The commonest cause of solar retinopathy is direct viewing of a solar eclipse.1 Other associations include sun gazing during religious rituals, drug or alcohol intoxication, and mental illness.2,3 However, it may not be considered in the absence of a history of sun gazing. We report an unusual case of solar retinopathy in a patient with bipolar affective disorder and demonstrate the value of optical coherence tomography in aiding the diagnosis in cases of unexplained visual loss in patients with mental illness.
Case report
A 45 year old woman presented complaining of a gradual deterioration in vision over 3 years. Past medical history included hypothyroidism and bipolar affective disorder treated with antidepressant and antipsychotic medication.
Presenting visual acuities were 6/12 in the right eye and 6/9 in the left. In the centre of the fovea in both eyes there was a small, irregular 100 μm size red spot without oedema (fig 1). Fluorescein angiogram was normal. Optical coherence tomography (OCT) was performed bilaterally using a Zeiss Stratus model 3000, with the scanning line centred manually on the area of foveal disturbance. Both eyes showed similar findings with multiple slices at different angles revealing a single spot of hyporeflectivity in the outer retina, suggesting discontinuity in the photoreceptor outer segment layer (fig 2).

Figure 1 Colour photograph depicting stage 1 macular hole‐like appearance.
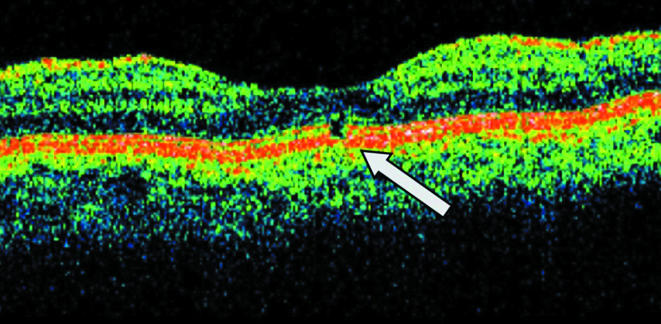
Figure 2 A 3 mm Stratus OCT single line scan through fixation. Arrow indicating hyporeflectivity in photoreceptor outer segment layer suggesting discontinuity.
The OCT appearance suggested a diagnosis of solar retinopathy and on direct questioning the patient admitted to staring at the sun for prolonged periods of time during depressive phases of her illness and during solar eclipses.
Comment
Classically, solar retinopathy presents soon after the initial insult with symptoms including reduced visual acuity, central scotoma, chromatopsia, photophobia, and metamorphopsia. Acutely, there may be loss of the foveal reflex together with a small yellow‐white spot near the foveola which gradually fades. A longstanding lesion may only show an irregularly pigmented macula with foveal hypopigmentation.3
Differential diagnoses include early macular hole, lamellar hole, macula dystrophy, or cystoid macular oedema.3 Fluorescein angiography may help to differentiate these. However there is often little or no abnormality in solar retinopathy, although in severe cases there may be a window defect caused by retinal pigment epithelium (RPE) atrophy.2
OCT findings in acute solar retinopathy were first described by Codenotti et al.4 OCT studies in chronic solar retinopathy describe hyporeflective spaces at the level of the outer photoreceptor segments and RPE. These may involve the entire photoreceptor layer in more severe cases, together with overlying neurosensory thinning.5,6
Our patient would not initially volunteer a history of sun gazing but admitted to this when told the OCT findings. Similar OCT findings can be seen in stage 1 macular hole, but these findings in combination with a history of sun gazing are strongly suggestive of a diagnosis of solar retinopathy. Sun gazing has been described in a patient with bipolar disease during a manic episode with psychotic symptoms, although there was no evidence of alteration of visual function or macular damage.7 Previous reports have mainly been associated with schizophrenia.8,9 Patients presented acutely, as acute or chronic episodes with repeated sun gazing, or were found to have a typical macular lesion incidentally. In chronic cases they gave a history of sun gazing during acute episodes of illness.
To our knowledge this is the first documented case of solar retinopathy in a patient with bipolar affective disorder. This case demonstrates the benefits of OCT in the diagnosis of macular diseases where the history may be unreliable. It also highlights the need to consider the diagnosis of solar retinopathy in a range of psychiatric conditions where there is functional visual loss.
Footnotes
Competing interests: none declared
References
- 1.Rai N, Thuladar L, Brandt F.et al Solar retinopathy. A study from Nepal and Germany. Doc Ophthalmol 19989599–108. [DOI] [PubMed] [Google Scholar]
- 2.Michaelides M, Rajendram R, Marshall J.et al Eclipse retinopathy. Eye 200115148–151. [DOI] [PubMed] [Google Scholar]
- 3.Thomas J W, Stokkermans O D, Dunbar T M. Solar retinopathy in a hospital based primary care clinic. J Am Optom Assoc 199869625–636. [PubMed] [Google Scholar]
- 4.Codenotti M, Patelli F, Brancato R. OCT findings in patients with retinopathy after watching a solar eclipse. Ophthalmologica 2002216463–466. [DOI] [PubMed] [Google Scholar]
- 5.Jorge R, Costa R A, Quirino L S. Optical coherence tomography findings in patients with late solar retinopathy. Am J Ophthalmol 2004371139–1143. [DOI] [PubMed] [Google Scholar]
- 6.Garg S J, Martidis A, Nelson M L.et al Optical coherence tomography of chronic solar retinopathy. Am J Ophthalmol 2004137351–354. [DOI] [PubMed] [Google Scholar]
- 7.Kamp P S, Dietrich A M, Rosse R B. Sungazing by psychiatric patients. Am J Psychiatry 1990147810–811. [DOI] [PubMed] [Google Scholar]
- 8.Galainena M L. Solar retinopathy. Ann Ophthalmol 19768304–306. [PubMed] [Google Scholar]
- 9.Anaclerio A M, Wicker S H. Self induced solar retinopathy by patients in a psychiatric hospital. Am J Ophthalmol 197069731–736. [DOI] [PubMed] [Google Scholar]


