Abstract
Aim
To examine the association between epilation and corneal opacity (CO) among trichiasis patients presenting for surgery.
Methods
Cross sectional data from the STAR trial were utilised. Patients presenting for trichiasis surgery in Wolayta Zone, Ethiopia, were evaluated for current trichiasis status. Number of inturned lashes, evidence of epilation, level of entropion, trichiasis duration, and CO were collected. The primary outcome was prevalence of CO, stratified by entropion and epilation status.
Results
Approximately 10% of eyes with mild entropion had CO, regardless of epilation status. Among eyes with moderate entropion, epilated eyes were less likely to have CO than non‐epilated eyes (21% v 34% p = 0.002). The same association was seen in eyes with severe entropion: 43% of epilated eyes while 74% of non‐epilated eyes had CO (p<0.0001). Presence of CO increased with age. Adjusted models showed a protective effect of epilation in eyes with moderate or severe entropion (OR: 0.51; 95% CI: 0.32 to 0.83 and OR: 0.24; 95% CI: 0.13 to 0.45, respectively). Among eyes with mild entropion there was no difference in the prevalence of CO comparing eyes that were epilated with those that were not epilated.
Conclusion
Entropion was the most significant predictor of CO. Cross sectional associations suggest that epilation may not be helpful for eyes with mild entropion, but may offer protection against CO in eyes with moderate to severe entropion. Epilation should not be a substitute for trichiasis surgery, however, as 43% of eyes with severe entropion that were epilated still had CO.
Keywords: epilation, corneal opacity, trichiasis, Ethiopia, STAR trial
Trachoma remains the leading infectious cause of blindness worldwide, with over 1.3 million individuals currently blind.1 Years of repeated infection with Chlamydia trachomatis cause scarring which can result in the lid rotating inward (entropion) and the lashes abrading the cornea (trichiasis). If not corrected, corneal opacity (CO) and eventually blindness may result. A simple surgical procedure, the bilamellar tarsal rotation procedure (BTRP), has been endorsed by the World Health Organization to correct trichiatic lashes. The WHO recommends that if one or more inturned lashes are touching the cornea surgery should be performed, regardless of the total number of lashes touching the globe.2 Surgical uptake varies substantially by country, with as many as 80% of individuals not presenting for surgery.3,4,5
Trachoma control programmes are in need of alternative measures for individuals who refuse surgery, and some programmes have suggested epilation as an effective method for preventing corneal opacity. In addition, in some countries trichiasis surgery is not recommended until at least five lashes are touching the globe. For example, in the Gambia, surgery is not recommended until at least five lashes are touching the globe, and individuals are instructed to epilate until this point.6,7 To date, however, no studies have examined the effects of epilation on corneal opacity. A large cohort of patients presenting for trichiasis surgery in southern Ethiopia provided the opportunity to evaluate the cross sectional association between epilation and corneal opacity.
Methods
This study relies on data from the Surgery for Trichiasis, Antibiotics to prevent Trichiasis (STAR) trial, a clinical trial of 1452 patients who presented for trichiasis surgery in the Wolayta Soddo Zone of southern Ethiopia. The STAR trial aims to evaluate the role of antibiotic treatment for trachoma at the time of trichiasis surgery on reducing recurrence up to 1 year following surgery. Trichiasis surgery had not been available in this area before the trial. A detailed description of the data collection methods for the trial is provided elsewhere.8 Briefly, all patients aged ⩾18 years presenting for trichiasis surgery with unoperated trichiasis in at least one eye were evaluated for previous lid surgery and current trichiasis status. Participants were also asked the duration of the lashes rubbing their eyes. Duration was categorised as less than 6 months, 6 months to less than 1 year, 1 year to less than 2 years, and 2 years or more.
Trichiasis was evaluated using a torch light with the patient in a shaded location, with eyes in primary gaze. The number of lashes touching any part of the globe, the number specifically touching the cornea, and the location of trichiatic lashes were recorded. The number of lashes was counted up to 10 lashes. When eyes had more than 10 lashes touching, “10” was recorded. Evidence of epilation was recorded as present or absent. Evidence of epilation was strictly based on the grader visualising eyelash bases where the lash had been removed, short lash stubs that were growing back in, or broken lashes indicating incomplete epilation. Eyes were classified as “completely epilated” if evidence of epilation was present and no lashes were touching the globe. If epilation was present and at least one lash or stub was touching the globe, the eye was classified as “incompletely epilated.” Entropion status was evaluated using a previously validated detailed grading in which interobserver agreement was 0.82.9 Entropion was classified into one of three categories: mild, moderate, or severe. Full descriptions of these categories are provided in table 1. Entropion was evaluated with the grader looking straight at the participant. Corneal opacity (CO) was graded as present if there was an easily visible CO, which obscured at least part of the pupillary margin, in accordance with the WHO definition.10 Given that one grader evaluated all characteristics of trichiasis, including lashes touching the globe, evidence of epilation and entropion status, the grader was not masked to any of these three individual characteristics.
Table 1 Entropion classification9.
| Entropion classification | Description of classification |
|---|---|
| Mild | All lash bases visible in the region with trichiasis |
| Moderate | One or more lash bases inturned, but some bases still visible in the region with trichiasis |
| Severe | All lash bases not visible in the region with trichiasis |
Severity of trichiasis is frequently defined by the number of trichiatic lashes touching the globe. For this study, this classification was not feasible, as a large percentage of individuals were epilating, and epilation prevents accurate counting of the number of lashes that would be touching the globe if they were present. Thus, we defined severity based on the degree of entropion. Among eyes without epilation, tests were conducted to examine the correspondence of our classification to the number of lashes touching the globe.
Frequency tables and χ2 tests were used to assess bivariate associations. Multivariate analyses were conducted at the eye level. Logistic regression models were used to evaluate the association between each risk factor and corneal opacity. To account for the correlation between eyes of an individual, standard errors were corrected using the generalised estimating equation (with exchangeable correlation structure) approach. These analyses were conducted using the GENMOD procedure (SAS version 8.0, Cary, NC, USA).11 The Mantel‐Haenszel χ2 test was used to test for trends, specifically, to evaluate whether there was a trend regarding the relation between duration of lashes and degree of entropion.
The Johns Hopkins Medical Institutions joint committee on clinical investigation and the Ethiopia Science and Technology Commission's national ethical clearance committee approved all study procedures. All study procedures met the tenets of the Declaration of Helsinki.
Results
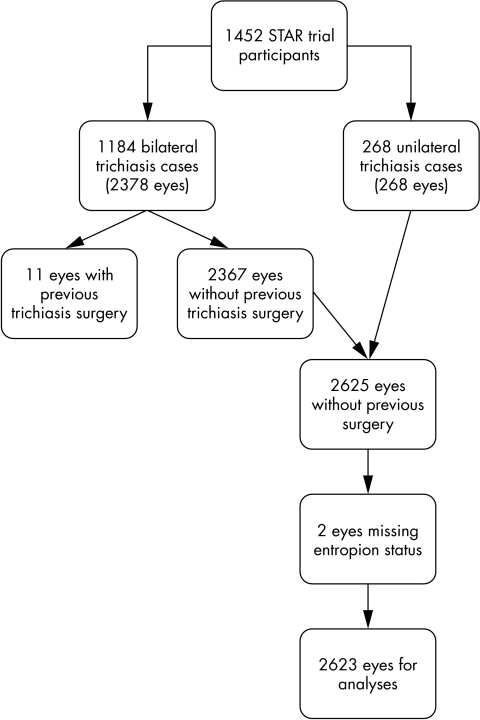
Of the 1452 individuals enrolled in the STAR trial, 82% presented with bilateral trichiasis; 11 eyes of bilateral cases had been previously operated and two eyes were missing entropion information, leaving 2623 eyes with unoperated trichiasis for our analyses (fig 1). Characteristics of our cohort are presented in table 2. Among eyes with unoperated trichiasis, 783 (30%) had moderate entropion and 426 (16%) had severe entropion. Corneal opacity was present in 21% of eyes with unoperated trichiasis (table 2). The median number of lashes touching the globe in eyes without epilation was six, indicating the severity of disease in this population. Among eyes with evidence of epilation and at least one lash touching the globe, the median number of lashes touching was also six.
Figure 1 Flow diagram of eyes included in epilation analyses.
Table 2 Characteristics of 2623 eyes with unoperated trichiasis.
| Characteristic | No (%) | |
|---|---|---|
| Trichiasis duration 2+ years | 2404 (92) | |
| Evidence of epilation | 1815 (69) | |
| Entropion: | ||
| Mild | 1414 (54) | |
| Moderate | 783 (30) | |
| Severe | 426 (16) | |
| Median number of lashes touching globe, among non‐epilated eyes (n = 808) | 6 | |
| Corneal opacity | 538 (21) |
Good correlation existed between number of trichiatic lashes and degree of entropion among eyes with no evidence of epilation (table 3, p<0.0001). Only 30% of eyes with mild entropion had seven or more lashes touching the globe; while 80% and 98% of eyes with moderate and severe entropion, respectively, had seven or more trichiatic lashes. Thus, entropion served as an appropriate indicator of trichiasis severity. At all levels of entropion, over 50% of eyes had evidence of epilation; 59% of eyes with mild entropion and 76% of eyes with severe entropion were epilated.
Table 3 Entropion as an indicator of trichiasis severity among eyes with no evidence of epilation.
| Entropion | No | % (n) with 7+ lashes touching globe | % (n) with 1+ lashes touching cornea |
|---|---|---|---|
| Mild | 585 | 29.7 (174) | 86.5 (505) |
| Moderate | 122 | 79.5 (97) | 95.1 (116) |
| Severe | 101 | 98.0 (99) | 100.0 (101) |
| Total | 808 | 45.8 (370) | 89.5 (722) |
Comparing eyes with mild entropion that were epilated with eyes that were not epilated, there was no statistically significant difference in the percentage of eyes with corneal opacity, 8.9% v 10.9%, respectively (p = 0.23); however, there was a statistically significant reduction in the frequency of CO among epilated eyes with moderate or severe entropion compared to non‐epilated eyes (table 4). Not surprisingly, the overall association between epilation and CO was attenuated due to the substantial size of the mild entropion group (1414 eyes) and the lack of association in that subgroup.
Table 4 Percentage of eyes with corneal opacity according to entropion status.
| Entropion | No | % with corneal opacity | p Value | |
|---|---|---|---|---|
| Not epilating | Epilating | |||
| Mild | 1414 | 8.9 | 10.9 | 0.23 |
| Moderate | 783 | 34.4 | 21.3 | 0.002 |
| Severe | 426 | 74.0 | 42.8 | <0.0001 |
| Total | 2623 | 20.8 | 20.4 | 0.80 |
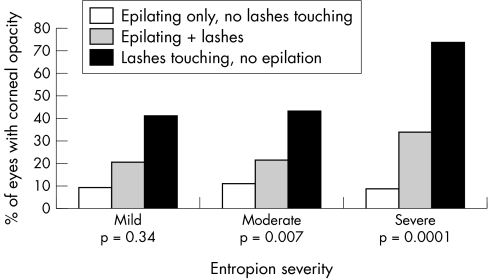
Many eyes (1203) still had lashes touching the globe, although evidence of epilation also was present. In each category of entropion severity, eyes with lashes touching and evidence of epilation (that is, incomplete epilation) were less likely to have CO than eyes with no evidence of epilation (fig 2). These eyes, which were not completely epilated, were more similar to eyes that were completely epilated than to eyes with no evidence of epilation.
Figure 2 Corneal opacity according to epilation success and level of entropion.
Separate multivariate models were developed for each of the three entropion categories (table 5). These age and sex adjusted models accounting for the correlation between eyes suggest that epilation has a protective effect against CO among eyes with moderate (OR: 0.51; 95% CI = 0.32 to 0.83) or severe entropion (OR: 0.24; 95% CI = 0.13 to 0.45) but is not protective for eyes with mild entropion (table 5). For each five year increase in age, there was a 12–15% increase in odds of CO for each of the three entropion categories. Females were not more likely to have CO than males. Duration of trichiasis was a risk factor for CO in eyes with mild entropion (test for trend p<0.05); however, since nearly 98% of eyes with moderate or severe entropion reported duration of more than two years, the association between duration of trichiasis and CO could not be assessed in these two models.
Table 5 Odds ratios (95% confidence intervals) for the adjusted association between potential risk factors and corneal opacity (multivariate analyses, stratified by entropion status)*.
| Covariate | Mild | Moderate | Severe |
|---|---|---|---|
| Epilation | 1.12 (0.75 to 1.68) | 0.51 (0.32 to 0.83) | 0.24 (0.13 to 0.45) |
| Age (5 year increments) | 1.12 (1.03 to 1.22) | 1.13 (1.04 to 1.22) | 1.15 (1.05 to 1.27) |
| Female | 1.11 (0.69 to 1.79) | 0.71 (0.44 to 1.14) | 0.70 (0.35 to 1.89) |
| Duration of trichiasis: | |||
| <1 year | 1.0 (reference)† | NA | NA |
| 1−<2 years | 1.35 (0.25 to 7.33)† | NA | NA |
| 2+ years | 2.73 (0.64 to 11.69)† | NA | NA |
*Adjusted for correlation between eyes using generalised estimating equations.
†Mantel Haenszel test for trend, p<0.05.
Discussion
In this cross sectional evaluation, eyes with moderate or severe entropion that were epilated were less likely to have CO than eyes that were not epilated. Among eyes with mild entropion, epilation did not appear to offer protection against corneal opacity; however, CO was less common among both epilated and non‐epilated eyes compared to eyes with moderate or severe entropion. To our knowledge, this study is the first to evaluate the association between epilation and CO among eyes with trachomatis trichiasis. Our analyses are based on a large patient population where epilation is commonly practised.
In many settings, trichiasis severity is measured by counting the number of trichiatic lashes touching the globe. However, in the presence of epilation, the number of lashes rubbing the globe may not provide an accurate descriptor of trichiasis severity as individuals may epilate an entire section of the lid, without regard to which lashes are actually touching the globe. We have demonstrated that among non‐epilated eyes, the number of lashes touching the globe and the degree of entropion were highly correlated; therefore, entropion provides an adequate severity measure for this study. It is possible that eyes which are completely epilated may be more difficult to categorise as moderate versus severe; however, we doubt that this possibility would have an important effect on our results, as an analysis combining these two groups still showed a statistically significant reduction in the frequency of CO comparing epilated eyes with non‐epilated eyes (p<0.0001).
While this study provides a critical first step in evaluating the relation between epilation and corneal opacity, it has limitations that must be recognised. These analyses are based on cross sectional data which showed a protective association of epilation in eyes with moderate or severe entropion. However, current epilation practice may not provide a completely accurate marker of previous epilation history. Individuals with severe entropion and/or severe CO may have previously practised epilation but stopped epilating for several reasons. These individuals may have given up the practice of epilating, thinking that it was futile. Alternatively, they may have stopped because the opacity was so severe that it no longer helped their vision to epilate, or the cornea may have become numb and the individual no longer able to feel the sharp lashes abrading the cornea. No studies to date, however, have examined this possibility.
Our method for assessing epilation provides an accurate descriptor of whether or not the patient was epilating, but does not provide information on the extent of epilation. We intentionally collected epilation data as a binomial variable, as we think that more detailed information may not provide an accurate characterisation of the trichiatic lashes that would have been present in the absence of epilation. When individuals have several inturned lashes and practise epilation, they are likely to remove more lashes than just those that are touching the globe in primary gaze. Thus, it is difficult to accurately ascertain the degree of epilation that corresponds to trichiatic lashes. One could roughly assess the extent of epilation (for example, based on a rough description of the extent of the lid that is epilated), but this convention would not be directly comparable to the current practice of defining severe trichiasis as having 5+ lashes touching the globe. This information was not collected for this study. However, our data demonstrate that entropion provided an accurate descriptor of severity of trichiasis because of the correlation between number of lashes touching the globe and degree of entropion among eyes that did not have evidence of epilation.
Longitudinal studies would be necessary to overcome most of the limitations associated with this study. Such studies would afford the opportunity to periodically evaluate epilation practices including frequency, extent of epilation, and epilation success (that is, whether lashes are completely removed or broken off during the process of epilating). To conduct such studies, however, would first require development of reliable, more extensive tools for evaluating trichiasis progression because the current tools for assessing progression do not allow for detection before visually significant complications develop. Currently, CO is the only available outcome measure that would allow assessment of the effectiveness of epilation on reducing long term visual impairment, and this measurement does not necessarily provide an ethically sound measure for evaluating epilation success. Such studies also would require extensive human resources to frequently monitor epilation practices and to ensure that individuals did not progress to significant visual impairment. Future studies are needed that incorporate new evaluation tools.
In summary, these data provide a first look at the cross sectional association between epilation and corneal opacity. The data suggest that epilation may offer some protection against CO among eyes with moderate to severe entropion. If individuals consistently refuse surgery, trachoma control programmes may recommend epilation as a means of potentially reducing progression to corneal opacity. If such recommendations are made, they should be accompanied by detailed instructions on how to epilate to remove the entire lash and prevent lashes from breaking off. Epilation should not, however, on the basis of this study, be a substitute for surgery, since a significant proportion of epilated eyes with severe entropion have corneal opacity. These data suggest that epilation may not be helpful for eyes with mild entropion. This lack of an association has potential ramifications for countries that recommend delaying surgery. Before such conclusions can be drawn, however, further research into the role of epilation in preventing CO needs to be conducted.
Acknowledgements
The authors gratefully acknowledge the funding provided for this project by the National Eye Institute, National Institutes of Health, grant number EY13878. In addition, the authors would like to thank the STAR trial research team and the trichiasis surgery patients in Wolayta Zone, Ethiopia, for their participation.
Abbreviations
BTRP - bilamellar tarsal rotation procedure
CO - corneal opacity
STAR trial - Surgery for Trichiasis, Antibiotics to prevent Trichiasis trial
Footnotes
Competing interests: none declared
Presented in part as a poster at the Association for Research in Vision and Ophthalmology Meeting, May 2005, Ft Lauderdale, FL, USA.
References
- 1.Resnikoff S, Pascolini D, Etya'ale D.et al Global data on visual impairment in the year 2002. Bull World Health Organ 200482844–851. [PMC free article] [PubMed] [Google Scholar]
- 2.Reacher M H, Foster A, Huber M J.Trichiasis surgery for trachoma the bilamellar tarsal rotation procedure. New York: World Health Organization Programme for the Prevention of Blindness, 1993
- 3.Oliva M S, Munoz B, Lynch M.et al Evaluation of barriers to surgical compliance in the treatment of trichiasis. Int Ophthalmol 199721235–241. [DOI] [PubMed] [Google Scholar]
- 4.Bowman R J, Faal H, Jatta B.et al Longitudinal study of trachomatous trichiasis in the Gambia: barriers to acceptance of surgery. Invest Ophthalmol Vis Sci 200243936–940. [PubMed] [Google Scholar]
- 5.West S, Lynch M, Munoz B.et al Predicting surgical compliance in a cohort of women with trichiasis. Int Ophthalmol 199418105–109. [DOI] [PubMed] [Google Scholar]
- 6.Bowman R J, Faal H, Jatta B.et al Longitudinal study of trachomatous trichiasis in the Gambia: barriers to acceptance of surgery. Invest Ophthalmol Vis Sci 200243936–940. [PubMed] [Google Scholar]
- 7.Bowman R, Faal H, Jatta B.et al Longitudinal study of trachomatis trichiasis in the Gambia. Br J Ophthalmol 200286339–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.West E S, Alemayehu W, Munoz B.et al Surgery for trichiasis, Antibiotics to Prevent Recurrence (STAR) Clinical Trial Methodology. Ophthalmic Epidemiol 200512279–286. [DOI] [PubMed] [Google Scholar]
- 9.Melese M, Alemayehu W, Bejiga A.et al Modified grading system for upper eyelid trachomatous trichiasis. Ophthalmic Epidemiol 20031075–80. [DOI] [PubMed] [Google Scholar]
- 10.Thylefors B, Dawson R, Jones B R.et alA simple system for the assessment of trachoma and its complications. 65 ed 1987 [PMC free article] [PubMed]
- 11.Liang K, Zeger S. Longitudinal data analysis using generalized linear models. Biometrika 19867313–22. [Google Scholar]