Training is an increasingly relevant issue in the UK.1 The structure of postgraduate medical training is undergoing significant change at present, with attempts to streamline and shorten duration. Modernising medical careers (MMC) marks a major reform in postgraduate medical education.2
Endoscopic retrograde cholangiopancreatography (ERCP) requires considerable training to perform effectively and safely.3 Competency has been based on total procedure numbers performed by trainees. Consensus suggests 180–200 diagnostic/therapeutic ERCPs are required to obtain competence within a training facility with sufficient case volume for viable training opportunities.2 Selective cannulation of the bile duct has been used as a benchmark for technical success.4 Moreover, multivariate analyses find case volume to independently predict ERCP related complications.5,6,7,8
“Diagnostic” ERCP should rarely be required with the increasing accessibility to newer imaging modalities. Magnetic resonance cholangiopancreatography (MRCP) has been found to be of equivalent diagnostic utility as ERCP. Such developments may reduce ERCP case volume and potentially increase procedure complexity with implications for service and training. Few studies have reported potential changes to ERCP practice following MRCP introduction.
To test our hypothesis that MRCP introduction may produce quantitative and qualitative changes to existing ERCP practice, we assessed 542 consecutive ERCPs during a 28 month period from November 2001 to February 2004 from a prospective database. The effect of MRCP introduction on ERCP practice was assessed 14 months after the addition of MRCP facilities to our unit and compared with the 14 month period prior to MRCP introduction.
Pre‐MRCP introduction, 310 ERCPs (298 with complete data) were performed and 232 were performed in the post‐MRCP period. Indications for ERCP were categorised by clinical, biochemical, and ultrasound (USS) findings and the likelihood of therapeutic intervention for each indication assessed before and after MRCP introduction. Failed cannulation was defined by the inability to cannulate the papilla and opacify the required duct.
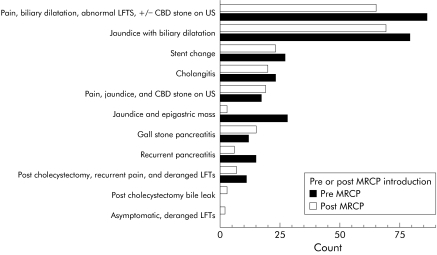
The ERCP indication profile changed little following MRCP introduction (fig 1). A 25% reduction in total ERCP numbers was found in the post‐MRCP period and the monthly mean number of ERCPs performed was reduced from 22 to 17 per month.
Figure 1 Indications for endoscopic retrograde cholangiopancreatography (ERCP) in pre‐magnetic resonance cholangiopancreatography (MRCP) and post‐MRCP introduction periods. CBD, common bile duct; LTFS, liver function tests.
Cannulation failure rates pre‐MRCP and post‐MRCP were 8.7% (26 ERCPs) and 14.2% (33 ERCPs), respectively. Pre‐MRCP introduction, 191 of 272 (70%) successful cannulations were with therapeutic intent. Post‐MRCP introduction, 163 of 232 (81%) successful cannulations were with therapeutic intent. Significant increases in the proportion of therapeutic procedures (odds ratio (OR) 1.74 (95% confidence interval (CI) 1.13–2.69); p = 0.012) and failed cannulations (OR 1.74 (95% CI 1.005–2.99); p = 0.046) were therefore identified. No significant associations existed between each ERCP indication and failed cannulation. Changes in therapeutic intervention following MRCP introduction for each indication are highlighted in table 1.
Table 1 Indication and therapeutic intervention.
| Indication | Therapeutic intervention | Pre‐MRCP (n = ) | Post‐MRCP (n = ) | OR (95% CI) |
|---|---|---|---|---|
| Pain, biliary dilatation, abnormal LFTs±CBD stone on USS | Yes | 31 | 40 | 2.92 (1.43–5.97) |
| No | 43 | 19 | ||
| Jaundice with biliary dilatation | Yes | 70 | 44 | 0.53 (0.13–1.98) |
| No | 4 | 5 | ||
| Stent change | Yes | 27 | 23 | N/A |
| No | 0 | 0 | ||
| Cholangitis | Yes | 20 | 15 | 0.25 (0.02–2.65) |
| No | 1 | 3 | ||
| Pain, jaundice, and CBD stone | Yes | 12 | 18 | 3.00 (0.24–36.9) |
| No | 2 | 1 | ||
| Jaundice with epigastric mass | Yes | 12 | 1 | 0.93 (0.82–1.07) |
| No | 13 | 2 | ||
| Gall stone pancreatitis | Yes | 8 | 9 | 0.84 (0.14–4.97) |
| No | 3 | 4 | ||
| Recurrent pancreatitis | Yes | 3 | 3 | 5.50 ( 0.61–49.5) |
| No | 11 | 2 | ||
| Post cholecystectomy, recurrent pain, and deranged LFTs | Yes | 6 | 5 | 1.67 (0.21–13.2) |
| No | 4 | 2 | ||
| Post cholecystectomy bile leak | Yes | 0 | 2 | N/A |
| No | 0 | 1 | ||
| Asymptomatic with deranged LFTs | Yes | 0 | 0 | N/A |
| No | 0 | 2 |
MRCP, magnetic resonance cholangiopancreatography; CBD, common bile duct; LTFS, liver function tests; USS, ultrasound; N/A not applicable; OR (95% CI), odds ratio (95% confidence interval).
We have encountered alterations in ERCP practice following MRCP introduction with fewer, potentially more complex, procedures being performed. Subset analysis found change only in the group with pain, biliary dilatation, with abnormal LFTs±CBD stone on USS, potentially reflecting improved identification of duct stones by MRCP. Objective assessment of technical difficulty was not easy, as both trainees and trainers were both involved in performing ERCPs and no validated criteria to assess ERCP difficulty were available during the study period.
MRCP introduction has an impact on ERCP practice. ERCP services and training may require redirection towards fewer but more complex procedures. These changes may necessitate a reduction in the number of cases performed on a list, may result in fewer trainees embarking on ERCP training and, as endoscopy centres require threshold numbers of cases to ensure competency in technique and adequacy of training, may reduce the number of centres able to offer viable training opportunities.
Footnotes
Conflict of interest: None declared.
References
- 1.Anwar M, Irfan S, Daly N.et al EWTD has negative impact on training for surgeons. BMJ 20053311476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Poole A. The implications of modernising medical careers for specialist registrars. BMJ 2003326s194. [DOI] [PubMed] [Google Scholar]
- 3.American Society for Gastrointestinal Endoscopy Principles of training in gastrointestinal endoscopy. Gastrointest Endosc 199949845–853. [PubMed] [Google Scholar]
- 4.Freeman M L. Training and competence in gastrointestinal endoscopy. Rev Gastroenterol Disord 2001173–86. [PubMed] [Google Scholar]
- 5.Freeman M L, DiSario J A, Nelson D B.et al Risk factors for post‐ERCP pancreatitis: a prospective, multicenter study. Gastrointest Endosc 200154425–434. [DOI] [PubMed] [Google Scholar]
- 6.Loperfido S, Angelini G, Benedetti G.et al Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc 1998481–10. [DOI] [PubMed] [Google Scholar]
- 7.Freeman M L, Nelson D B, Sherman S.et al Complications of endoscopic biliary sphincterotomy. N Engl J Med 1996335909–918. [DOI] [PubMed] [Google Scholar]
- 8.Freeman M L. Procedure‐specific outcomes assessment for endoscopic retrograde cholangiopancreatography. Gastrointest Endosc Clin N Am 19999639–647. [PubMed] [Google Scholar]