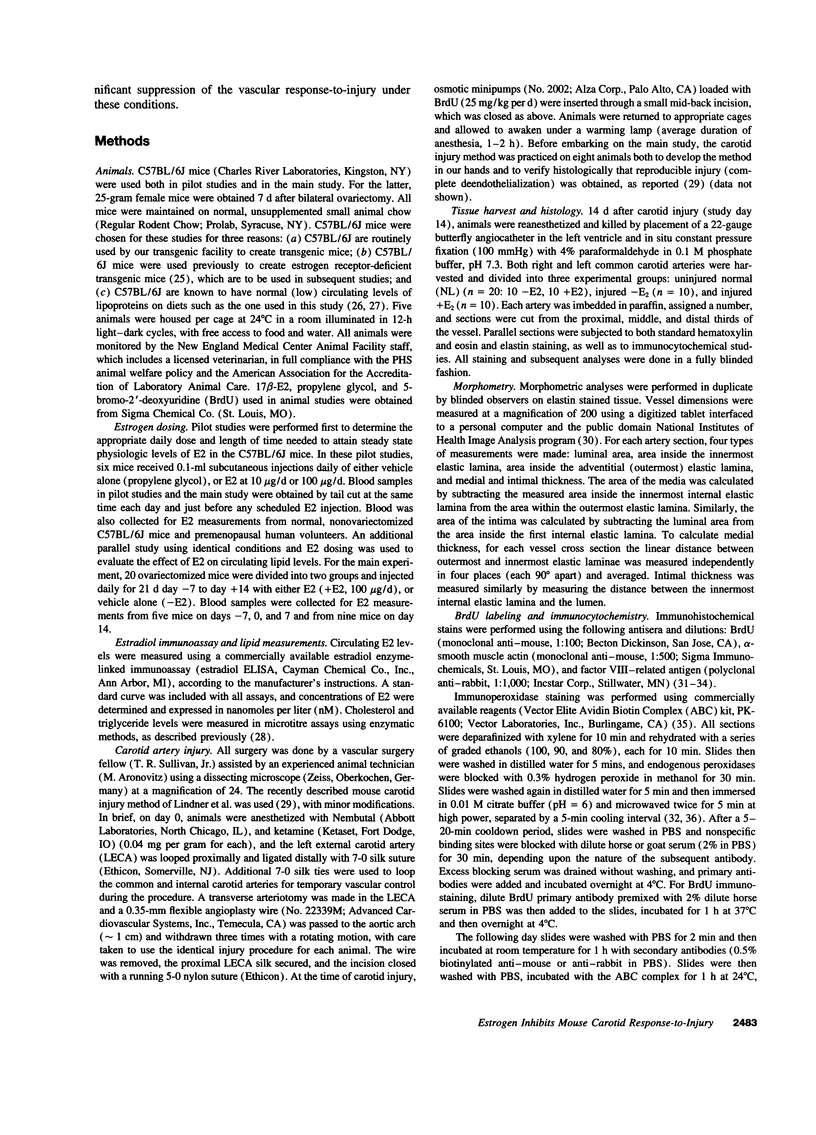
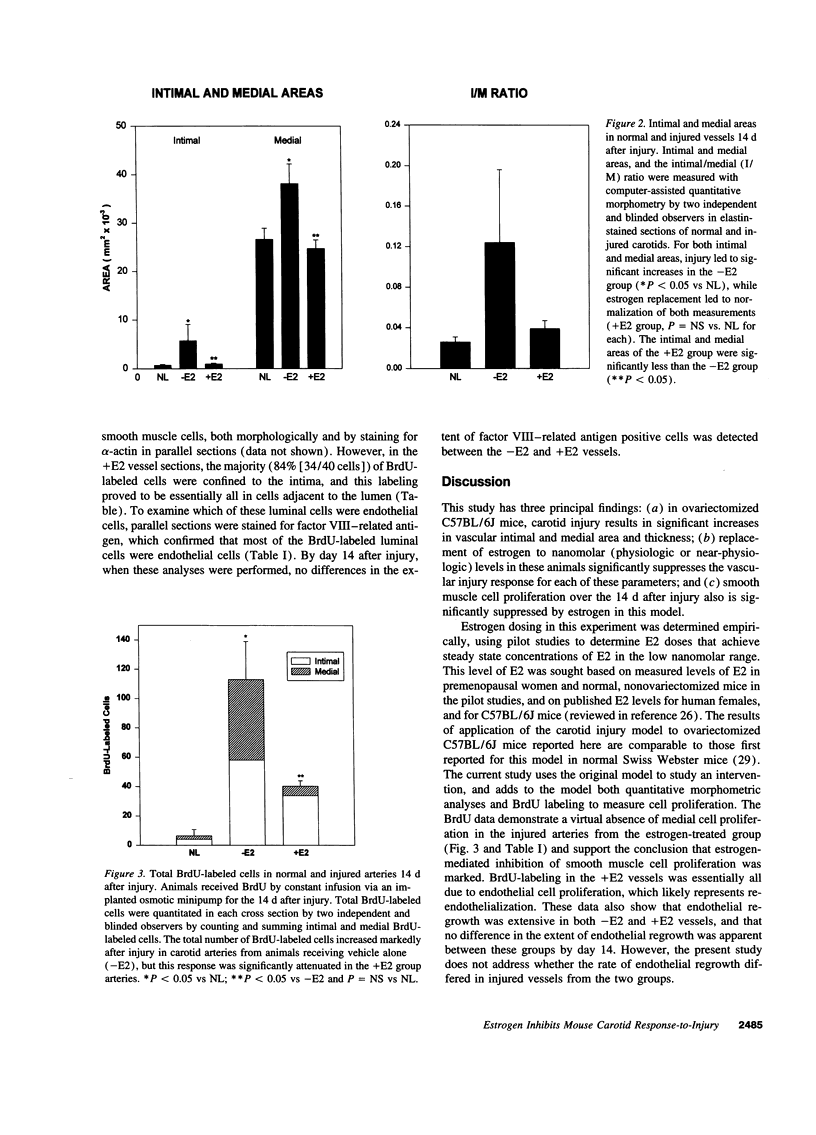
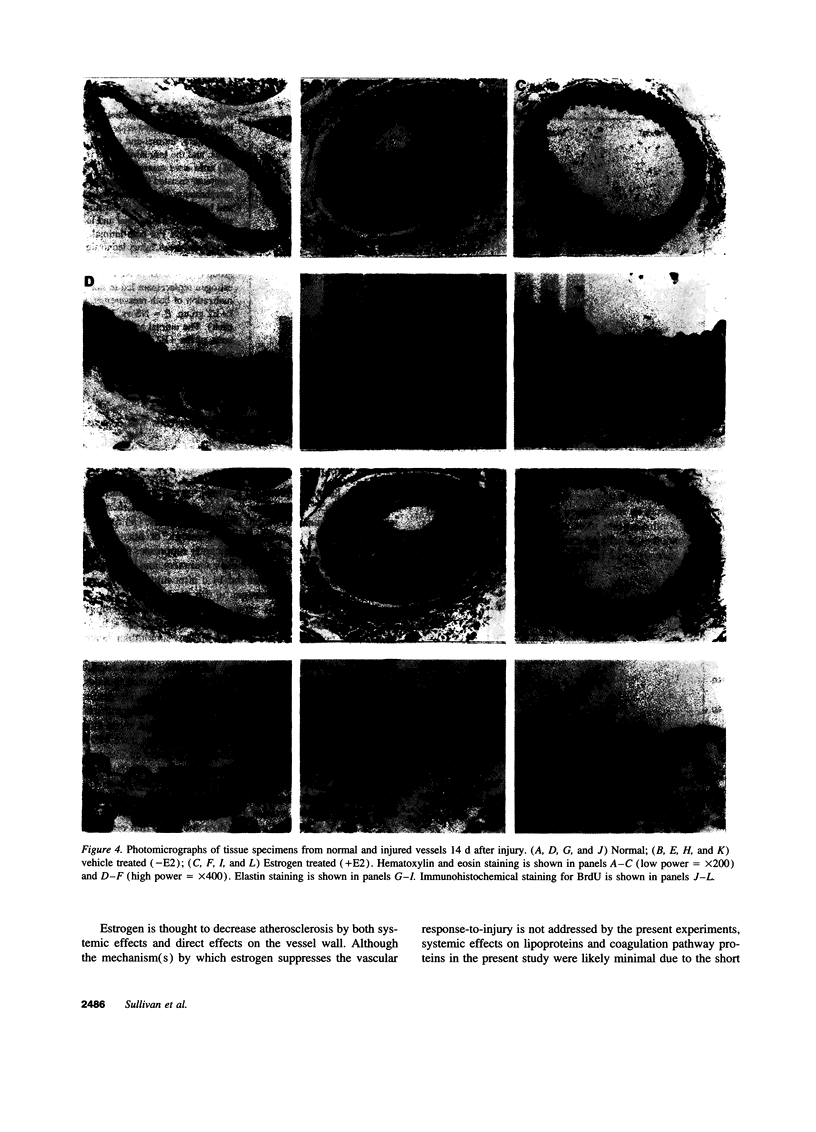
The atheroprotective effects of estrogen are well documented, but the mechanisms responsible for these effects are not well understood. To study the role of physiologic (nanomolar) estrogen levels on the arterial response-to-injury, we applied a mouse carotid artery injury model to ovariectomized C57BL/6J mice. Mice were treated with vehicle (-E2, n = 10) or 17 beta-estradiol (+E2, n = 10) for 7 d, subjected to unilateral carotid injury, and 14 d later contralateral (normal = NL) and injured carotids from -E2 and +E2 animals were pressure fixed, harvested, and analyzed by quantitative morphometry. E2 levels in +E2 mice were consistently in the nanomolar range (2.1-2.5 nM) at days 0, 7, and 14. At 14 d, measures of both intimal and medial area were markedly increased in the -E2 group: (-E2 vs NL, P < 0.05 for both), but were unchanged from normal levels in the +E2 group (+E2 vs NL, P = NS and +E2 vs -E2, P < 0.05 for both). Cellular proliferation, as assessed by bromodeoxyuridine (BrdU) labeling, was significantly increased over NL in the -E2 mice, but this increase was markedly attenuated in the estrogen replacement group (total BrdU positive cells/section: NL = 6.4 +/- 4.5; -E2 = 113 +/- 26, +E2 = 40 +/- 3.7; -E2 vs NL, P < 0.05; +E2 vs NL, P = NS; -E2 vs +E2, P < 0.05). These data (a) demonstrate significant suppression of the mouse carotid response-to-injury by physiologic levels of estrogen replacement; (b) support the utility of this model in the study of the biologic effects of estrogen on the vascular-injury response; and (c) suggest a direct effect of estrogen on vascular smooth muscle cell proliferation in injured vessels.
Full text
PDF


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aubert R., Perdereau D., Roubiscoul M., Herzog J., Lemonnier D. Genetic variations in serum lipid levels of inbred mice and response to hypercholesterolemic diet. Lipids. 1988 Jan;23(1):48–54. doi: 10.1007/BF02535304. [DOI] [PubMed] [Google Scholar]
- Barkley M. S., Geschwind I. I., Bradford G. E. The gestational pattern of estradiol, testosterone and progesterone secretion in selected strains of mice. Biol Reprod. 1979 May;20(4):733–738. doi: 10.1095/biolreprod20.4.733. [DOI] [PubMed] [Google Scholar]
- Barrett-Connor E., Bush T. L. Estrogen and coronary heart disease in women. JAMA. 1991 Apr 10;265(14):1861–1867. [PubMed] [Google Scholar]
- Bayard F., Clamens S., Meggetto F., Blaes N., Delsol G., Faye J. C. Estrogen synthesis, estrogen metabolism, and functional estrogen receptors in rat arterial smooth muscle cells in culture. Endocrinology. 1995 Apr;136(4):1523–1529. doi: 10.1210/endo.136.4.7895662. [DOI] [PubMed] [Google Scholar]
- Beldekas J. C., Smith B., Gerstenfeld L. C., Sonenshein G. E., Franzblau C. Effects of 17 beta-estradiol on the biosynthesis of collagen in cultured bovine aortic smooth muscle cells. Biochemistry. 1981 Apr 14;20(8):2162–2167. doi: 10.1021/bi00511a014. [DOI] [PubMed] [Google Scholar]
- CEMBRANO J., LILLO M., VAL J., MARDONES J. Influence of sex difference and hormones on elastine and collagen in the aorta of chickens. Circ Res. 1960 May;8:527–529. doi: 10.1161/01.res.8.3.527. [DOI] [PubMed] [Google Scholar]
- CONSTANTINIDES P., GUTMANN-AUERSPERGN, HOSPES D., WILLIAMS K. Estriol and prednisolone in rabbit atherosclerosis. Arch Pathol. 1962 Apr;73:277–280. [PubMed] [Google Scholar]
- Clarkson T. B., Anthony M. S., Klein K. P. Effects of estrogen treatment on arterial wall structure and function. Drugs. 1994;47 (Suppl 2):42–51. doi: 10.2165/00003495-199400472-00008. [DOI] [PubMed] [Google Scholar]
- Conrad K. P., Joffe G. M., Kruszyna H., Kruszyna R., Rochelle L. G., Smith R. P., Chavez J. E., Mosher M. D. Identification of increased nitric oxide biosynthesis during pregnancy in rats. FASEB J. 1993 Apr 1;7(6):566–571. [PubMed] [Google Scholar]
- Fischer-Dzoga K., Wissler R. W., Vesselinovitch D. The effect of estradiol on the proliferation of rabbit aortic medial tissue culture cells induced by hyperlipemic serum. Exp Mol Pathol. 1983 Dec;39(3):355–363. doi: 10.1016/0014-4800(83)90064-3. [DOI] [PubMed] [Google Scholar]
- Fischer G. M., Swain M. L. Effects of estradiol and progesterone on the increased synthesis of collagen in atherosclerotic rabbit aortas. Atherosclerosis. 1985 Feb;54(2):177–185. doi: 10.1016/0021-9150(85)90177-7. [DOI] [PubMed] [Google Scholar]
- Foegh M. L., Khirabadi B. S., Nakanishi T., Vargas R., Ramwell P. W. Estradiol protects against experimental cardiac transplant atherosclerosis. Transplant Proc. 1987 Aug;19(4 Suppl 5):90–95. [PubMed] [Google Scholar]
- Frazier-Jessen M. R., Kovacs E. J. Estrogen modulation of JE/monocyte chemoattractant protein-1 mRNA expression in murine macrophages. J Immunol. 1995 Feb 15;154(4):1838–1845. [PubMed] [Google Scholar]
- Gilligan D. M., Quyyumi A. A., Cannon R. O., 3rd Effects of physiological levels of estrogen on coronary vasomotor function in postmenopausal women. Circulation. 1994 Jun;89(6):2545–2551. doi: 10.1161/01.cir.89.6.2545. [DOI] [PubMed] [Google Scholar]
- Grady D., Rubin S. M., Petitti D. B., Fox C. S., Black D., Ettinger B., Ernster V. L., Cummings S. R. Hormone therapy to prevent disease and prolong life in postmenopausal women. Ann Intern Med. 1992 Dec 15;117(12):1016–1037. doi: 10.7326/0003-4819-117-12-1016. [DOI] [PubMed] [Google Scholar]
- Gratzner H. G. Monoclonal antibody to 5-bromo- and 5-iododeoxyuridine: A new reagent for detection of DNA replication. Science. 1982 Oct 29;218(4571):474–475. doi: 10.1126/science.7123245. [DOI] [PubMed] [Google Scholar]
- Gruchow H. W., Anderson A. J., Barboriak J. J., Sobocinski K. A. Postmenopausal use of estrogen and occlusion of coronary arteries. Am Heart J. 1988 May;115(5):954–963. doi: 10.1016/0002-8703(88)90063-4. [DOI] [PubMed] [Google Scholar]
- Hayashi T., Fukuto J. M., Ignarro L. J., Chaudhuri G. Basal release of nitric oxide from aortic rings is greater in female rabbits than in male rabbits: implications for atherosclerosis. Proc Natl Acad Sci U S A. 1992 Dec 1;89(23):11259–11263. doi: 10.1073/pnas.89.23.11259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horwitz K. B., Horwitz L. D. Canine vascular tissues are targets for androgens, estrogens, progestins, and glucocorticoids. J Clin Invest. 1982 Apr;69(4):750–758. doi: 10.1172/JCI110513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karas R. H., Patterson B. L., Mendelsohn M. E. Human vascular smooth muscle cells contain functional estrogen receptor. Circulation. 1994 May;89(5):1943–1950. doi: 10.1161/01.cir.89.5.1943. [DOI] [PubMed] [Google Scholar]
- Korach K. S. Insights from the study of animals lacking functional estrogen receptor. Science. 1994 Dec 2;266(5190):1524–1527. doi: 10.1126/science.7985022. [DOI] [PubMed] [Google Scholar]
- Lee P. C., Gibbons G. H., Dzau V. J. Cellular and molecular mechanisms of coronary artery restenosis. Coron Artery Dis. 1993 Mar;4(3):254–259. doi: 10.1097/00019501-199303000-00005. [DOI] [PubMed] [Google Scholar]
- Lindner V., Fingerle J., Reidy M. A. Mouse model of arterial injury. Circ Res. 1993 Nov;73(5):792–796. doi: 10.1161/01.res.73.5.792. [DOI] [PubMed] [Google Scholar]
- Losordo D. W., Kearney M., Kim E. A., Jekanowski J., Isner J. M. Variable expression of the estrogen receptor in normal and atherosclerotic coronary arteries of premenopausal women. Circulation. 1994 Apr;89(4):1501–1510. doi: 10.1161/01.cir.89.4.1501. [DOI] [PubMed] [Google Scholar]
- Lubahn D. B., Moyer J. S., Golding T. S., Couse J. F., Korach K. S., Smithies O. Alteration of reproductive function but not prenatal sexual development after insertional disruption of the mouse estrogen receptor gene. Proc Natl Acad Sci U S A. 1993 Dec 1;90(23):11162–11166. doi: 10.1073/pnas.90.23.11162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MOSKOWITZ M. S., MOSKOWITZ A. A., BRADFORD W. L., Jr, WISSLER R. W. Changes in serum lipids and coronary arteries of the rat in response to estrogens. AMA Arch Pathol. 1956 Mar;61(3):245–263. [PubMed] [Google Scholar]
- Mendelsohn M. E., Karas R. H. Estrogen and the blood vessel wall. Curr Opin Cardiol. 1994 Sep;9(5):619–626. doi: 10.1097/00001573-199409000-00018. [DOI] [PubMed] [Google Scholar]
- Morales D. E., McGowan K. A., Grant D. S., Maheshwari S., Bhartiya D., Cid M. C., Kleinman H. K., Schnaper H. W. Estrogen promotes angiogenic activity in human umbilical vein endothelial cells in vitro and in a murine model. Circulation. 1995 Feb 1;91(3):755–763. doi: 10.1161/01.cir.91.3.755. [DOI] [PubMed] [Google Scholar]
- Mukai K., Schollmeyer J. V., Rosai J. Immunohistochemical localization of actin: applications in surgical pathology. Am J Surg Pathol. 1981 Jan;5(1):91–97. doi: 10.1097/00000478-198101000-00013. [DOI] [PubMed] [Google Scholar]
- Nabulsi A. A., Folsom A. R., White A., Patsch W., Heiss G., Wu K. K., Szklo M. Association of hormone-replacement therapy with various cardiovascular risk factors in postmenopausal women. The Atherosclerosis Risk in Communities Study Investigators. N Engl J Med. 1993 Apr 15;328(15):1069–1075. doi: 10.1056/NEJM199304153281501. [DOI] [PubMed] [Google Scholar]
- Otto J., Ordovas J. M., Smith D., van Dongen D., Nicolosi R. J., Schaefer E. J. Lovastatin inhibits diet induced atherosclerosis in F1B golden Syrian hamsters. Atherosclerosis. 1995 Apr 7;114(1):19–28. doi: 10.1016/0021-9150(94)05457-t. [DOI] [PubMed] [Google Scholar]
- Reis S. E., Gloth S. T., Blumenthal R. S., Resar J. R., Zacur H. A., Gerstenblith G., Brinker J. A. Ethinyl estradiol acutely attenuates abnormal coronary vasomotor responses to acetylcholine in postmenopausal women. Circulation. 1994 Jan;89(1):52–60. doi: 10.1161/01.cir.89.1.52. [DOI] [PubMed] [Google Scholar]
- Rhee C. Y., Spaet T. H., Stemerman M. B., Lajam F., Shiang H. H., Caruso E., Litwak R. S. Estrogen suppression of surgically induced vascular intimal hyperplasia in rabbits. J Lab Clin Med. 1977 Jul;90(1):77–84. [PubMed] [Google Scholar]
- Ross R. The pathogenesis of atherosclerosis: a perspective for the 1990s. Nature. 1993 Apr 29;362(6423):801–809. doi: 10.1038/362801a0. [DOI] [PubMed] [Google Scholar]
- STAMLER J., PICK R., KATZ L. N. Prevention of coronary atherosclerosis by estrogen-androgen administration in the cholesterol-fed chick. Circ Res. 1953 Jan;1(1):94–98. doi: 10.1161/01.res.1.1.94. [DOI] [PubMed] [Google Scholar]
- Shi S. R., Key M. E., Kalra K. L. Antigen retrieval in formalin-fixed, paraffin-embedded tissues: an enhancement method for immunohistochemical staining based on microwave oven heating of tissue sections. J Histochem Cytochem. 1991 Jun;39(6):741–748. doi: 10.1177/39.6.1709656. [DOI] [PubMed] [Google Scholar]
- Stampfer M. J., Colditz G. A., Willett W. C., Manson J. E., Rosner B., Speizer F. E., Hennekens C. H. Postmenopausal estrogen therapy and cardiovascular disease. Ten-year follow-up from the nurses' health study. N Engl J Med. 1991 Sep 12;325(11):756–762. doi: 10.1056/NEJM199109123251102. [DOI] [PubMed] [Google Scholar]
- Tischler A. S. Triple immunohistochemical staining for bromodeoxyuridine and catecholamine biosynthetic enzymes using microwave antigen retrieval. J Histochem Cytochem. 1995 Jan;43(1):1–4. doi: 10.1177/43.1.7822757. [DOI] [PubMed] [Google Scholar]
- Vargas R., Wroblewska B., Rego A., Hatch J., Ramwell P. W. Oestradiol inhibits smooth muscle cell proliferation of pig coronary artery. Br J Pharmacol. 1993 Jul;109(3):612–617. doi: 10.1111/j.1476-5381.1993.tb13616.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner C. P., Lizasoain I., Baylis S. A., Knowles R. G., Charles I. G., Moncada S. Induction of calcium-dependent nitric oxide synthases by sex hormones. Proc Natl Acad Sci U S A. 1994 May 24;91(11):5212–5216. doi: 10.1073/pnas.91.11.5212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenger N. K., Speroff L., Packard B. Cardiovascular health and disease in women. N Engl J Med. 1993 Jul 22;329(4):247–256. doi: 10.1056/NEJM199307223290406. [DOI] [PubMed] [Google Scholar]
- Williams J. K., Adams M. R., Herrington D. M., Clarkson T. B. Short-term administration of estrogen and vascular responses of atherosclerotic coronary arteries. J Am Coll Cardiol. 1992 Aug;20(2):452–457. doi: 10.1016/0735-1097(92)90116-5. [DOI] [PubMed] [Google Scholar]
- Williams J. K., Adams M. R., Klopfenstein H. S. Estrogen modulates responses of atherosclerotic coronary arteries. Circulation. 1990 May;81(5):1680–1687. doi: 10.1161/01.cir.81.5.1680. [DOI] [PubMed] [Google Scholar]