Perioperative visual loss has been associated with many types of non‐ocular surgery.1 Risk factors include combinations of prolonged surgical times, hypotension, anaemia due to blood loss, or prone positioning.2 We are not aware of another report of perioperative visual loss in which the only risk factor was hypotension.
Case report
A 55 year old man had left rotator cuff surgery. He was supine, surgical time was 3 hours, and blood loss was minimal. Postoperatively he experienced “kaleidoscopic” vision in the inferior visual field of his left eye which cleared. Four weeks later he had right rotator cuff surgery. Again he was supine, surgery lasted 2–3 hours, and blood loss was 100 ml. After recovery he had “kaleidoscopic” vision in the same eye. It did not resolve and his vision continued to deteriorate prompting him to seek ophthalmological care.
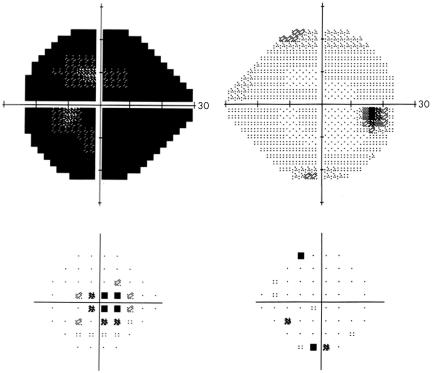
His medical history was significant for treated hyperlipidaemia. He quit smoking 35 years earlier. Visual acuity was 20/20 in the right eye and counting fingers in the left. He identified 9/12 colour plates in the right eye and 0/12 in the left. He had a left afferent papillary defect. The right optic disc was congenitally anomalous, the left pale and swollen. Visual fields revealed an inferior arcuate defect in the left eye.
Figure 1 Humphrey automated perimetry after the second surgery and loss of vision in the left eye.
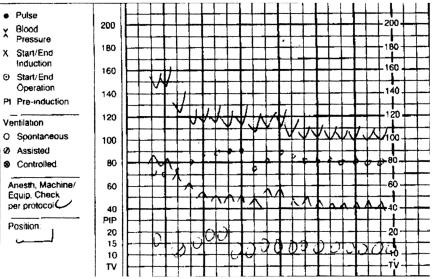
Figure 2 Intraoperative anaesthesia record showing 80 minute drop in mean arterial pressure. Small boxes, 10 minutes; Large boxes, 30 minutes; downward pointing arrowheads, systolic pressure; upward pointing arrowheads, diastotic pressure.
Comment
Many types of non‐ophthalmic surgery have been associated with anterior ischaemic optic neuropathy (AION).1 Our patient's preoperative risk factors included treated hyperlipidaemia and anomalous nerves. During surgery he did not have any of the established risk factors for perioperative non‐AION with the exception of prolonged hypotension. His MAP was reduced by 41.6% for 80 minutes. The previous surgery on the patient's left side decreased the MAP only 28%.
It is likely that this hypotension combined with anomalous nerves led to his optic nerve infarction. The perfusion pressure of the eye drops linearly with the mean arterial blood pressure.3 If there are areas of atherosclerosis or watershed zones present in a particular optic nerve a significant drop in the perfusion pressure to the eye could result in ischaemia. Of interest, he experienced transient visual obscurations after his first surgery with a smaller drop in his MAP, perhaps signifying a vascular system susceptible to hypotensive episodes.
Bhatti and Enneking described decreased vision and ophthalmoparesis following rotator cuff surgery but the patient did not have non‐AION and the vision eventually recovered.4 In addition, after a review of Medline, we did not find any other cases of perioperative visual loss in whichh the only risk factor was prolonged hypotension. This underscores the importance of hypotension as an independent risk factor for perioperative visual loss.
References
- 1.Chang M A, Sigurdson W, tempelhoff R.et al Visual loss after spine surgery: a survey. Neurosurg 200046625–630. [DOI] [PubMed] [Google Scholar]
- 2.Katz D M, Trobe J D, Cornblath W.et al Ischemic optic neuropathy. Arch Ophthalmol 1994112925–931. [DOI] [PubMed] [Google Scholar]
- 3.Hayreh S S. Anterior ischemic optic neuropathy. Clin Neuro 19974251–263. [PubMed] [Google Scholar]
- 4.Bhatti M T, Enneking F K. Visual loss and ophthalmoplegia after shoulder surgery. Anes Anal 200396899–902. [DOI] [PubMed] [Google Scholar]