Surgery is the primary treatment of non‐metastatic colon cancer. En bloc removal of the colon with its associated mesenteric lymph nodes is essential. However, the number of lymph nodes reported with colectomy varies widely and may be a result of variation in the actual number of regional lymph nodes, surgical technique, or the thoroughness of the pathologist in finding lymph nodes. The number of lymph node metastases is an important negative prognostic factor and is used in stratification schemes for clinical trials.1
Recent studies have emphasised the fact that examining a greater number of nodes increases the likelihood of correct staging and is associated with better survival, after controlling for the number of nodes involved.2 Hence, the Will Rogers phenomenon may profoundly affect the reported outcome of colon cancer.3 Indeed, experienced teams often perform meticulous and extensive lymph node dissection, which increases the probability of finding nodes. This not only affects the expected outcome but may also influence decisions on adjuvant treatments. Patients with inadequate lymph node resection could therefore receive less efficient adjuvant treatment. Berger et al reported that the ratio of metastatic to examined lymph nodes (the lymph node ratio (LNR)) may decrease the amount of stage migration, and is an important prognostic factor in colon cancer, using four LNR groups.3
We compared directly the UICC staging system in node positive colon cancer (metastases in 1–3 (pN1) versus in 4 or more (pN2) regional lymph nodes) to LNR based staging, using two prognostic groups. Data were extracted from the surveillance, epidemiology, and end results (SEER) 9 registries.4 Selection criteria were histology confirmed primary colorectal cancer, diagnosed between 1988 and 1997, surgically resected, and node positive disease. Data from 26 181 patients were included in the study, of which 3941 received radiotherapy. Median number of examined nodes was 10. The number of positive nodes increased with the number of nodes examined (pairwise correlation coefficient = 0.36; p<0.0001).
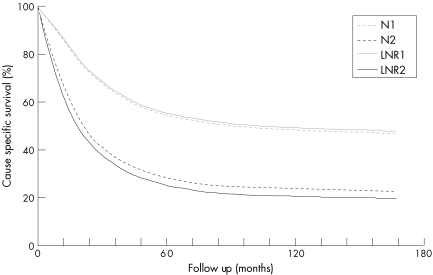
The endpoint of the study was cause specific survival. The number of events was 14 121, with a median follow up of 92 months. The optimal cut off (LNR1 v LNR2), determined using the Nagelkerke's r2 index, was 0.4. In the Cox multivariate analysis, LNR appeared to be a strong independent risk factor (p<0.0001), next to sex, age at diagnosis, race, marital status, tumour size, level of cancer infiltration (pT), histological grade, number of positive nodes, and number of nodes removed. Comparison between the LNR and UICC pN stage was performed using Kaplan‐Meyer survival estimates and log rank tests (fig 1). The group of patients with LNR1 and LNR2 had a five year cause specific survival of 56% and 25%, respectively. In comparison, pN1 and pN2 stages displayed a five year cause survival of 54% and 28%, respectively. Hence prognostic separation using LNR was 31% compared with 26% using the UICC pN stage.
Figure 1 Prognostic value of a number based (N1–2) compared with a ratio based (LNR 1–2) staging system in colon cancer. LNR, lymph node ratio.
Therefore, we propose using the LNR in future staging systems for colon cancer, in stratification schemes for clinical trials, and to compare interinstitutional treatment results.
Footnotes
This work was supported by grants from “Foundation against Cancer, foundation of public interest”, and the “Scientific Fund W Gepts AZ‐VUB”.
Conflict of interest: None declared.
References
- 1.Suzuki O, Sekishita Y, Shiono T.et al Number of lymph node metastases is better predictor of prognosis than level of lymph node metastasis in patients with node‐positive colon cancer. J Am Coll Surg 2006202732–736. [DOI] [PubMed] [Google Scholar]
- 2.Le Voyer T E, Sigurdson E R, Hanlon A L.et al Colon cancer survival is associated with increasing number of lymph nodes analyzed: a secondary survey of intergroup trial INT‐0089. J Clin Oncol 2003212912–2919. [DOI] [PubMed] [Google Scholar]
- 3.Berger A C, Sigurdson E R, LeVoyer T.et al Colon cancer survival is associated with decreasing ratio of metastatic to examined lymph nodes. J Clin Oncol 2005238706–8712. [DOI] [PubMed] [Google Scholar]
- 4.Surveillance, Epidemiology, and End Results (SEER) Program www.seer.cancer.gov (last accessed 4 September 2006) Public‐Use Data (1973‐2001), National Cancer Institute, DCCPS, Surveillance Research Program, Cancer Statistics Branch, released April 2004, based on the November 2003 submission