Abstract
Aim
To study the prevalence rate of uncorrected refractive error and associated risk factors among Singapore schoolchildren aged 12–16 years (grade 7).
Methods
A cross sectional study of 628 participants (participation rate 99.8%) was conducted in two schools. An interviewer led questionnaire asking about sociodemographic variables and risk factors was administered. Refractive errors were measured using a table mounted autorefractor. Participants with habitual visual acuity (VA) of 0.2 logMAR or worse underwent subjective refraction. Uncorrected refractive error was defined as improvement of at least 0.2 logMAR in best corrected visual acuity after subjective refraction.
Results
The prevalence rate of uncorrected refractive error was 22.3% (95% confidence interval (CI) 19.0% to 25.5%). The multivariate adjusted odds ratio of uncorrected refractive error in students with the lowest academic ability was 2.24 (95% CI 1.34 to 3.73). Increasing time interval since the last visit to an eye care provider increased the risk of uncorrected refractive error (trend p = 0.001).
Conclusion
Uncorrected refractive error was a significant problem among Singapore students aged 12–16 years (grade 7). Uncorrected refractive error was more common among students with low academic ability or those who had not visited an eye care provider for a long time.
Keywords: refractive errors, children, cross sectional studies, Singapore
Recent studies have highlighted the importance of uncorrected refractive error as one of the leading causes of visual impairment.1,2,3,4 As a consequence, the World Health Organization has adopted the correction of refractive errors in developed and developing countries as one of the main priorities of its “Vision 2020: the right to sight” initiative.5
Myopia is a major public health concern in Singapore, which has one of the highest prevalence rates in the world.6 Among children aged 7 years, 28% were myopic7; and 83% of Singapore military conscripts were myopic.8,9,10 Thus, the under or over correction of refractive error may also be a sizeable problem in Singapore.
While several studies have reported on the prevalence rates of uncorrected refractive error in adult populations,1,2,3,4 data relevant to school age children, notably in South East Asia, are sparse. The multinational Refractive Error Study in Children (RESC) found that the prevalence rate of baseline visual acuity of less than 20/32 among 5–15 year old children in the People's Republic of China was 10.9%, of which 9.2% could potentially benefit from prescription glasses.11 The respective rates were 14.7% and 7.3% in Chile, and 2.8% and 1.5% in Nepal.12,13
The aim of this study was to investigate the prevalence rate and associated risk factors for uncorrected refractive error in grade 7 students in Singapore.
Materials and methods
This cross sectional survey was carried out by a group of third year medical students from the National University of Singapore (NUS) during a community health project (CHP) component of the medical curriculum in January 2005. A total of 630 grade 7 junior high school (secondary one) students from two schools in the northern and western parts of Singapore were selected. Approval for the study was obtained from the community health project staff committee at the community, occupational and family medicine department, NUS. Participants and their parents or guardians were provided with information leaflets detailing the study objectives and the measurement procedures. The nature of the study was described in the informational leaflets. If the parents or the participants chose not to participate, they would inform the study investigators. Owing to logistic constraints, the school principals preferred that signed consents were not obtained.
Questionnaire
We assessed sociodemographic variables and possible risk factors for uncorrected refractive error using an interviewer led questionnaire, which took an average of 45 minutes to complete. The questionnaire was administered en masse to the participants at each school. Oral explanations were provided to students who had difficulty understanding or completing the questionnaire.
Sociodemographic variables included were parents' highest educational levels, parents' occupations, housing type, total household income, and educational stream at school. The educational streams reflect academic ability and junior high school students in Singapore are assigned to the following streams: “special (highest academic ability),” “express (next highest ability),” “normal academic (intermediate ability),” or “normal technical (lowest ability),” according to their performance at the primary school leaving examination (PSLE), a nationwide examination for grade 6 students (12 years). The following possible risk factors for uncorrected refractive error were also assessed: existing eye conditions, the time interval since the last visit to an eye care provider (such as an optician, an optometrist, or an ophthalmologist) and the frequency of visits to an eye care provider.
Ocular examination
Distance habitual visual acuity was measured using a modified ETDRS logarithm of the minimum angle of resolution (logMAR) chart at 4 metres under standard lighting conditions in the schools. Refraction was determined using a stand alone autorefractor (Canon RK‐5 Autorefractor, Canon Inc, Japan). Participants with habitual visual acuity of 0.2 logMAR or worse underwent subjective refraction and were assessed for best corrected visual acuity. Uncorrected refractive error was defined in our study as an improvement of at least 0.2 logMAR (two lines equivalent) in the best corrected visual acuity in subjects with a habitual visual acuity of 0.2 logMAR or worse. Refractive error was expressed as spherical equivalent (SE; defined as sphere + half cylinder). Myopia was defined as an SE of at least −1.00 dioptres (D), hyperopia as an SE of at least +1.00 D, and astigmatism as cylinder of at least −1.00 D in any eye. Non‐habitual visual aid wearers were defined as individuals without visual aid correction on the day of ocular examination (that is, students who did not have visual aids or students who had but did not wear them regularly). Visual aids referred to spectacles and contact lenses, which were both popular in the local student population. Students with uncorrected refractive error or less than optimal visual acuity were referred to ophthalmologists for further management.
Statistical analysis
Data were analysed using SPSS version 12.0 for Windows. Proportions were compared using χ2 test. Associations of sociodemographic variables and uncorrected refractive error were evaluated. A p value less than or equal to 0.05 was used to establish statistical significance for all tests. Multiple logistic regression models were used to study the relation between uncorrected refractive error and selected factors.
Results
Of the 630 eligible students, 629 aged 12–16 years participated (99.8% response), including 335 females (53.3%) and 294 males (46.7%), with a mean age of 12.13 years. There were 425 Chinese (67.6%), 125 Malays (19.9%), 64 Indians (10.2%), and 15 from other races (2.4%). There were 336 students in the express stream (53.4%), 161 in normal academic (25.6%), and 132 in normal technical (21.0%) streams. These figures were similar to those of the national grade 7 population statistics published by the Ministry of Education, Singapore14; 43.8% had pure myopia, 4.3% pure hyperopia, 3.2% pure astigmatism, and 22.4% mixed refractive errors, most commonly, myopic astigmatism. Lastly, 21.8% of the students were emmetropic.
In this study, 140 of the 629 students had uncorrected refractive error, giving rise to a prevalence rate of 22.3% (95% confidence interval, 19.0, 25.6).
Table 1 describes the proportion of uncorrected refractive error using sociodemographic variables and possible risk factors. The prevalence rates of uncorrected refractive error were similar between the sexes (males 20.7% and females 23.6%), and among the races (Chinese 21.4%, Malay 22.4%, Indian and other races 21.0%).
Table 1 Prevalence rates of uncorrected refractive error (n = 629).
| No | Number with uncorrected refractive error | Uncorrected refractive error, percentage (95% CI) | Crude odds ratio (95% CI) | p Value (χ2 test) | |
|---|---|---|---|---|---|
| Total | 629 | 140 | 22.3 (19.0 to 25.6) | ||
| Sex | |||||
| Male | 294 | 61 | 20.7 (16.1 to 25.3) | 1 (referent) | |
| Female | 335 | 79 | 23.6 (19.1 to 28.1) | 1.18 (0.81 to 1.72) | 0.442 |
| Race | |||||
| Chinese | 425 | 91 | 21.4 (17.5 to 25.3) | 1 (referent) | |
| Malay | 125 | 28 | 22.4 (15.1 to 29.7) | 1.06 (0.66 to 1.71) | |
| Indian and others | 79 | 21 | 21.0 (13.5 to 30.3) | 1.33 (0.77 to 2.30) | 0.597 |
| Age (years) | |||||
| 12 | 578 | 126 | 21.8 (18.4 to 25.2) | 1 (referent) | 0.100 |
| 13 | 27 | 4 | 14.8 (1.4 to 28.2) | 0.62 (0.21 to 1.84) | (trend) |
| >13 | 24 | 10 | 41.7 (22.0 to 61.4) | 2.56 (1.11 to 5.91) | |
| Educational stream | |||||
| Express | 336 | 66 | 19.6 (15.4 to 23.8) | 1 (referent) | 0.014 |
| Normal academic | 161 | 33 | 20.5 (14.3 to 26.7) | 1.05 (0.66 to 1.68) | (trend) |
| Normal technical | 132 | 41 | 31.1 (23.2 to 39.0) | 1.84 (1.17 to 2.91) | |
| Number of parents with refractive error | |||||
| 0 | 236 | 54 | 22.9 (17.5 to 28.2) | 1 (referent) | 0.904 |
| 1 | 211 | 43 | 20.4 (14.9 to 25.8) | 0.86 (0.55 to 1.36) | (trend) |
| 2 | 182 | 43 | 23.6 (17.4 to 29.8) | 1.04 (0.66 to 1.65) | |
| Existing eye condition(s) | |||||
| Emmetropia only | 137 | 10 | 7.3 (6.56 to 8.04) | 1 (referent) | <0.001 |
| Myopia only | 304 | 80 | 26.3 (21.4 to 31.3) | 4.54 (2.27 to 9.07) | |
| Hyperopia only | 27 | 3 | 11.1 (2.35 to 29.2) | 1.59 (0.41 to 6.20) | |
| Astigmatism only | 20 | 4 | 20.0 (5.73 to 43.7) | 3.18 (0.89 to 11.3) | |
| Two or more of the above | 141 | 43 | 30.5 (22.9 to 38.1) | 5.57 (2.67 to 11.6) | |
| Use of visual aid—spectacles or contact lenses | |||||
| Habitually worn | 365 | 95 | 26.0 (21.5 to 30.5) | 1 (referent) | 0.009 |
| Habitually not worn | 264 | 45 | 17.0 (12.5 to 21.5) | 0.58 (0.39 to 0.87) | |
| Consult optician | |||||
| Ever | 411 | 110 | 26.8 (22.5 to 31.0) | 1 (referent) | <0.001 |
| Never | 218 | 30 | 13.8 (9.19 to 18.3) | 0.44 (0.28 to 0.68) | |
The prevalence rates of uncorrected refractive error among express students, normal academic students, and normal technical students were 19.6%, 20.5%, and 31.1% respectively (p for trend = 0.014). Among participants who habitually wore visual aids, 26.0% were found to have uncorrected refractive error, compared to 17.0% among those who did not wear visual aids habitually (p = 0.009). The prevalence rate of uncorrected refractive error was 26.8% among students who had ever consulted any eye care provider, compared to 13.8% for those who had not (p<0.001). Existing eye conditions were also associated with uncorrected refractive error (p<0.001); 26.3% of the myopic students were found to have uncorrected refractive error and 30.5% of students with mixed refractive errors had uncorrected refractive error.
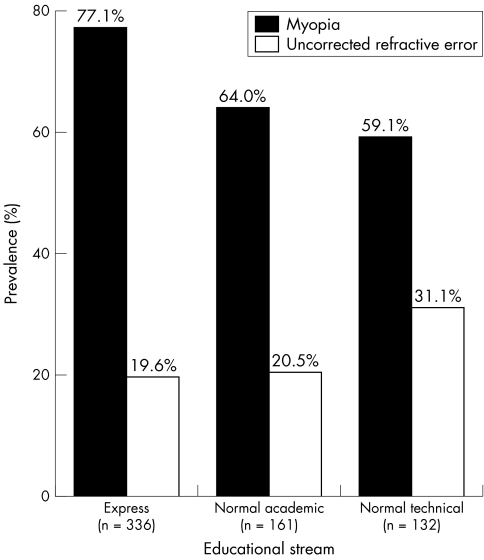
In addition to prevalence rates among the educational streams, figure 1 shows the prevalence rates of myopia among these streams: 77.1% for express, 64.0% for normal academic, and 59.1% for normal technical.
Figure 1 Relation between the educational stream and prevalence of myopia, and between the educational stream and prevalence of uncorrected refractive error.
A multiple logistic regression model was constructed with uncorrected refractive error as the dependent variable and sex, race, age, educational streams and existing eye conditions as the explanatory covariates (table 2). Normal technical students were 2.24 times more likely to have uncorrected refractive error compared with the express students. But the normal academic students did not have a significantly higher risk (odds ratio = 1.27) compared with the express students. The odds ratio of having uncorrected refractive error among students with myopia and with mixed refractive errors were 5.54 and 7.40 respectively, compared with emmetropic students in multivariate analysis.
Table 2 Multiple logistic regression model of the predictors of uncorrected refractive error among all students (n = 629).
| No | Multivariate odds ratio (95% CI) | p Value | |
|---|---|---|---|
| Total | 629 | ||
| Sex | |||
| Male | 294 | 1 (referent) | 0.23 |
| Female | 335 | 1.28 (0.86 to 1.91) | |
| Race | |||
| Chinese | 425 | 1 (referent) | – |
| Malay | 125 | 1.09 (0.65 to 1.83) | 0.75 |
| Indian and others | 79 | 1.53 (0.84 to 2.78) | 0.17 |
| Age (years) | |||
| 12 | 578 | 1.34 (0.92 to 1.97) | 0.13 |
| 13 | 27 | ||
| >13 | 24 | ||
| Stream | |||
| Express | 336 | 1 (referent) | – |
| Normal academic | 161 | 1.27 (0.78 to 2.06) | 0.35 |
| Normal technical | 132 | 2.24 (1.34 to 3.73) | 0.002 |
| Existing eye condition(s) | |||
| Emmetropia only | 137 | 1 (referent) | – |
| Myopia only | 304 | 5.54 (2.71 to 11.29) | <0.001 |
| Hyperopia only | 27 | 1.66 (0.42 to 6.65) | 0.47 |
| Astigmatism only | 20 | 3.28 (0.90 to 12.02) | 0.07 |
| Two or more of the above | 141 | 7.40 (3.43 to 15.96) | <0.001 |
*Adjusted for all other factors in the table and school.
The rates of uncorrected refractive error among students who habitually wore visual aids were evaluated in table 3. Prevalence rates of uncorrected refractive error among the express, the normal academic and the normal technical students were 22.2%, 26.4% and 42.9%, respectively (p for trend = 0.005). In addition, the prevalence rate of uncorrected refractive error increased with increasing interval since the last visit to an eye care provider: 21.0% for within last 6 months, 22.7% for between 6 months and 1 year, 37.3% for between 1 year and 2 years, and 50.0% for more than 2 years (p for trend = 0.001).
Table 3 Prevalence rates of uncorrected refractive error among students who habitually wore visual aids (N = 365).
| No | Number with uncorrected refractive error | Uncorrected refractive error, percentage (95% CI) | Crude odds ratio (95% CI) | p Value (χ2 test) | |
|---|---|---|---|---|---|
| Total | 365 | 95 | 26.8 (22.5 to 31.0) | ||
| Sex | |||||
| Male | 163 | 37 | 22.7 (16.3 to 29.1) | 1 (referent) | 0.230 |
| Female | 202 | 58 | 28.7 (22.5 to 35.0) | 1.37 (0.85 to 2.21) | |
| Race | |||||
| Chinese | 276 | 67 | 24.3 (19.2 to 29.3) | 1 (referent) | 0.402 |
| Malay | 50 | 16 | 32.0 (19.5 to 46.7) | 1.47 (0.76 to 2.83) | |
| Indian and others | 39 | 12 | 23.5 (12.8 to 37.5) | 1.39 (0.67 to 2.89) | |
| Age (years) | |||||
| 12 | 344 | 89 | 25.9 (21.2 to 30.5) | 1 (referent) | 0.460 |
| 13 | 12 | 2 | 16.7 (2.08 to 48.4) | 0.57 (0.12 to 2.67) | |
| >13 | 9 | 4 | 44.4 (13.7 to 78.8) | 2.29 (0.60 to 8.73) | |
| Stream | |||||
| Express | 225 | 50 | 22.2 (16.8 to 27.7) | 1 (referent) | 0.005 |
| Normal academic | 91 | 24 | 26.4 (17.7 to 36.3) | 1.25 (0.71 to 2.20) | (trend) |
| Normal technical | 49 | 21 | 42.9 (28.8 to 57.8) | 2.62 (1.37 to 5.01) | |
| Number of parents with refractive error | |||||
| 0 | 114 | 36 | 31.6 (23.0 to 40.1) | 1 (referent) | 0.244 |
| 1 | 134 | 30 | 22.4 (15.3 to 29.4) | 0.63 (0.36 to 1.10) | |
| 2 | 117 | 29 | 24.8 (17.0 to 32.6) | 0.71 (0.40 to 1.27) | |
| Existing eye condition(s) | |||||
| Emmetropia only | 11 | 2 | 18.2 (2.29 to 51.8) | 1 (referent) | 0.802 |
| Myopia only | 219 | 54 | 24.7 (18.9 to 30.4) | 1.47 (0.31 to 7.03) | |
| Hyperopia only | 2 | 1 | 50.0 (12.6 to 98.7) | 4.50 (0.19 to 107) | |
| Astigmatism only | 4 | 1 | 25.0 (.62 to 80.6) | 1.50 (0.10 to 23.1) | |
| Two or more of the above | 129 | 37 | 28.7 (20.9 to 36.5) | 1.81 (0.37 to 8.78) | |
| Last visit to eye care provider | |||||
| <6 months ago | 162 | 34 | 21.0 (14.7 to 27.3) | 1 (referent) | 0.001 |
| >6 months, <1 year ago | 113 | 25 | 22.7 (14.9 to 30.6) | 1.05 (0.58 to 1.89) | (trend) |
| >1 year, <2 years | 75 | 28 | 37.3 (26.4 to 49.3) | 2.24 (1.23 to 4.09) | |
| >2 years | 15 | 8 | 50.0 (26.0 to 74.0) | 3.76 (1.39 to 10.2) | |
| Frequency of visit to eye care provider | |||||
| Once every 1–6 months | 77 | 25 | 32.5 (22.2 to 44.1) | 1 (referent) | 0.534 |
| Once every 7–12 months | 169 | 34 | 19.9 (13.8 to 26.0) | 0.52 (0.29 to 0.96) | (trend) |
| Once every 13–24 months | 104 | 28 | 26.9 (18.4 to 35.4) | 0.77 (0.40 to 1.46) | |
| No visit in recent 2 years | 15 | 8 | 53.3 (26.6 to 78.7) | 2.38 (0.78 to 7.29) | |
Among habitual visual aid wearers, a multiple logistic regression model was constructed with uncorrected refractive error as the dependent variable and sex, race, educational stream, and interval since the last visit to an eye care provider as explanatory co‐variates (table 4). After multivariate adjustment, the normal technical students were 2.57 times more likely to have uncorrected refractive error compared with the express students. There was no significantly higher risk for the normal academic students (odds ratio = 1.12, 95% confidence interval 0.62 to 2.01). The multivariate adjusted odds ratio for a last visit to an eye care provider between 6 months to 1 year ago was 1.20, between 1–2 years ago was 2.39, and more than 2 years ago was 4.22, compared to a visit less than 6 months ago.
Table 4 Multiple logistic regression model of the predictors of uncorrected refractive error among students who wear visual aids habitually (n = 365).
| No | Multivariate odds ratio (95% CI) | p Value | |
|---|---|---|---|
| Total | 365 | ||
| Sex | |||
| Male | 163 | 1 (referent) | 0.12 |
| Female | 202 | 1.49 (0.90 to 2.50) | |
| Race | |||
| Chinese | 276 | 1 (referent) | – |
| Malay | 50 | 1.22 (0.62 to 2.43) | 0.57 |
| Indian and others | 39 | 1.04 (0.47 to 2.30) | 0.93 |
| Stream | |||
| Express | 225 | 1 (referent) | – |
| Normal academic | 91 | 1.12 (0.62 to 2.01) | 0.72 |
| Normal technical | 49 | 2.57 (1.28 to 5.15) | 0.008 |
| Last visit to eye care provider | |||
| <6 months ago | 162 | 1 (referent) | – |
| >6 months, <1 year ago | 110 | 1.20 (0.66 to 2.18) | 0.56 |
| >1 year, <2 years | 75 | 2.39 (1.29 to 4.44) | 0.006 |
| >2 years | 18 | 4.22 (1.38 to 12.88) | 0.012 |
*Adjusted for all other factors in the table and school.
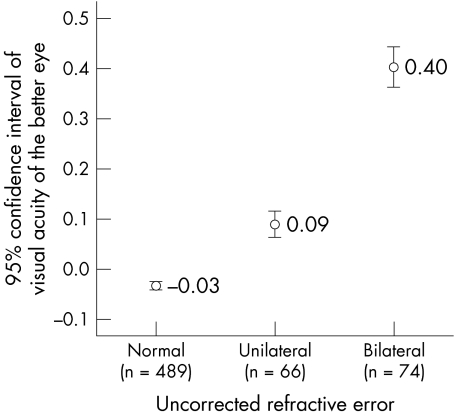
Figure 2 shows the impact of uncorrected refractive error on visual acuity. Among the 140 students who had uncorrected refractive error, 74 (52.9%, 95% confidence interval 44.6% to 61.1%) had the condition bilaterally. In terms of logMAR visual acuity of the better eye, students who had uncorrected refractive error bilaterally had mean visual acuity value of 0.40, while those who had the problem unilaterally and those who do not have uncorrected refractive error had mean visual acuity values of 0.09 and −0.03 respectively.
Figure 2 Relation between status of uncorrected refractive error and habitual visual acuity (logMAR).
Discussion
The reported uncorrected refractive error rate of 22.3% in grade 7 students is higher than those in reported in other countries, including the People's Republic of China (Shunyi District, 10.9%11 and Guangzhou, 10.215), Chile (La Florida, 14.7%12), Nepal (Mechi Zone, 2.8%13), India (Mahabubnagar District, 4.9%16 and New Delhi, 7.4%17), and South Africa (Durban, 2.7%18). Similar studies on adults revealed uncorrected refractive error rates of 6.1% in the Blue Mountains Eye Study in 2000,3 10% in the Melbourne and Rural Victoria Visual Impairment Project,2 6% in the Proyecto Visual Evaluation and Research,4 and 17.3% in the Tanjong Pagar Survey.1 Our higher rate could be attributed to the high refractive error rates in the Singapore population,6,8 and the very rapid progression rate of myopia seen in paediatric subjects.7 It also suggests that the problem is greater in the school age group. However, comparisons of uncorrected refractive error rates across studies could be limited by differences in the definition of uncorrected refractive error, refractive error techniques, target population, and sampling strategies.
Of the 140 students with uncorrected refractive error in our study, 52.9% had bilateral uncorrected refractive error. Visual acuity was poorer in students with unilateral uncorrected refractive error and, to a greater extent, in those with bilateral error (fig 2). In the RESC studies, proportions of children with baseline visual acuity worse than 20/32 bilaterally in China, Chile, and Nepal were 56.0%, 49.8%, and 43.4%, respectively.11,12,13 While a unilateral uncorrected refractive error could be compensated with the better eye, these results show that about half of the children with uncorrected refractive error have no means of compensation. These children are in urgent need of vision correction.
The educational stream showed significant association with the prevalence of uncorrected refractive error. The risk was the greatest among the normal technical students (crude odds ratio 1.84; 95% confidence interval 1.17 to 2.91). In the Proyecto Visual Evaluation and Research, 2002, having less than 13 years of education was a risk factor for uncorrected refractive error.4 In the Tanjong Pagar Survey, 2004, having fewer years of education was also a risk factor.1 In the Melbourne and Rural Victoria Visual Impairment Project, 1999, the lack of tertiary education predicted for uncorrected refractive error.2 A possible explanation for our results is that people with lower educational status may be less aware of the need for frequent visits to eye care providers. Therefore, the public should be educated about the necessity of regular screening visits, and the visual problems associated with uncorrected refractive error. The public education messages could be targeted at adults with lower educational levels.
This study also found that a dose‐response relation existed between the time interval since the last visit to an eye care provider and the prevalence rate of uncorrected refractive error among those who habitually wore optical devices. A similar association was identified among urban Chinese (Guangzhou) schoolchildren with less frequent refraction checkups.15 This was also reported in the Blue Mountains Eye Study among adults.3 Similarly, in the Proyecto Visual Evaluation and Research, 2002, people who had not seen an eye care provider in the past 2 years had higher risks of uncorrected refractive error.4 Because the progression of myopia is rapid in Singapore children,7 frequent visits to the eye care provider are necessary to optimally correct vision. Vision checks in the school could be performed once in 6 months rather than annually. In addition, parents should be encouraged to bring their child to see the optometrist at least once in 6 months.
Among different refractive errors, myopia had the strongest association with uncorrected refractive error in our study (crude odds ratio 4.54; 95% confidence interval 2.27 to 9.07). This result further highlights the issue of myopia as a direct cause of poor vision. Having a mixed refractive error had an even stronger association (crude odds ratio 5.57; 95% confidence interval 2.67 to 11.6) with uncorrected refractive error. Myopia is of special interest in Asia because the rates of myopia are among the highest in the world.6,7,8,9,10 The prevalence rate of myopia among the 629 grade 7 students in our study was 70.0%. Therefore, eye care providers should inform schoolchildren with myopia or mixed refractive error about their added risks of poor vision as a result of uncorrected refractive error and the importance of frequent and regular follow ups.
This study contributes to the scarce information on uncorrected refractive error prevalence rates and associated factors among school age children. The other strengths of our study include a high response rate of 99.8% because the schools involved in the study made the study part of their curriculum. Our study population was similar to the Singapore grade 7 (secondary one) student population.14
The lack of cycloplegic examination was one of the limitations of our study. In addition, ideally, random sampling of all grade 7 students in Singapore should have been carried out. Owing to logistic and time constraints, we chose two co‐education neighbourhood schools (such schools represent the majority of Singapore schools) that were in dissimilar locations in Singapore. Lastly, the presence of temporal bias in a cross sectional study also limits our ability to draw conclusions.
In summary, uncorrected refractive error is a sizeable problem (22.3%) among Singapore grade 7 students, more than half of whom had binocular uncorrected refractive error. This was more common among students with low academic ability, who had not visited any eye care provider for a long time, and who had myopia or mixed refractive error. Strategies to improve the uptake of spectacles in this population will be important.
Acknowledgements
We would like to thank all the medical students from the Community Health Project Group 5, 2005, who participated in this study: Kwek SC, M Adib BM, Nieh CM, Ong CWA, Wong XH, Xu X, Ng HXM, Ng P, Tan Y, Tong S, Wong SY, Yeo EMN, Chang M, Lie SA, Tan HYJ, Tan SM, Tay SK, Tham CA, Yeo JJC, Zhuang KD, Koh JC, Lim CL, Satkunanantham M, Poon YLE, Tan M, Wong SH, Cheow E, Huang ML, Ng YQA, S Radhziah BS, Tan LL, Wang LK, Zhang ZE. We would also like to thank Ms Yeo A and the final year Singapore Polytechnic optometry students who helped in data collection.
Abbreviations
RESC - Refractive Error Study in Children
SE - spherical equivalent
VA - visual acuity
Footnotes
Competing interests: none declared
We thank Helen Keller International Asia‐Pacific for the spectacle funds.
References
- 1.Saw S M, Foster P J, Gazzard G.et al Undercorrected refractive error in Singaporean Chinese adults: the Tanjong Pagar survey. Ophthalmology 20041112168–2174. [DOI] [PubMed] [Google Scholar]
- 2.Liou H L, McCarty C A, Jin C L.et al Prevalence and predictors of undercorrected refractive errors in the Victorian population. Am J Ophthalmol 1999127590–596. [DOI] [PubMed] [Google Scholar]
- 3.Foran S, Rose K, Wang J J.et al Correctable visual impairment in an older population: the blue mountains eye study. Am J Ophthalmol 2002134712–719. [DOI] [PubMed] [Google Scholar]
- 4.Munoz B, West S K, Rodriguez J.et al Blindness, visual impairment and the problem of uncorrected refractive error in a Mexican‐American population: Proyecto VER. Invest Ophthalmol Vis Sci 200243608–614. [PubMed] [Google Scholar]
- 5.World Health Organization Vision 2020 priority eye diseases: refractive error and low vision. www.who.int/pbd/blindness/vision_2020/priorities/en/index5.html (accessed 22 May 2005)
- 6.Seet B, Wong T Y, Tan D T.et al Myopia in Singapore: taking a public health approach. Br J Ophthalmol 200185521–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saw S M, Tong L, Chua W H.et al Incidence and progression of myopia in Singaporean school children. Invest Ophthalmol Vis Sci 20054651–57. [DOI] [PubMed] [Google Scholar]
- 8.Au Eong K G, Tay T H, Lim M K. Education and myopia in 110,236 young Singaporean males. Singapore Med J 199334489–492. [PubMed] [Google Scholar]
- 9.Law N M, Chew S J, Ritch R. Survey of refraction in a Chinese population shows that myopia severity can be predicted from its age of onset. Invest Ophthalmol Vis Sci 199233(suppl)709S [Google Scholar]
- 10.Wu H M, Yap E P H, Seet B.et alReport on the study of myopia and its impact in a cohort of Singapore Armed Forces enlistees. Singapore: Defence Medical Research Institute, 1998
- 11.Zhao J, Pan X, Sui R.et al Refractive Error Study in Children: results from Shunyi District, China. Am J Ophthalmol 2000129427–435. [DOI] [PubMed] [Google Scholar]
- 12.Maul E, Barroso S, Munoz S R.et al Refractive Error Study in Children: results from La Florida, Chile. Am J Ophthalmol 2000129445–454. [DOI] [PubMed] [Google Scholar]
- 13.Pokharel G P, Negrel A D, Munoz S R.et al Refractive Error Study in Children: results from Mechi Zone, Nepal. Am J Ophthalmol 2000129436–444. [DOI] [PubMed] [Google Scholar]
- 14.Ministry of Education Education Statistics Digest 2004. Singapore 2005
- 15.He M, Xu J, Yin Q.et al Need and challenges of refractive correction in urban Chinese school children. Optom Vis Sci 200582229–234. [DOI] [PubMed] [Google Scholar]
- 16.Dandona R, Dandona L, Srinivas M.et al Refractive error in children in a rural population in India. Invest Ophthalmol Vis Sci 200243615–622. [PubMed] [Google Scholar]
- 17.Murthy G V, Gupta S K, Ellwein L B.et al Refractive error in children in an urban population in New Delhi. Invest Ophthalmol Vis Sci 200243623–631. [PubMed] [Google Scholar]
- 18.Naidoo K S, Raghunandan A, Mashige K P.et al Refractive error and visual impairment in African children in South Africa. Invest Ophthalmol Vis Sci 2003443764–3770. [DOI] [PubMed] [Google Scholar]