Abstract
Background and aims
We followed a population based cohort of patients with inflammatory bowel disease (IBD) from Olmsted County, Minnesota, in order to analyse long term survival and cause specific mortality.
Material and methods
A total of 692 patients were followed for a median of 14 years. Standardised mortality ratios (SMRs, observed/expected deaths) were calculated for specific causes of death. Cox proportional hazards regression was used to determine if clinical variables were independently associated with mortality.
Results
Fifty six of 314 Crohn's disease patients died compared with 46.0 expected (SMR 1.2 (95% confidence interval (CI) 0.9–1.6)), and 62 of 378 ulcerative colitis (UC) patients died compared with 79.2 expected (SMR 0.8 (95% CI 0.6–1.0)). Eighteen patients with Crohn's disease (32%) died from disease related complications, and 12 patients (19%) died from causes related to UC. In Crohn's disease, an increased risk of dying from non‐malignant gastrointestinal causes (SMR 6.4 (95% CI 3.2–11.5)), gastrointestinal malignancies (SMR 4.7 (95% CI 1.7–10.2)), and chronic obstructive pulmonary disease (COPD) (SMR 3.5 (95% CI 1.3–7.5)) was observed. In UC, cardiovascular death was reduced (SMR 0.6 (95% CI 0.4–0.9)). Increased age at diagnosis and male sex were associated with mortality in both subtypes. In UC but not Crohn's disease, a diagnosis after 1980 was associated with decreased mortality.
Conclusions
In this population based study of IBD patients from North America, overall survival was similar to that expected in the US White population. Crohn's disease patients were at increased risk of dying from gastrointestinal disease and COPD whereas UC patients had a decreased risk of cardiovascular death.
Keywords: death causes, Crohn's disease, inflammatory bowel disease, ulcerative colitis, survival, mortality, prognosis
Population based data are still sparse and conflicting when it comes to long term survival in patients with inflammatory bowel disease (IBD). In Crohn's disease, a slight decrease in life expectancy has been described in studies with follow up ending in the 1970s,1,2 1980s,3,4 and 1990s.5,6,7,8 The increased mortality was associated with female sex,6 long disease duration,6 and disease location,9 and was further ascribed to an increased risk of dying from pulmonary cancer,10 genitourinary tract diseases,6 and gastrointestinal, liver, and biliary diseases.5,6,10 Three studies, however, reported normal survival in patients with Crohn's disease.9,11,12 In contrast, the majority of population based studies have shown normal or even improved survival among ulcerative colitis (UC) patients compared with the general population.8,9,13,14,15,16,17,18 These findings have been ascribed to decreased mortality from cardiovascular diseases10 and non‐gastrointestinal cancer, especially lung cancer.10 However, four Scandinavian studies4,5,19,20 reported slightly to 40% reduced survival among UC patients due to increased mortality from gastrointestinal diseases (including UC),5,19 hepatobiliary diseases,5 colorectal cancer,4,5 chronic lung diseases,4,5 pulmonary embolism,18 and suicide.18
The majority of the aforementioned studies however do not account for recent changes in the management of IBD patients, especially the introduction of new immunosuppressive medications. We therefore aimed to: (1) re‐evaluate survival in a population based IBD cohort from Olmsted County, Minnesota, after extension of the observation period by a decade to the year 2004; (2) analyse, for the first time, the cause specific mortality in IBD patients from the USA compared with the general population; and (3) determine if clinical variables were associated with mortality.
Methods
Patient cohort
Olmsted County, situated in southeastern Minnesota, had a population of 124 277 inhabitants in the 2000 US Census. The majority of people reside in Rochester, which is the urban centre of an otherwise rural county. Eighty nine per cent are non‐Hispanic White, and a substantial portion is of northern European heritage. Although 25% of county residents are employed in health care services (versus 8% nationwide), and the level of education is consequently higher (30% of adults have completed college versus 21% nationwide), the residents of Olmsted County are otherwise socioeconomically similar to the US White population.21
The study cohort comprised 692 Olmsted County residents first diagnosed with IBD (314 Crohn's disease and 378 UC) between 1940 and 2001, according to well defined criteria, as described previously.7,17,22 All patients were followed from diagnosis until emigration, death, or the end of the study (31 May 2004).
Treatment policy
During the entire observation period, patients diagnosed with IBD were followed by gastroenterologists or internists at one of two medical centres within the county. Patients underwent periodic (usually annual) evaluations, and some patients received maintenance therapy with 5‐aminosalicylates (5‐ASA). From the early 1990s, azathioprine and 6‐mercaptopurine (6‐MP) were used as alternatives to 5‐ASA. In the mid 1990s, treatment with methotrexate was introduced, and infliximab has been used as maintenance therapy in a few cases since 1999. Short term oral corticosteroid treatment has been used for episodes or worsening of symptoms, at initial doses of 30–60 mg prednisone daily that were usually tapered and discontinued over 2–3 months. Surgical resections have been performed for obstructive symptoms and for failure to respond to medical therapy. The practice of periodic colonoscopic surveillance with biopsies for UC patients with longstanding extensive colitis became widespread in the 1980s, and this practice was extended to left sided colitis and Crohn's colitis at a later date.
Follow up and registration of deaths
As medical care is practically self contained within Olmsted County and provided by the Mayo Medical Centre, the Olmsted Medical Centre, and their affiliated clinics and hospitals, it is possible to trace all IBD patients in the common medical record linkage system (Rochester Epidemiology Project).21 Complete (inpatient and outpatient) medical files in the community were reviewed to determine end of follow up due to emigration or death. For all patients who had died, death certificates were retrieved in order to register the underlying cause of death according to the International Classification of Diseases (ICD‐9), and hospital records were examined to confirm the cause and to reveal any relation to IBD.
Statistical analysis
Cumulative survival in the cohort was calculated from the date of IBD diagnosis to the last follow up using the Kaplan‐Meier product limit method, and compared with expected survival (based on mortality figures for the 1960–2000 US White background population) using the one sample log rank test. For specific causes of deaths, standardised mortality ratios (SMRs) for observed compared with expected deaths were calculated with 95% confidence intervals (CI). Expected numbers of deaths were calculated according to person years at risk in the cohort and age and sex matched cause of death figures from the US White population (1960–2000). SMR analysis was stratified by age at IBD diagnosis (0–18 years, 19–29 years, 30–49 years, ⩾50 years), calendar period of IBD diagnosis (1940–1959, 1960–1979, 1980–2001), and by immunosuppressive/biological medication usage (any use of azathioprine, 6‐MP, methotrexate, or infliximab versus none). Confidence intervals excluding 1.0 were considered statistically significant (p<0.05). To determine if age at diagnosis (five year increments), sex, calendar period of diagnosis, or maximal disease extent were independent predictors of mortality, we used Cox proportional hazards regression analysis for each subtype of IBD, using time to death as the dependent variable. These results were expressed as hazards ratios (HR) with their 95% CI.
Results
A total of 692 Olmsted County residents with IBD were observed for a total of 11 307 person years, with a median follow up time of 14 years (range 7 days–58 years). Crohn's disease patients (159 women and 155 men) contributed 4946 person years of observational time and were followed for a median of 13 years (range 7 days–54 years). The maximal extent of Crohn's disease involvement was small bowel in 91 patients (29%), colonic in 93 (30%), and ileocolonic in 130 (41%). Among 21 Crohn's disease patients diagnosed between 1940 and 1959, none received immunosuppressives or biological agents during their clinical course, while 13 of 116 patients (11%) diagnosed between 1960 and 1979 and 65 of 177 patients (37%) diagnosed between 1980 and 2001 received one of these agents at some point in their clinical course. UC patients (166 women and 212 men) were followed for 6360 person years, or a median of 15 years (range 25 days–58 years). The maximal extent of UC involvement was proctitis in 64 patients (17%), left sided colitis in 134 (35%), and extensive in 179 (47%). (The extent was unknown in one UC patient.) None of the 34 UC patients diagnosed between 1940 and 1959 received immunosuppressive agents or biological agents during their clinical course, while five of 143 patients (3%) diagnosed between 1960 and 1979 and 41 of 201 patients (20%) diagnosed between 1980 and 2001 received at least one of these agents. The relationship between subtype of IBD, age, sex, and calendar year at diagnosis is shown in table 1.
Table 1 Demographic characteristics of Olmsted County, Minnesota, residents diagnosed with inflammatory bowel disease during 1940–2001.
| Calendar period at diagnosis | Crohn's disease | Ulcerative colitis | ||||||
|---|---|---|---|---|---|---|---|---|
| All patients | Women | Men | Median age at diagnosis (y) | All patients | Women | Men | Median age at diagnosis (y) | |
| 1940–1949 | 9 | 3 | 6 | 42.8 | 12 | 7 | 5 | 47.1 |
| 1950–1959 | 12 | 8 | 4 | 38.6 | 22 | 13 | 9 | 35.5 |
| 1960–1969 | 44 | 23 | 21 | 28.1 | 61 | 25 | 36 | 31.2 |
| 1970–1979 | 72 | 44 | 28 | 26.0 | 82 | 39 | 43 | 30.9 |
| 1980–1989 | 72 | 32 | 40 | 27.8 | 85 | 31 | 54 | 32.5 |
| 1990–2001 | 105 | 49 | 56 | 34.0 | 116 | 51 | 65 | 35.2 |
| All years | 314 | 159 | 155 | 28.9 | 378 | 166 | 212 | 33.3 |
Overall survival
Crohn's disease
Among 314 patients with Crohn's disease, 56 deaths were observed compared with 46.0 expected (SMR 1.2 (95% CI 0.9–1.6)). Twenty six women died compared with 22.1 expected (SMR 1.2 (95% CI 0.8–1.7)) and 30 men compared with 23.9 expected (SMR 1.3 (95% CI 0.9–1.8)). Median age at death was 79 years (range 34–95) in women and 70 years (range 29–93) in men.
When SMR values for Crohn's disease were stratified by age at diagnosis, there did not appear to be any significant differences. SMR for Crohn's disease patients aged 0–18 years at diagnosis was 1.1 (95% CI 0.03–6.4), 1.1 (95% CI 0.4–2.6) for patients aged 19–29 years, 1.3 (95% CI 0.8–2.0) for patients aged 30–49 years, and 1.2 (95% CI 0.8–1.7) for those ⩾50 years old at diagnosis. Similarly, the risk of dying was not significantly associated with calendar year at diagnosis: SMR for Crohn's disease patients diagnosed between 1940 and 1959 was 0.9 (95% CI 0.5–1.5), 1.4 (95% CI 0.9–2.1) for those diagnosed between 1960 and 1979, 1.7 (95% CI 0.8–3.2) for patients diagnosed between 1980 and 1989, and 1.2 (95% CI 0.5–2.3) for patients diagnosed between 1990 and 2001 (p⩾0.19 when comparing any two of four time periods). Among 78 Crohn's disease patients who had record of use of 6‐MP, azathioprine, methotrexate, or infliximab, there were four deaths versus 4.29 expected (SMR 0.9 (95% CI 0.3–2.4)). Among the 236 patients with no record of use of these medications, 52 patients died versus 41.71 expected (SMR 1.3 (95% CI 0.9–1.6)).
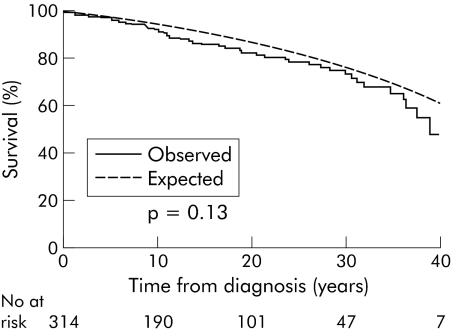
Cumulative survival among Crohn's disease patients after 10 years was 91% (95% CI 88–95%)) versus 94% expected, 82% (95% CI 77–87%) versus 86% expected after 20 years, 73% (95% CI 65–81%) versus 74% expected after 30 years, and 48% (95% CI 30–65%) versus 61% expected after 40 years (fig 1). Thus there was a suggestion of decreased survival in Crohn's disease patients but the reduction was not statistically significant (one sample log rank test, p = 0.13).
Figure 1 Observed and expected cumulative survival from time of diagnosis in 314 Olmsted County, Minnesota, residents with Crohn's disease diagnosed in 1940–2004 (log rank, p = 0.13).
Ulcerative colitis
A total of 62 deaths occurred in 378 UC patients, compared with 79.2 expected (SMR 0.8 (95% CI 0.6–1.0)). Twenty six women died versus 36.3 expected (SMR 0.7 (95% CI 0.5–1.1)), and 36 men died versus 42.9 expected (SMR 0.8 (95% CI 0.6–1.2)). Median age at death was 81 years (range 38–97) in women and 71 years (range 26–92) in men.
Observed mortality was less than expected in all age strata but this was not as prominent among patients aged ⩾50 years at diagnosis. None of the patients aged 0–18 years at UC diagnosis died versus 1.01 expected (SMR 0 (95% CI 0–3.6)) while three patients aged 19–29 years died versus 7.23 expected (SMR 0.4 (95% CI 0.1–1.2)). Fourteen patients aged 30–49 years at diagnosis died versus 22.2 expected (SMR 0.6 (95% CI 0.3–1.0)), and 45 patients aged ⩾50 years died versus 48.3 expected (SMR 0.9 (95% CI 0.7–1.3)). When stratified by calendar year at diagnosis, survival appeared to improve over time. SMR was 0.8 (95% CI 0.5–1.3) for UC patients diagnosed between 1940 and 1959, 0.9 (95% CI 0.6–1.2) for those diagnosed between 1960 and 1979, 0.7 (95% CI 0.3–1.3) for patients diagnosed between 1980 and 1989, and 0.5 (95% CI 0.1–1.3) for those diagnosed between 1990 and 2001. Yet there were no statistically significant differences between any two of the four period specific SMRs (p⩾0.19 for all six comparisons). Among 46 patients who had received 6‐MP, azathioprine, methotrexate, or infliximab, there were three deaths versus 2.28 expected (SMR 1.3 (95% CI 0.3–3.8)). Among 332 UC patients who did not receive these medications, 59 died versus 76.88 expected (SMR 0.8 (95% CI 0.6–0.99)).
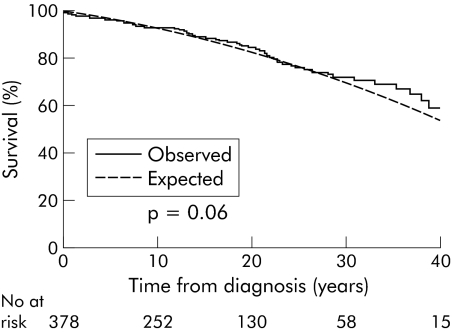
In contrast with Crohn's disease, UC patients had a slightly better cumulative survival than expected (fig 2): 93% (95% CI 91–96%) versus 92% expected after 10 years, 85% (95% CI 80–89%) versus 82% expected after 20 years, 72% (95% CI 65–79%) versus 68% expected after 30 years, and 59% (95% CI 48–70%) versus 53% expected after 40 years (one sample log rank test, p = 0.06).
Figure 2 Observed and expected cumulative survival from time of diagnosis in 378 Olmsted County, Minnesota, residents with ulcerative colitis diagnosed in 1940–2004 (log rank, p = 0.06).
Inflammatory bowel disease specific mortality
Crohn's disease
A total of 18 deaths (32%) among patients with Crohn's disease were definitely or possibly related to the underlying disease (table 2). Eight (44%) were women. Median age at Crohn's disease diagnosis for these patients was 40.5 years (range 13–77), and median age at death was 54.5 years (range 17–77). Seven patients died from causes related to severe fistulising Crohn's disease (that is, intra‐abdominal abscesses, peritonitis, and short bowel syndrome after surgery for internal fistulae). One patient, a 35 year old woman recently treated with infliximab, died of sepsis after surgery for an internal fistula. In three patients, death was related to primary sclerosing cholangitis (PSC), as two died from end stage liver disease due to PSC and one died from cholangiocarcinoma of the hepatic bile ducts and concurrent haemorrhagic pancreatitis. Whether the disease phenotype in these three patients, described as ileocolonic Crohn's disease, could in some cases have been UC with backwash ileitis is uncertain. Six patients (three women and three men) died from intestinal cancer, thus accounting for 10% of all deaths in Crohn's disease patients.
Table 2 Clinical characteristics of 18 patients with a cause of death related to Crohn's disease: a population based study, Olmsted County, Minnesota, 1940–2004.
| Cause of death | Sex | Maximal extent of CD | Calendar year at diagnosis | Age at diagnosis (y) | Age at death (y) | Disease duration (y) | |
|---|---|---|---|---|---|---|---|
| Complications of Crohn's disease | |||||||
| Severe disease, fistulas, perforation, sepsis | |||||||
| 1 | Intra‐abdominal abscess, peritonitis | F | Colonic | 1972 | 53 | 53 | <1 |
| 2 | Sepsis after surgery for internal fistula, recent infliximab treatment | F | Ileocolonic | 1990 | 25 | 35 | 10 |
| 3 | Severe CD, sepsis | M | Colonic | 1943 | 56 | 56 | <1 |
| 4 | Severe CD, ileum perforation, peritonitis | M | Ileocolonic | 1949 | 56 | 62 | 6 |
| 5 | Severe fistulising CD, sepsis | M | Colonic | 1965 | 77 | 77 | <1 |
| 6 | Severe fistulising CD, peritonitis, MI | M | Ileocolonic | 1973 | 47 | 48 | 1 |
| Short bowel syndrome | |||||||
| 7 | Short bowel syndrome after surgery for internal fistulas, COPD | F | Ileocolonic | 1976 | 52 | 71 | 19 |
| 8 | Short bowel syndrome, intestinal ischemia | M | Ileocolonic | 1962 | 42 | 61 | 19 |
| PSC and cholagiocarcinoma | |||||||
| 9 | End stage liver disease due to PSC | F | Ileocolonic | 1980 | 35 | 46 | 11 |
| 10 | End stage liver disease due to PSC | M | Colonic | 1987 | 39 | 49 | 10 |
| 11 | Cholangiocarcinoma of hepatic bile ducts and hemorrhagic pancreatitis | M | Ileocolonic | 1954 | 30 | 62 | 32 |
| Embolism | |||||||
| 12 | Steroid refractory CD, pulmonary embolism | F | Ileocolonic | 1972 | 43 | 57 | 14 |
| Median (range) | 43 (15–77) | 56 (17–77) | 11 (1–32) | ||||
| Intestinal cancer | |||||||
| 1 | Metastatic leiomyosarcoma of small bowel | F | Ileocolonic | 1951 | 32 | 63 | 31 |
| 2 | Metastatic ileocaecal adenocarcinoma | F | Ileocolonic | 1978 | 25 | 34 | 9 |
| 3 | Metastatic colorectal cancer | F | Colonic | 1969 | 30 | 43 | 13 |
| 4 | Small bowel lymphoma | M | Jejunal, ileocolonic | 1967 | 23 | 47 | 24 |
| 5 | Metastatic colorectal cancer | M | Jejunum, ileocolonic | 1962 | 13 | 30 | 17 |
| 6 | Metastatic colorectal cancer | M | Ileal | 1987 | 69 | 70 | 1 |
| Median (range) | 28 (13–69) | 45 (30–70) | 15 (1–31) | ||||
CD, Crohn's disease; COPD, chronic obstructive pulmonary disease; PSC, primary sclerosing cholangitis; F, female; M, male; MI, acute myocardial infarction.
Ulcerative colitis
Among patients with UC, 12 deaths (19%) could be ascribed to the underlying disease (table 3). These 12 patients (25% women) had a median age at diagnosis of 47 years (range 26–87) and a median age at death of 62.5 years (26–91). Seven patients died from severe UC, in most cases pancolitis, with complications such as perforation, intestinal haemorrhage, and postoperative acute myocardial infarction or sepsis. Only one patient (2% of all deaths in UC patients) died from end stage liver disease due to PSC. Lastly, five patients died from metastatic colorectal cancer, causing 8% of all deaths in patients with UC.
Table 3 Clinical characteristics of 12 patients with a cause of death related to ulcerative colitis: a population based study, Olmsted County, Minnesota, 1940–2004.
| Sex | Maximal extent of UC | Calendar year at diagnosis | Age at diagnosis (y) | Age at death (y) | Disease duration (y) | ||
|---|---|---|---|---|---|---|---|
| Complications of ulcerative colitis | |||||||
| 1 | Severe UC, intestinal haemorrhage | F | Left sided | 1957 | 87 | 91 | 4 |
| 2 | Severe UC, postoperative MI | F | Extensive | 1969 | 67 | 67 | <1 |
| 3 | Severe UC, perforation, peritonitis | M | Extensive | 1942 | 26 | 26 | <1 |
| 4 | Severe UC, postoperative sepsis | M | Extensive | 1956 | 58 | 71 | 13 |
| 5 | Severe UC, ileus | M | Left sided | 1962 | 75 | 83 | 8 |
| 6 | Severe UC, anaemia, MI | M | Left sided | 1980 | 69 | 75 | 6 |
| 7 | UC, PSC, portal hypertension | M | Extensive | 1972 | 36 | 45 | 9 |
| Median (range) | 67 (26–87) | 71 (26–91) | 8 (1–13) | ||||
| Colorectal cancer | |||||||
| 1 | Metastatic colorectal cancer | F | Extensive | 1949 | 37 | 38 | 1 |
| 2 | Metastatic colorectal cancer | M | Extensive | 1960 | 34 | 46 | 12 |
| 3 | Metastatic colorectal cancer | M | Left sided | 1964 | 57 | 58 | 1 |
| 4 | Metastatic colorectal cancer | M | Extensive | 1966 | 29 | 67 | 37 |
| 5 | Metastatic colorectal cancer | M | Extensive | 1973 | 32 | 53 | 21 |
| Median (range) | 34 (30–57) | 53 (38–67) | 12 (1–37) | ||||
MI, acute myocardial infarction; UC, ulcerative colitis; PSC, primary sclerosing cholangitis.
Cause specific mortality
Crohn's disease
The slightly increased mortality from Crohn's disease could be explained by an increased risk of dying from gastrointestinal disease and cancer, primarily due to the Crohn's disease related deaths described above (table 4). In 11 patients, death was classified as due to gastrointestinal disease (ICD‐9 codes 520–579) compared with 1.7 expected (SMR 6.4 (95% CI 3.2–12)). In six patients, the cause of death was classified as gastrointestinal malignancy (ICD‐9 codes 152–154) versus 1.3 expected (SMR 4.7 (95% CI 1.7–10)). No significant difference in risk was observed when stratifying by sex.
Table 4 Causes of death among 56 patients with Crohn's disease: a population based study, Olmsted County, Minnesota, 1940–2004.
| Causes of death (ICD‐9) | Women | Men | ||||||
|---|---|---|---|---|---|---|---|---|
| Observed deaths | Expected deaths | SMR | 95% CI | Observed deaths | Expected deaths | SMR | 95% CI | |
| Infections (001–139) | 0 | 0.3 | 0.0 | 0.0–12 | 1 | 0.6 | 1.7 | <0.1–9.6 |
| Cancer (140–239) | 6 | 5.3 | 1.1 | 0.4–2.5 | 10 | 5.7 | 1.8 | 0.8–3.2 |
| Intestinal cancer (152–154) | 3 | 0.6 | 4.7 | 1.0–14 | 3 | 0.6 | 4.7 | 1.0–14 |
| Pancreas cancer (157) | 1 | 0.3 | 3.8 | 0.1–21 | 1 | 0.3 | 3.9 | 0.1–22 |
| Pulmonary cancer (162) | 0 | 1.0 | 0.0 | 0.0–3.6 | 3 | 2.0 | 1.5 | 0.3–4.4 |
| Malignant melanoma (172) | 1 | 0.1 | 14.8 | 0.4–82 | 1 | 0.1 | 9.6 | 0.2–53 |
| Leukaemia (204–208) | 0 | 0.2 | 0.0 | 0.0–20 | 0 | 0.2 | 0.0 | 0.0–18 |
| Diseases of blood and blood forming organs (280–289) | 0 | 0.1 | 0.0 | 0.0–41 | 0 | 0.1 | 0.0 | 0.0–47 |
| Nervous system (320–359) | 0 | 0.4 | 0.0 | 0.0–9.1 | 0 | 0.4 | 0.0 | 0.0–9.8 |
| Diseases of the circulatory system (390–459) | 11 | 10.8 | 1.0 | 0.5–1.8 | 8 | 10.4 | 0.8 | 0.3–1.5 |
| Respiratory diseases (460–519) | 3 | 1.8 | 1.7 | 0.4–5.0 | 4 | 2.0 | 2.0 | 0.5–5.1 |
| Pneumonia (485) | 0 | 0.8 | 0.0 | 0.0–4.6 | 1 | 0.7 | 1.5 | <0.1–8.1 |
| COPD (490–496) | 3 | 0.7 | 4.3 | 0.9–13 | 3 | 1.0 | 2.9 | 0.6–8.5 |
| Gastrointestinal and liver diseases (520–579) | 6 | 0.8 | 7.3 | 2.7–16* | 5 | 0.9 | 5.6 | 1.8–13* |
| Genitourinary tract diseases (580–629) | 0 | 0.4 | 0.0 | 0.0–8.4 | 1 | 0.4 | 2.9 | 0.1–16 |
| Suicide (950–959) | 0 | 0.2 | 0.0 | 0.0–18 | 0 | 0.6 | 0.0 | 0.0–5.8 |
| Accidents (800–949) | 0 | 0.7 | 0.0 | 0.0–5.5 | 1 | 1.4 | 0.7 | <0.1–4.1 |
| All other causes | 0 | 1.4 | 0.0 | 0.0–2.6 | 0 | 1.4 | 0.0 | 0.0–2.7 |
| Total | 26 | 22.1 | 1.2 | 0.8–1.7 | 30 | 23.9 | 1.3 | 0.9–1.8 |
*95% confidence interval excluding 1.0 (p<0.05).
COPD, chronic obstructive pulmonary disease; SMR, standardised mortality ratio.
Patients with Crohn's disease were also at increased risk of dying from COPD (ICD‐9 codes 490–496), as six patients died versus 1.7 expected (SMR 3.5 (95% CI 1.3–7.5)). Notably, no patient died from leukaemia (0.4 deaths expected) and only one patient died in 1991 from lymphoma, which was located in the small intestine and classified as an intestinal malignancy.
Ulcerative colitis
In UC patients, cause specific mortality was not significantly increased in any subcategory (table 5). Despite the 12 deaths ascribed to UC, the risk of dying from gastrointestinal diseases (SMR 2.0 (95% CI 0.8–4.4)) or gastrointestinal cancer (SMR 2.2 (95% CI 0.7–5.2)) was not significantly increased.
Table 5 Causes of death among 62 patients with ulcerative colitis: a population based study, Olmsted County, Minnesota, 1940–2004.
| Causes of deaths (ICD‐9) | Women | Men | ||||||
|---|---|---|---|---|---|---|---|---|
| Observed deaths | Expected deaths | SMR | 95% CI | Observed deaths | Expected deaths | SMR | 95% CI | |
| Infections (001–139) | 0 | 0.5 | 0.0 | 0.0–7.4 | 0 | 0.9 | 0.0 | 0.0–4.0 |
| Cancer (140–239) | 5 | 8.2 | 0.6 | 0.2–1.4 | 10 | 11.0 | 0.9 | 0.4–1.7 |
| Intestinal cancer (152–154) | 1 | 1.0 | 1.0 | <0.1–5.3 | 4 | 1.2 | 3.3 | 0.9–8.4 |
| Pancreas cancer (157) | 1 | 0.4 | 2.3 | 0.1–13 | 0 | 0.5 | 0.0 | 0.0–7.4 |
| Pulmonary cancer (162) | 0 | 1.6 | 0.0 | 0.0–2.4 | 2 | 3.9 | 0.5 | 0.1–1.9 |
| Malignant melanoma (172) | 0 | 0.1 | 0.0 | 0.0–40 | 0 | 0.2 | 0.0 | 0.0–20 |
| Leukaemia (204–208) | 0 | 0.3 | 0.0 | 0.0–13 | 2 | 0.4 | 5.2 | 0.6–19 |
| Diseases of blood and blood‐forming organs (280–289) | 0 | 0.1 | 0.0 | 0.0–26 | 1 | 0.1 | 7.1 | 0.2–39 |
| Nervous system (320–359) | 2 | 0.7 | 3.1 | 0.4–11 | 1 | 0.7 | 1.5 | <0.1–8.3 |
| Diseases of the circulatory system (390–459) | 8 | 18.1 | 0.4 | 0.2–0.9* | 15 | 18.9 | 0.8 | 0.4–1.3 |
| Respiratory diseases (460–519) | 4 | 2.9 | 1.4 | 0.4–3.5 | 2 | 3.6 | 0.6 | 0.1–2.0 |
| Pneumonia (485) | 3 | 1.3 | 2.2 | 0.5–6.5 | 0 | 1.1 | 0.0 | 0.0–3.2 |
| COPD (490–496) | 0 | 1.2 | 0.0 | 0.0–3.2 | 2 | 2.0 | 1.0 | 0.1–3.7 |
| Gastrointestinal and liver diseases (520–579) | 2 | 1.3 | 1.5 | 0.2–5.5 | 4 | 1.7 | 2.4 | 0.7–6.2 |
| Genitourinary tract diseases (580–629) | 2 | 0.7 | 2.7 | 0.3–10 | 0 | 0.6 | 0.0 | 0.0–6.1 |
| Suicide (950–959) | 0 | 0.2 | 0.0 | 0.0–16 | 1 | 1.0 | 1.0 | <0.1–5.6 |
| Accidents (800–949) | 1 | 0.9 | 1.2 | <0.1–6.5 | 1 | 2.0 | 0.5 | <0.1–2.8 |
| All other causes | 2 | 2.2 | 0.9 | 0.1–3.4 | 1 | 2.3 | 0.4 | 0.1–2.4 |
| Total | 26 | 36.3 | 0.7 | 0.5–1.1 | 36 | 42.9 | 0.8 | 0.6–1.2 |
*95% confidence interval excluding 1.0 (p<0.05).
SMR standardised mortality ratio; COPD, chronic obstructive pulmonary disease.
In contrast with this, a decreased risk of dying from cardiovascular diseases (ICD‐9 codes 390–459) was observed among all UC patients (SMR 0.6 (95% CI 0.4–0.9)) and in women in particular (SMR 0.4 (95% CI 0.2–0.9)). Two patients (both males) with UC died from leukaemia versus 0.7 expected (SMR 3.0 (95% CI 0.4–11)). One died in 1971 from acute myelomonocytic leukaemia with disseminated intravascular coagulation, and one who had coexistent PSC died in 1992 from chronic lymphatic leukaemia. No patients died from lymphoma.
Cox proportional hazards regression
For Crohn's disease, age was independently associated with mortality (HR 1.6 per five year increment (95% CI 1.4–1.7)). There was a trend for male sex to be associated with mortality (HR 1.7) but this did not quite meet statistical significance (95% CI 0.98–3.1). Using patients diagnosed between 1940 and 1959 as the reference, being diagnosed in 1960–79 (HR 1.6 (95% CI 0.7–3.4)) or 1980–2001 (HR 1.1 (95% CI 0.5–2.8)) were not independently associated with mortality. Using patients with colonic involvement only as the reference group, having isolated small bowel involvement (HR 0.8 (95% CI 0.4–1.6)) or ileocolonic involvement (HR 0.8 (95% CI 0.4–1.7)) were also not significantly associated with mortality.
For UC, both age (HR 1.7 per five year increment (95% CI 1.5–1.9)) and male sex (HR 2.0 (95% CI 1.2–3.4)) were independently associated with mortality. Using patients diagnosed in the 1940–1959 period as the reference group, being diagnosed in the 1960–79 period was not independently associated with mortality (HR 0.6 (95% CI 0.3–1.1)), but being diagnosed in the 1980–2002 period was significantly associated with decreased mortality (HR 0.2 (95% CI 0.1–0.6)). Using ulcerative proctitis patients as the reference group, having left sided colitis was not significantly associated with mortality (HR 0.9 (95% CI 0.4–2.3)) while having extensive colitis was associated with mortality (HR 2.2) although this did not quite meet statistical significance (95% CI 0.9–5.1).
Discussion
The present long term follow up study of a population based inception cohort of patients with IBD from the USA revealed an almost unchanged pattern of survival during the past six decades. In Crohn's disease, overall mortality was slightly increased due to deaths from gastrointestinal disease and gastrointestinal malignancies. In contrast, overall survival in UC was slightly greater than expected due to decreased mortality from cardiovascular diseases. No increased risk of dying from leukaemia or lymphomas was observed. Multiple variable analysis suggested that older age at diagnosis and male sex were associated with mortality. Being diagnosed with UC after 1980 was associated with decreased mortality in multiple variable analysis, but the same was not seen for Crohn's disease.
All patients derived from a well defined geographic region, Olmsted County, and were included in the cohort according to strict international diagnostic criteria.7,17,22 All death certificates were retrieved, and the causes of death were verified in the regional medical record linkage system (the Rochester Epidemiology Project), which provides access to all local medical records and assures a high level of clinical detail. However, the relatively small number of patients and low frequency of events observed in the present study may veil differences in risk estimates in subsets of patients. It can also be questioned whether Olmsted County is representative of the general US population due to the relatively high percentage of Whites in the region studied and their somewhat greater education level.
In the present study, we observed a trend towards decreased survival among patients with Crohn's disease compared with an age and sex matched background population, and 32% of deaths were ascribed to the underlying disease, similar to the percentage observed in Copenhagen County, Denmark.6 Crohn's disease related deaths resulted in an excess risk of dying from gastrointestinal disease and cancer, as observed also in Italy and Scandinavia.5,6,10 Although the majority of Crohn's disease related deaths occurred in patients diagnosed before the 1990s, overall survival remained unchanged during the following decade of observation. One may speculate that introduction of new treatment strategies has improved survival from Crohn's disease itself, but has led to an increased risk of dying from other causes (long term adverse events). When we directly compared relative mortality between patients who received immunosuppressive agents and those who did not, we could see no significant differences. In a retrospective, non‐randomised study, however, any potential benefit of these agents could have been masked by the fact that patients with more severe disease were receiving them. In the present study, the death of one patient had a possible relation to anti‐tumour necrosis factor α treatment, but no patient died from opportunistic infection or lymphoma due to treatment with these drugs. For comparison, a recent population based study from Stockholm County, Sweden, suggested an increased mortality in IBD patients treated with infliximab due to fatal adverse events such as lymphomas, opportunistic infections, and postoperative complications, but the expected number of deaths from an age and sex matched background population or non‐infliximab treated IBD population were lacking.23 A preliminary report from the TREAT registry (a registry maintained by Ovation Research and funded by Centocor Inc.) suggested that an increased risk of serious infections and death in Crohn's disease patients is attributable to treatment with prednisone rather than infliximab.24 Future prospective population based studies are required to evaluate the long term effect of treatment with new biological modifiers on survival in Crohn's disease patients.
Furthermore, an increased risk of dying from COPD was observed in patients with Crohn's disease, which is in accordance with the high frequency of smokers among Crohn's disease patients compared with unaffected individuals.25 Thus as disease activity and chronic lung disease are the major contributors to mortality in this patient group, and since they are both related to the use of tobacco, it is essential not only to encourage Crohn's disease patients to quit smoking but also to provide relevant assistance to overcome the dependency.
In UC patients from Olmsted County, overall survival was not affected, in accordance with several population based studies from Europe.8,9,13,14,15,16,18 Indeed, survival even seemed to improve slightly over the six decades of observation. Thus the initially reported poor prognosis in UC26 is again not confirmed, leading one to conclude that UC patients should not be denied access to reasonably priced medical and life insurance policies. The 19% of deaths which had a certain or possible relation to UC were counterbalanced by a decreased risk of dying from cardiovascular diseases. This is in accordance with an older study from the UK26 and a recent study from Italy,10 and is possibly explained by the low frequency of cigarette smoking among UC patients combined with a lower systolic and diastolic blood pressure in UC patients compared with controls (probably due to sodium and water depletion in patients with extensive colitis or ileostomy).27 Interestingly, only 8% of deaths among UC patients were caused by colorectal cancer (CRC) in contrast with the one sixth cited in a recent meta‐analysis of CRC in selected and unselected UC cohorts.28 The low cancer mortality in UC is in accordance with the findings of a recent population based study from Copenhagen,18 and is of important prognostic value. We recently described the low incidence of CRC among Olmsted County residents with IBD.29 The relative risk of CRC in UC was 1.1, and the cumulative incidence of CRC after 25 years of disease was only 2%. In Crohn's disease, the relative risk of CRC was 1.9, but not significantly different from that expected, and the cumulative risk of CRC was 2.4% after 25 years of disease. Perhaps a combination of surveillance colonoscopy, proctocolectomy (25 year cumulative risks of 20.8% and 10.4% for UC and Crohn's disease, respectively), and more widespread use of 5‐ASA derivates have led to this apparent decline in CRC incidence. Future studies should address the influence of strict treatment policies, surgical interventions, and close follow up of UC patients on low CRC incidence and mortality.
In conclusion, this population based study of IBD patients from North America revealed a relatively stable survival pattern during the past six decades. Cause specific mortality seemed related to differences in smoking habits, as increased mortality from gastrointestinal diseases and COPD was observed in Crohn's disease whereas decreased mortality from cardiovascular disease was observed in UC. An active and structured approach to Crohn's disease patients regarding cessation of smoking is required.
Acknowledgements
Supported in part by the Mayo Foundation for Medical Education and Research and AR30582 from the National Institutes of Health. Dr Tine Jess' stay at the Mayo Clinic was supported by the Astra Zeneca Travel Foundation, Augustinus Foundation, Beckett Foundation, Danish Crohn Colitis Foundation, Jacob Madsen and Olga Madsen Foundation, and Sigrid R. Moran Foundation.
Abbreviations
COPD - chronic obstructive pulmonary disease
HR - hazards ratio
IBD - inflammatory bowel disease
6‐MP - 6‐mercaptopurine
SMR - standardised mortality ratio
UC - ulcerative colitis
5‐ASA - 5‐aminosalicylic acid
PSC - primary sclerosing cholangitis
CRC - colorectal cancer
Footnotes
Conflict of interest: None declared.
Presented in part at the 106th Annual Meeting of the American Gastroenterological Association, Chicago, Illinois, USA, May 14–19, 2005 (Gastroenterology 2005;128(suppl 2):A321).
References
- 1.Prior P, Gyde S, Cooke W T.et al Mortality in Crohn's disease. Gastroenterology 198180307–312. [PubMed] [Google Scholar]
- 2.Weedon D D, Shorter R G, Ilstrup D M.et al Crohn's disease and cancer. N Engl J Med 19732891099–1103. [DOI] [PubMed] [Google Scholar]
- 3.Weterman I T, Biemond I, Pena A S. Mortality and causes of death in Crohn's disease. Review of 50 years' experience in Leiden University Hospital. Gut 1990311387–1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ekbom A, Helmick C G, Zack M.et al Survival and causes of death in patients with inflammatory bowel disease: a population‐based study. Gastroenterology 1992103954–960. [DOI] [PubMed] [Google Scholar]
- 5.Persson P G, Bernell O, Leijonmarck C E.et al Survival and cause‐specific mortality in inflammatory bowel disease: a population‐based cohort study. Gastroenterology 19961101339–1345. [DOI] [PubMed] [Google Scholar]
- 6.Jess T, Winther K V, Munkholm P.et al Mortality and causes of death in Crohn's disease: follow‐up of a population‐based cohort in Copenhagen County, Denmark. Gastroenterology 20021221808–1814. [DOI] [PubMed] [Google Scholar]
- 7.Loftus E V, Jr, Silverstein M D, Sandborn W J.et al Crohn's disease in Olmsted County, Minnesota, 1940–1993: incidence, prevalence, and survival. Gastroenterology 19981141161–1168. [DOI] [PubMed] [Google Scholar]
- 8.Palli D, Trallori G, Saieva C.et al General and cancer specific mortality of a population based cohort of patients with inflammatory bowel disease: the Florence Study. Gut 199842175–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Farrokhyar F, Swarbrick E T, Grace R H.et al Low mortality in ulcerative colitis and Crohn's disease in three regional centers in England. Am J Gastroenterol 200196501–507. [DOI] [PubMed] [Google Scholar]
- 10.Masala G, Bagnoli S, Ceroti M.et al Divergent patterns of total and cancer mortality in ulcerative colitis and Crohn's disease patients: the Florence IBD study 1978–2001. Gut 2004531309–1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Probert C S, Jayanthi V, Wicks A C.et al Mortality from Crohn's disease in Leicestershire, 1972–1989: an epidemiological community based study. Gut 1992331226–1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cottone M, Magliocco A, Rosselli M.et al Mortality in patients with Crohn's disease. Scand J Gastroenterol 199631372–375. [DOI] [PubMed] [Google Scholar]
- 13.Langholz E, Munkholm P, Davidsen M.et al Colorectal cancer risk and mortality in patients with ulcerative colitis. Gastroenterology 19921031444–1451. [DOI] [PubMed] [Google Scholar]
- 14.Probert C S, Jayanthi V, Wicks A C.et al Mortality in patients with ulcerative colitis in Leicestershire, 1972–1989. An epidemiological study. Dig Dis Sci 199338538–541. [DOI] [PubMed] [Google Scholar]
- 15.Davoli M, Prantera C, Berto E.et al Mortality among patients with ulcerative colitis: Rome 1970–1989. Eur J Epidemiol 199713189–194. [DOI] [PubMed] [Google Scholar]
- 16.Viscido A, Bagnardi V, Sturniolo G C.et al Survival and causes of death in Italian patients with ulcerative colitis. A GISC nationwide study. Dig Liver Dis 200133686–692. [DOI] [PubMed] [Google Scholar]
- 17.Loftus E V, Jr, Silverstein M D, Sandborn W J.et al Ulcerative colitis in Olmsted County, Minnesota, 1940–1993: incidence, prevalence, and survival. Gut 200046336–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Winther K V, Jess T, Langholz E.et al Survival and cause‐specific mortality in ulcerative colitis: follow‐up of a population‐based cohort in Copenhagen County. Gastroenterology 20031251576–1582. [DOI] [PubMed] [Google Scholar]
- 19.Stewenius J, Adnerhill I, Anderson H.et al Incidence of colorectal cancer and all cause mortality in non‐selected patients with ulcerative colitis and indeterminate colitis in Malmo, Sweden. Int J Colorectal Dis 199510117–122. [DOI] [PubMed] [Google Scholar]
- 20.Wandall E P, Damkier P, Moller P F.et al Survival and incidence of colorectal cancer in patients with ulcerative colitis in Funen county diagnosed between 1973 and 1993. Scand J Gastroenterol 200035312–317. [DOI] [PubMed] [Google Scholar]
- 21.Melton L J., iii History of the Rochester Epidemiology Project. Mayo Clinic Proc 199671266–274. [DOI] [PubMed] [Google Scholar]
- 22.Loftus C G, Loftus E V, Jr, Sandborn W J.et al Update on incidence and prevalence of Crohn's Disease (CD) and ulcerative colitis (UC) in Olmsted County, Minnesota. Gastroenterology 2003124A36 [Google Scholar]
- 23.Ljung T, Karlen P, Schmidt D.et al Infliximab in inflammatory bowel disease: clinical outcome in a population based cohort from Stockholm County. Gut 200453849–853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lichtenstein G R, Cohen R D, Feagan B G.et al Safety of infliximab and other Crohn's disease therapies—updated treat™ registry data with over 10,000 patient‐years of follow‐up. Gastroenterology 2005128(suppl 2)A580 [Google Scholar]
- 25.Orholm M, Binder V, Sorensen T I.et al Concordance of inflammatory bowel disease among Danish twins. Results of a nationwide study. Scand J Gastroenterol 2000351075–1081. [DOI] [PubMed] [Google Scholar]
- 26.Gyde S, Prior P, Dew M J.et al Mortality in ulcerative colitis. Gastroenterology 19828336–43. [PubMed] [Google Scholar]
- 27.Gyde S N, Prior P, Alexander F.et al Ulcerative colitis: why is the mortality from cardiovascular disease reduced? Q J Med 198453351–357. [PubMed] [Google Scholar]
- 28.Eaden J A, Abrams K R, Mayberry J F. The risk of colorectal cancer in ulcerative colitis: a meta‐analysis. Gut 200148526–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jess T, Loftus E V, Jr, Velayos F S.et al Risk of intestinal cancer in inflammatory bowel disease: a population‐based study from Olmsted County, Minnesota, 1940–2001. Gastroenterology 20061301039–1046. [DOI] [PubMed] [Google Scholar]