Abstract
Aims
To prospectively study the evolution of possible high risk features of conjunctival filtration blebs like avascularity, transconjunctival oozing (TCO), and leaks after mitomycin C (MMC) enhanced glaucoma surgery.
Methods
Single observer, 2 year prospective study on bleb characteristics of 125 eyes of 125 consecutive patients who had MMC augmented glaucoma surgery with initially successful filtration. MMC (0.2 mg/ml for 2 minutes in most cases) was applied on the area of the scleral flap before dissection. Glaucoma surgeries included were trabeculectomy, deep sclerectomy, and combined procedures. A dry fluorescein strip was applied on the avascular part of the bleb and observed for aqueous egress with flow (point leak, PL) or without (TCO).
Results
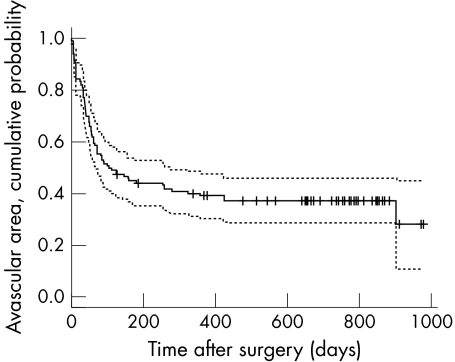
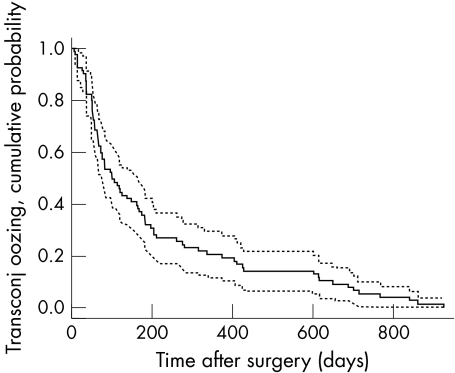
The mean time (95% CI) for observing bleb avascularity, TCO, and bleb leaks were 106 days (69 to 143), 208 days (155 to 261), and 609 days (559 to 659), respectively. Bleb leaks were observed in 17 eyes (13.6%)—15 (24.6%) in the trabeculectomy group and two (3.1%) in the deep sclerectomy group (p = 0.003). Kaplan‐Meier survival analyses showed that the probability of observing bleb avascularity at sixth, 12th, and 24th month after surgery was 56%, 71%, and 73%, respectively. In eyes with avascular blebs, the probability of developing TCO and leaks was 77% and 1% at 6 months, 81% and 12% at 12 months, and 95% and 26% at 24 months, respectively. Cox's regression analyses and log rank tests showed that eyes with larger avascular blebs (>4 mm) were more likely to develop TCO (hazard ratio 3.77, p = 0.001) and delayed bleb leaks were more likely to be seen in eyes of the trabeculectomy group rather than the deep sclerectomy group (hazard ratio 0.06, p = 0.0006).
Conclusions
MMC application over the area of scleral flap dissection during glaucoma surgery is associated with a high incidence of bleb avascularity, TCO, and delayed bleb leaks. Most eyes developed bleb avascularity within the first year after surgery. TCO will eventually be seen in all eyes with avascular blebs and the incidence of leaks gradually increases with time. This study shows that patients with eyes undergoing glaucoma surgery with MMC and avascular blebs should be monitored indefinitely.
Keywords: mitomycin C, transconjunctival oozing
The use of wound healing modifying agents like 5‐fluorouracil (5‐FU) and mitomycin C (MMC) has significantly enhanced the outcomes of glaucoma surgery.1,2,3,4,5,6,7,8 However, this has been achieved at the expense of avascular conjunctival filtering blebs and consequent transconjunctival oozing (TCO) or bleb “sweating,” delayed bleb leaks, hypotony, cataracts, severe visual loss, bleb infections, and endophthalmitis.1,2,5,9,10,11,12,13,14,15,16,17,18,19,20,21 Histological studies of MMC blebs show irregular surface epithelium and a largely avascular and acellular subepithelium of loosely arranged connective tissue.22,23,24,25 These findings may explain TCO and delayed bleb leaks seen frequently after MMC augmented glaucoma surgery.11,12,15,16,17
In a large cross sectional study from Japan on eyes with trabeculectomy, TCO was observed only in avascular areas of bleb; 11.9% of all blebs showed TCO. Eyes with larger avascular areas were prone to point leaks and eyes that had postoperative 5‐FU supplementation were more likely to show TCO. Eyes with TCO had lower intraocular pressure (IOP).26 The same authors in a another report on primary MMC enhanced trabeculectomies (MMC 0.4 mg/ml for 3 minutes) noted that bleb avascularity was observed in 97%, TCO in 36%, and leakage in 5.6% of eyes.16 The purpose of this study was to report the evolution of these high risk features (avascular areas, transconjunctival oozing, and leaks) on conjunctival filtering blebs after MMC augmented glaucoma surgery.
Methods
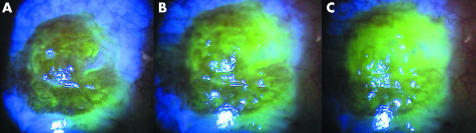
Consecutive patients undergoing MMC enhanced glaucoma surgery between April 2002 and March 2003 were included in the study. All surgeries were performed or supervised by one surgeon (NA). The techniques for trabeculectomy, deep sclerectomy, and combined surgery are described elsewhere.27,28 The MMC application technique was similar as shown in figure 1. In all cases, a fornix based conjunctival flap was performed. MMC was applied on the sclera over the proposed sclera flap site (approximately 25 mm2). Two to four collagen sponges (Visitec, UK) soaked in MMC, were applied in the subconjunctival space taking care to avoid the sponges touching the conjunctival flap edges (fig 1). After removal of the sponges, the area was irrigated by 20 ml of balanced salt solution. The duration and concentration of MMC was decided on the basis of risk factors for failure. The duration of application was also modified by the surgeons on operative findings like excessive subconjunctival fibrosis or bleeding while dissecting the conjunctival flap. Postoperative management included a topical steroid‐antibiotic combination four to six times daily for at least 6 weeks and longer depending on bleb appearance. In the trabeculectomy group suture release was done if required in the early postoperative period. Subconjunctival 5‐FU (5 mg) was administered in cases of incipient bleb failure and slit lamp needle revision with subconjunctival 5‐FU 5 mg was done in eyes with bleb failure. In the deep sclerectomy group usually Nd:YAG laser goniopuncture was attempted before any attempts at needle revision.
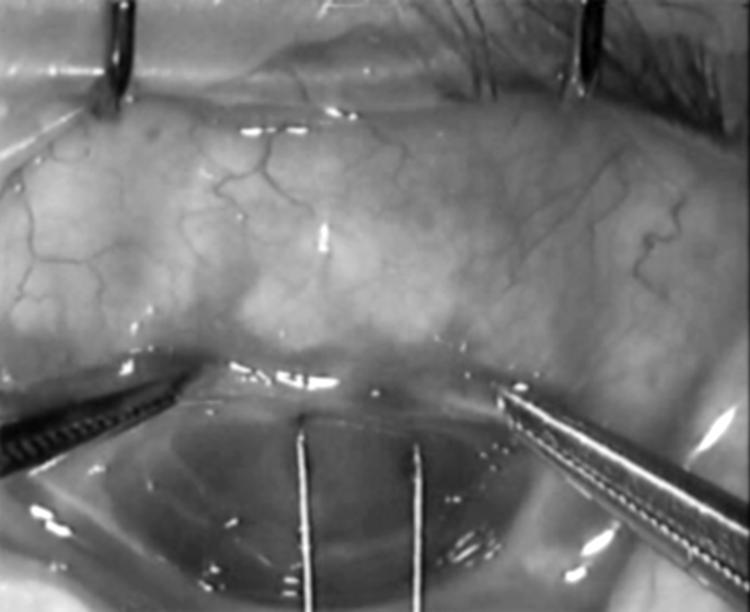
Figure 1 Technique for MMC application on sclera after dissection of a fornix based conjunctival flap.
Surgeries were divided into two broad categories—trabeculectomy and deep sclerectomy. Deep sclerectomies complicated by intraoperative perforation were included in the trabeculectomy group. In patients who had surgery in both eyes, the eye that underwent surgery first was included in the study. Frequency of postoperative visits was determined on an individual basis. Visual acuity, IOP, and slit lamp findings were recorded for each patient and were entered on a correlational database (Microsoft Access). All observations on bleb morphology were confirmed by one observer (NA).
Technique for bleb examination
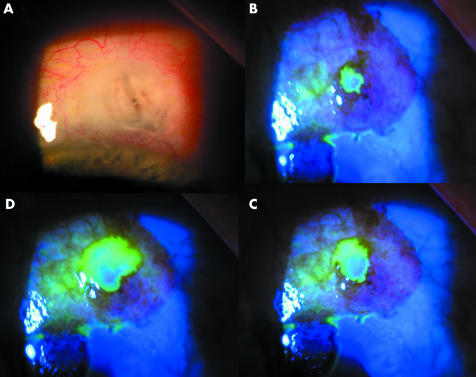
A careful slit lamp examination under high magnification (16 ×) for subconjunctival blebs was performed on each postoperative visit. The following bleb characteristics were noted on each visit—bleb location, height, extent, vascularity, and the presence or absence of microcysts. An avascular area was defined as an area within a bleb devoid of blood vessels and had either a transparent, multiloculated (cystic) or succulent appearance. The greatest extent of the avascular area was measured by a focused slit beam and avascular areas were placed in three categories—less than 4 mm, 4–8 mm, and more than 8 mm. The blebs were checked for leaks initially by instilling a drop of fluorescein and looking for an aqueous stream (Seidel's sign). Transconjunctival oozing (bleb sweating) and point leak were tested by asking the patient to look inferiorly, application of a dry sterile fluorescein strip on the avascular area, and observation under cobalt blue slit lamp illumination for 30 seconds. Transconjunctival oozing was identified as increasing fluorescence on the bleb surface without any apparent interruption of the conjunctival tissue or aqueous stream on the bleb wall (fig 1). A point leak was manifested by a spontaneous visible flow of aqueous (fig 2). While various bleb characteristics were recorded, the emphasis in this report is on high risk features such as bleb avascularity, TCO, and leaks.
Figure 2 Transconjunctival oozing. A dry fluoroscein strip is gently applied on the avascular bleb with the patient looking downwards. This series was taken within 30 seconds showing the characteristic increase in fluorescence with no flow of aqueous.
The protocol envisaged inclusion of eyes with blebs that showed evidence of aqueous filtration 3 months after surgery. This implied that if no filtration was present or if the blebs failed despite intensive postoperative management, the eye was excluded. Successful filtration was defined as the observation of a diffuse elevated subconjunctival area and the presence of subconjunctival microcysts. Signs of bleb failure were as for trabeculectomy—disappearance of subconjunctival microcysts, increasing vascularity, decreasing area of the bleb, and increasing IOP on serial examination. Failed blebs were localised or flat with no subconjunctival microcysts and an elevated IOP.
Statistical methods
The probability for observing the aforementioned bleb characteristics was done by Kaplan‐Meier survival analyses with 95% confidence intervals (Greenwood's method). If needle revision or any other procedure to lower IOP was done after 3 months postoperatively, survival data were censored at the time the procedure was done. A Cox regression model was used to determine the effect of various factors on the survival curves. For regression a p value 0.001 or less was considered as statistically significant. Factors found to be statistically significant by Cox's regression were retested by the univariate log rank test. Dichotomous variables were analysed using the χ2 test with Yates's correction and Fisher's exact test. Non‐parametric data were analysed by the Wilcoxon's matched pairs test. These tests were two tailed and p values less than 0.05 were taken to be significant.
Results
In all, 125 eyes of 125 patients were included in the study from 144 MMC augmented surgeries between April 2003 and March 2004. Eight eyes, six from the trabeculectomy and two from the deep sclerectomy group, were excluded because of bleb failure within 3 months of surgery. Nine eyes were excluded for being the second eye of the same patient. Two patients died within 4 months after surgery and were hence excluded. Demographic and preoperative details are shown in table 1. Thirty three eyes (26.4%) had previous surgery—28 (42.6%) from the trabeculectomy group and four (6.2%) from the deep sclerectomy group (p<0.001). In eyes with previous surgery the MMC regimens used were as follows: MMC 0.4 mg/ml for 3 minutes in three eyes (9.1%), 0.2 mg/ml for 2 minutes in 15 eyes (45.4%), and 0.2 mg/ml for 3 minutes in 12 eyes (36.4%). The mean time (95% confidence intervals) for observing bleb avascularity, TCO, and point leak (PL) were 106 days (69 to 143), 208 days (155 to 261), and 609 days (559 to 659), respectively. All three bleb parameters were observed earlier in the trabeculectomy group. There was no statistically significant difference in the mean time for observing bleb avascularity (285 v 351 days, p = 0.2) and TCO (195 v 212 days) between the trabeculectomy and deep sclerectomy groups but PL (505 v 700 days, p<0.001) were observed significantly earlier in the trabeculectomy group (see fig 3).
Table 1 Patient demographics and baseline characteristics. All percentages are from the total number of patients in the study.
| No of patients (eyes) | 125 |
| Mean age (SD) (years) | 71 (12.3) |
| Male/female | 66/59 |
| Mean follow up in months (SD) (range) | 24 (5.7) (6–32) |
| “Trabeculectomy” procedures | 61 (48.8%) |
| Trabeculectomy | 26 (20.8%) |
| Phaco‐trabeculectomy | 24 (19.2%) |
| deep sclerectomy converted to trabeculectomy | 05 (4.0%) |
| deep sclerectomy intraoperative perforation | 06 (4.8%) |
| “Deep sclerectomy” procedures | 64 (51.2%) |
| Deep sclerectomy | 48 (38.4%) |
| Phaco deep sclerectomy | 16 (12.8%) |
| Previous laser | |
| Nd:YAG laser peripheral iridotomy | 2 (1.6%) |
| Argon laser trabeculoplasty | 3 (2.4%) |
| Previous surgeries* | |
| Trabeculectomy | 15 (12%) |
| Deep sclerectomy | 2 (1.6%) |
| Phaco‐trabeculectomy | 1 (0.8%) |
| Combined ECCE and trabeculectomy | 2 (1.6%) |
| Trabeculectomy + MMC, ECCE | 1 (0.8%) |
| ECCE | 4 (3.2%) |
| Phacoemulsification | 3 (2.4%) |
| Retinal detachment surgery | 1 (0.8%) |
| MMC application concentration and duration of application | |
| 0.1 mg/ml for 1 minute | 2 (1.6%) |
| 0.2 mg/ml for 1 minute | 7 (5.6%) |
| 0.2 mg/ml for 2 minutes | 98 (78.4%) |
| 0.2 mg/ml for 3 minutes | 15 (12.0%) |
| 0.4 mg/ml for 3 minutes | 3 (2.4%) |
ECCE, extracapsular cataract extraction.
*Some eyes had more than one surgery.
Figure 3 Point leak in an eye with a deep sclerectomy complicated by intraoperative perforation.
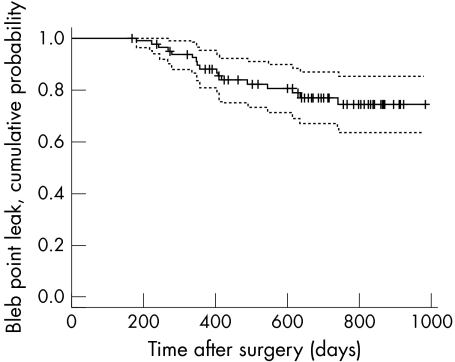
Kaplan‐Meier survival analyses (figures in parentheses are 95% confidence intervals) are depicted in figures 4, 5, and 6. They suggest that the probability of not developing bleb avascularity at sixth, 12th, and 24th month after surgery was 44% (35% to 50%), 39% (30% to 48%), and 37% (29% to 46%), respectively. Conversely, the probability of observing bleb avascularity at sixth, 12th, and 24th month after surgery was 56%, 71%, and 73% respectively. In eyes with avascular blebs, the probability of avoiding TCO and PL was 33% (23% to 43%) and 99% (96% to 100%) at 6 months, 19% (10% to 27%) and 88% (81% to 95%) at 12 months, and 5% (2% to 10%) and 74% (63% to 85%) at 24 months, respectively. Cox's regression models for risk factors (table 2) affecting the survival curves show that no factor had any significant effect on the development of avascular areas on bleb. Eyes with larger avascular blebs (>4 mm) were more likely to develop TCO (hazard ratio 3.77, p = 0.001) and delayed bleb leaks were more likely to be seen in eyes that had a trabeculectomy procedure (hazard ratio 0.06, p = 0.0006). Univariate, Kaplan‐Meier survival analyses confirmed that the probability of developing bleb leaks was significantly higher (log rank test p<0.001) in the trabeculectomy group (45.3% at 2 years) than in the deep sclerectomy group (7.3% at 2 years).
Figure 4 Kaplan‐Meier survival curves for probability of developing avascular areas on MMC augmented conjunctival filtration blebs. The broken lines represent 95% confidence intervals.
Figure 5 Kaplan‐Meier survival curves for the probability of observing transconjunctival oozing in eyes with avascular blebs. The broken lines represent 95% confidence intervals.
Table 2 Cox regression models for possible factors influencing the probability of developing avascular areas after MMC augmented glaucoma surgery and for TCO and bleb leaks to develop in eyes with avascular blebs.
| Risk factor | Model 1 bleb avascularity | Model 2 TCO in avascular blebs | Model 3 leaks in avascular blebs | |||
|---|---|---|---|---|---|---|
| Hazard ratios (95% CI) | p Value | Hazard ratios (95% CI)) | Hazard ratios (95% CI) | p Value | ||
| Age | 1.00 (0.98 to 1.02) | 0.77 | 1.00 (0.97 to 1.03) | 0.78 | 0.99 (0.93 to 1.07) | 0.94 |
| Sex | 1.04 (0.82 to 1.33) | 0.69 | 1.11 (0.84 to 1.47) | 0.45 | 1.00 (0.51 to 1.97) | 0.99 |
| Surgeon | 1.22 (0.69 to 2.16) | 0.49 | 0.74 (0.41 to 1.13) | 0.31 | 0.96 (0.19 to 4.83) | 0.97 |
| Type of procedure | 0.58 (0.34 to 0.99) | 0.05 | 0.61 (0.35 to 1.07) | 0.08 | 0.06 (0.01 to 0.31) | 0.0007 |
| Combined procedure | 0.60 (0.33 to 1.08) | 0.09 | 0.82 (0.45 to 1.51) | 0.53 | 1.19 to (0.31 to 3.93) | 0.80 |
| MMC application >2 minutes | 1.23 (0.54 to 2.81) | 0.62 | 0.59 (0.25 to 1.40) | 0.23 | 0.83 (0.19 to 3.66) | 0.81 |
| Previous intraocular surgery | 0.75 (0.35 to 1.60) | 0.45 | 0.64 (0.29 to 1.40) | 0.27 | 0.64 (0.14 to 2.89) | 0.57 |
| More than one previous ocular surgery | 0.66 (0.22 to 1.93) | 0.21 | 2.54 (0.73 to 8.80) | 0.14 | 2.02 (0.30 to 13.7) | 0.47 |
| Subconjunctival 5‐FU | 0.32 (0.11 to 0.91) | 0.03 | 0.96 (0.21 to 4.35) | 0.96 | No convergence | |
| Needle revision with 5‐FU within 3 months of surgery | 0.78 (0.24 to 2.57) | 0.69 | 0.76 (0.15 to 3.82) | 0.74 | No convergence | |
| Avascular area more than 4 mm | 3.77 (1.66 to 8.56) | 0.001 | No convergence | |||
Figure 6 Kaplan‐Meier survival curves for the probability of observing point leaks in eyes with avascular blebs. The broken lines represent 95% confidence intervals.
Details on bleb morphology and the frequency of observing TCO and leaks are given in table 3. The area of bleb avascularity was observed to increase in time in 21 eyes (16.8%) of the trabeculectomy group and 13 eyes (10.4%) of the deep sclerectomy group and decrease (with bleb failure and raised IOP in some cases) in 17 eyes (13.6%) of the trabeculectomy group and 24 (19.2%) of the deep sclerectomy group.
Table 3 Bleb characteristics after MMC enhanced glaucoma surgery.
| Bleb characteristics | Total | Trabeculectomy | Deep sclerectomy | p Value |
|---|---|---|---|---|
| Failed blebs | 5 (4.0%) | 1 (1.6%) | 4 (6.3%) | 0.37 |
| Encapsulated blebs | 5 (4.0%) | 5 (8.2%) | 0 (0%) | 0.20 |
| Bleb avascularity | 79 (62.6%) | 40 (65.6%) | 39 (61.0%) | 0.72 |
| Cystic avascular blebs | 60 (48.0%) | 33 (54.1%) | 27 (42.2%) | 0.25 |
| Avascularity >4 mm | 60 (48.0%) | 35 (57.4%) | 25 (39.1%) | 0.05 |
| Avascularity >8 mm | 30 (24.05) | 17 (27.9%) | 13 (20.3%) | 0.44 |
| Transconjunctival ooze | 70 (56%) | 36 (59.0%) | 34 (53.1%) | 0.62 |
| Bleb leaks | 17 (13.6%) | 14 (23.0%) | 2 (3.1%) | 0.004 |
| Seidel positive | 8 (6.4%) | 8 (13.1%) | 0 (0%) | |
| Point leaks | 9 (7.2%) | 7 (11.5%) | 2 (3.1%) |
Seidel positive leaks were observed in eight eyes (6.4%)—all in the trabeculectomy group. In one eye the leak resolved spontaneously. Three eyes are being observed as the patients are asymptomatic. One eye had blebitis that resolved on topical antibiotics and subsequently the avascular bleb was excised. A scleral patch allograft and conjunctival autograft was done in one eye with an extremely thin scleral flap and persistent leak. Leaks resolved after autologous blood injection into the bleb and after phacoemulsification in one eye each. Point leaks were observed in nine eyes (7.2%)—seven from the trabeculectomy and two from the deep sclerectomy group. These leaks are being managed conservatively and have resolved spontaneously in four eyes and after a phacoemulsification in one eye (see fig 3).
Bleb infections were seen in two eyes (1.6%), one from each group developed blebitis in the follow up period. No endophthalmitis has been observed to date. In one eye the leak preceded the blebitis. In the second eye (deep sclerectomy), a point leak was observed at the same time with blebitis. The leak resolved with the blebitis on topical antibiotic therapy. The patient has severe long standing eczema and blepharitis and is now on low dose oral tetracycline and lid hygiene.
In the first 3 months after surgery, 11 eyes (18.0%) of the trabeculectomy group received an average of 1.5 injections and five eyes of the deep sclerectomy group received a mean of one injection of subconjunctival 5‐FU. Needle revision with adjunctive 5‐FU in the same period was done in 11 eyes (18%) of the trabeculectomy group and none of the deep sclerectomy group. Procedures done after the initial surgery are shown in table 4. Scleral patch graft for hypotony with maculopathy was done in four eyes (3.2%) of the trabeculectomy group. No hypotony was seen in the deep sclerectomy group. The average of all measured IOPs (standard deviation) from 4 months after surgery was 12.62 (5.85) mm Hg for the trabeculectomy group and 13.31 (5.26) for the deep sclerectomy group and this difference was not statistically different at any time interval (ANOVA p>0.05). A total of 42 eyes (65.6%) in the deep sclerectomy group underwent Nd:YAG laser goniopuncture to lower IOP to the target range. Needle revision with concurrent injection of antimetabolites for delayed failure of blebs or increasing IOP (after 4 months) was done in 11 eyes (18%) of the trabeculectomy group and seven eyes (10.9%) of the deep sclerectomy group.
Table 4 Subsequent procedures after MMC augmented glaucoma surgery. Some eyes had more than one procedure.
| Subsequent procedures | Total | Trabeculectomy | Deep sclerectomy |
|---|---|---|---|
| Scleral patch allograft | 4(3.2%) | 4 (6.6%) | 0 |
| Bleb repair with excision of avascular area | 2 (1.6%) | 2(1.6%) | 0 |
| Subconjunctival autologous blood | 2 (1.6%) | 2(1.6%) | 0 |
| Delimiting conjunctival sutures | 1 (0.8%) | 0 | 1 (1.6%) |
| Phacoemulsification | 5 (4.0%) | 2 (3.7%) | 3 (4.7%) |
| Needle revision | 18 (14.4%) | 11 (17.2%) | 7 (10.9%) |
Discussion
The association between delayed bleb leaks and thin walled, avascular blebs has been reported previously and these leaks were more frequent after full thickness procedures.29 The use of MMC to enhance trabeculectomy has probably led to an increase in the frequency of thin avascular blebs and the consequences like delayed bleb leaks, hypotony, and bleb infections.30,31,32,33,34 The long terms effects of MMC on blebs after deep sclerectomy have not been reported.
Our study establishes that there is a high incidence of bleb avascularity, TCO, and delayed leaks after low dose MMC enhanced glaucoma surgery in a population of predominantly white patients. Bleb avascularity precedes TCO on average, by 3 months. Most blebs will show avascularity and TCO by the first year after surgery. However, delayed bleb leaks are usually seen after the first year and their incidence continues to increase with time. This may, in part, explain the development of delayed hypotony and endophthalmitis after MMC enhanced glaucoma surgery. Bindlish et al reported new cases of hypotony 4 years and 5 years after surgery.12 Why does this occur? Histopathological studies suggest that MMC produces an avascular and hypocellular scleral flap through a sustained cytotoxic effect on vascular endothelial cells, fibroblasts, and limbal pleuripotent stem cells. These effects also lead to bleb avascularity and frequent oozing and eventually breakdown of the conjunctival epithelial barrier months to years after uncomplicated surgery.23,25 Toxicity to ciliary body and hyposecretion are another explanation for late hypotony.23,35,36
We included patients who underwent deep sclerectomy procedures for several reasons; we have previously reported that most of our patients who had successful MMC augmented deep sclerectomy had visible conjunctival filtration blebs. Moreover, most of these blebs had avascular and cystic areas.37 Ultrasound biomicroscopy studies show a passage from the subscleral lake to the subconjunctival space.38,39 Most of the NPGS eyes also underwent Nd:YAG laser goniopuncture (42 eyes, 65.6%) effectively converting them into “micro penetrating” procedures. We did not analyse the effect of laser goniopuncture on bleb parameters. This procedure was often done to further lower the IOP after the first postoperative month. It would be impossible to isolate the effect of laser goniopuncture from that of intraoperative MMC and this is an important limitation of the study. A further study to see the effect of goniopuncture done at least 6 months after the initial surgery on filtration blebs is required.
We have reported a much higher frequency for bleb avascularity, TCO, and leaks than previous studies despite using a relatively lower MMC dose and application but similar technique. This may be because of the study design—prospective compared to cross sectional for previous studies. There is a delay between observing bleb avascularity and TCO of approximately 100 days. Hu et al16 had included patients with follow up ranging between 3 months to 4 years. A significant proportion of eyes with avascular blebs which would eventually exhibit TCO would have been missed. This is supported by their finding that blebs in the first postoperative year were significantly thicker and less likely to leak than blebs older than 2–3 years. Their technique for examination was slightly different, using moistened fluorescein strips and observation for oozing for 15 seconds. We used dry fluorescein strips and observed for a minimum of 30 seconds. It is possible our technique is more sensitive in picking up TCO. Dry fluorescein strips may actually de‐epithelialise the conjunctiva resulting in a higher incidence of TCO. On the other hand, they used a higher concentration and a longer application time for MMC (0.4 mg/ml for 3 minutes) and excluded cases undergoing repeat surgery. Despite this our incidence of bleb avascularity and leaks was similar. Data from both the studies and ours favour lowering the concentration and duration of MMC application during surgery, even in eyes with previous conjunctival surgery.
The treatment of TCO and point leaks in asymptomatic patients remains unclear. The association between avascular, thin walled blebs and bleb infections and endophthalmitis has been alluded to earlier in the discussion. Autologous serum injections have been shown to be effective in halting TCO but not point leaks.40 We currently do not intervene surgically unless there is hypotony, an episode of bleb infection, or the patient has bleb related symptoms like discomfort or blurred vision. . During the course of this study five leaks (29.4%), one frank bleb leak and four (of nine, 44%) point leaks, have resolved spontaneously. Three (of eight, 37.5%) eyes with Seidel leaks are asymptomatic and are being managed expectantly. No patient with a point leak is symptomatic and three (33%) have IOPs of more than 10 mm Hg.
It is evident from this study that MMC application on the area of scleral flap dissection leads to a high incidence of bleb avascularity, oozing, and delayed point leaks, regardless of the type of glaucoma surgery. A more posterior and wider application of MMC may lead to a lower frequency of bleb avascularity and leaks and perhaps should be adopted routinely.41,42
Abbreviations
5‐FU - 5‐fluorouracil
IOP - intraocular pressure
MMC - mitomycin C
PL - point leak
TCO - transconjunctival oozing
References
- 1.The Fluorouracil Filtering Surgery Study Group Five‐year follow‐up of the Fluorouracil Filtering Surgery Study. Am J Ophthalmol 1996121349–366. [DOI] [PubMed] [Google Scholar]
- 2.Beckers H J, Kinders K C, Webers C A. Five‐year results of trabeculectomy with mitomycin C. Graefes Arch Clin Exp Ophthalmol 2003241106–110. [DOI] [PubMed] [Google Scholar]
- 3.WuDunn D, Cantor L B, Palanca‐Capistrano A M.et al A prospective randomized trial comparing intraoperative 5‐fluorouracil vs mitomycin C in primary trabeculectomy. Am J Ophthalmol 2002134521–528. [DOI] [PubMed] [Google Scholar]
- 4.Hagiwara Y, Yamamoto T, Kitazawa Y. The effect of mitomycin C trabeculectomy on the progression of visual field defect in normal‐tension glaucoma. Graefes Arch Clin Exp Ophthalmol 2000238232–236. [DOI] [PubMed] [Google Scholar]
- 5.Kim Y Y, Sexton R M, Shin D H.et al Outcomes of primary phakic trabeculectomies without versus with 0.5‐ to 1‐minute versus 3‐ to 5‐minute mitomycin C. Am J Ophthalmol 1998126755–762. [DOI] [PubMed] [Google Scholar]
- 6.Mietz H, Krieglstein G K. Three‐year follow‐up of trabeculectomies performed with different concentrations of mitomycin‐C. Ophthalmic Surg Lasers 199829628–634. [PubMed] [Google Scholar]
- 7.Costa V P, Comegno P E, Vasconcelos J P.et al Low‐dose mitomycin C trabeculectomy in patients with advanced glaucoma. J Glaucoma 19965193–199. [PubMed] [Google Scholar]
- 8.Chen C W, Huang H T, Bair J S.et al Trabeculectomy with simultaneous topical application of mitomycin‐C in refractory glaucoma. J Ocul Pharmacol 19906175–182. [DOI] [PubMed] [Google Scholar]
- 9.Fluorouracil Filtering Surgery Study Three‐year follow‐up of the Fluorouracil Filtering Surgery Study. Am J Ophthalmol 199311582–92. [DOI] [PubMed] [Google Scholar]
- 10.Akova Y A, Bulut S, Dabil H.et al Late bleb‐related endophthalmitis after trabeculectomy with mitomycin C. Ophthalmic Surg Lasers 199930146–151. [PubMed] [Google Scholar]
- 11.Belyea D A, Dan J A, Stamper R L.et al Late onset of sequential multifocal bleb leaks after glaucoma filtration surgery with 5‐fluorouracil and mitomycin C. Am J Ophthalmol 199712440–45. [DOI] [PubMed] [Google Scholar]
- 12.Bindlish R, Condon G P, Schlosser J D.et al Efficacy and safety of mitomycin‐C in primary trabeculectomy: five‐year follow‐up. Ophthalmology 20021091336–1341. [DOI] [PubMed] [Google Scholar]
- 13.Costa V P, Wilson R P, Moster M R.et al Hypotony maculopathy following the use of topical mitomycin C in glaucoma filtration surgery. Ophthalmic Surg 199324389–394. [PubMed] [Google Scholar]
- 14.Dreyer E B, Chaturvedi N, Zurakowski D. Effect of mitomycin C and fluorouracil‐supplemented trabeculectomies on the anterior segment. Arch Ophthalmol 1995113578–580. [DOI] [PubMed] [Google Scholar]
- 15.Greenfield D S, Liebmann J M, Jee J.et al Late‐onset bleb leaks after glaucoma filtering surgery. Arch Ophthalmol 1998116443–447. [DOI] [PubMed] [Google Scholar]
- 16.Hu C Y, Matsuo H, Tomita G.et al Clinical characteristics and leakage of functioning blebs after trabeculectomy with mitomycin‐C in primary glaucoma patients. Ophthalmology 2003110345–352. [DOI] [PubMed] [Google Scholar]
- 17.Membrey W L, Poinoosawmy D P, Bunce C.et al Glaucoma surgery with or without adjunctive antiproliferatives in normal tension glaucoma: 1 intraocular pressure control and complications. Br J Ophthalmol 200084586–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mochizuki K, Jikihara S, Ando Y.et al Incidence of delayed onset infection after trabeculectomy with adjunctive mitomycin C or 5‐fluorouracil treatment. Br J Ophthalmol 199781877–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Muckley E D, Lehrer R A. Late‐onset blebitis/endophthalmitis: incidence and outcomes with mitomycin C. Optom Vis Sci 200481499–504. [DOI] [PubMed] [Google Scholar]
- 20.Susanna R, Jr, Takahashi W, Nicolela M. Late bleb leakage after trabeculectomy with 5‐fluorouracil or mitomycin C. Can J Ophthalmol 199631296–300. [PubMed] [Google Scholar]
- 21.Ticho U, Ophir A. Late complications after glaucoma filtering surgery with adjunctive 5‐fluorouracil. Am J Ophthalmol 1993115506–510. [DOI] [PubMed] [Google Scholar]
- 22.Mandal A K, Vemuganti G K, Ladda N.et al Partial excision with a conjunctival advancement flap after a relaxing incision for a dissecting glaucoma filtering bleb. Ophthalmic Surg Lasers 200233497–500. [PubMed] [Google Scholar]
- 23.Nuyts R M, Felten P C, Pels E.et al Histopathologic effects of mitomycin C after trabeculectomy in human glaucomatous eyes with persistent hypotony. Am J Ophthalmol 1994118225–237. [DOI] [PubMed] [Google Scholar]
- 24.Shields M B, Scroggs M W, Sloop C M.et al Clinical and histopathologic observations concerning hypotony after trabeculectomy with adjunctive mitomycin C. Am J Ophthalmol 1993116673–683. [DOI] [PubMed] [Google Scholar]
- 25.Mietz H, Arnold G, Kirchhof B.et al Histopathology of episcleral fibrosis after trabeculectomy with and without mitomycin C. Graefes Arch Clin Exp Ophthalmol 1996234364–368. [DOI] [PubMed] [Google Scholar]
- 26.Matsuo H, Tomidokoro A, Suzuki Y.et al Late‐onset transconjunctival oozing and point leak of aqueous humor from filtering bleb after trabeculectomy. Am J Ophthalmol 2002133456–462. [DOI] [PubMed] [Google Scholar]
- 27.Anand N, Atherley C. Deep sclerectomy augmented with mitomycin C. Eye 200519442–450. [DOI] [PubMed] [Google Scholar]
- 28.Funnell C L, Clowes M, Anand N. Combined cataract and glaucoma surgery with mitomycin C: phacoemulsification‐trabeculectomy compared to phacoemulsification‐deep sclerectomy. Br J Ophthalmol 200589694–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lamping K A, Bellows A R, Hutchinson B T.et al Long‐term evaluation of initial filtration surgery. Ophthalmology 19869391–101. [DOI] [PubMed] [Google Scholar]
- 30.Poulsen E J, Allingham R R. Characteristics and risk factors of infections after glaucoma filtering surgery. J Glaucoma 20009438–443. [DOI] [PubMed] [Google Scholar]
- 31.Mochizuki K, Jikihara S, Ando Y.et al Incidence of delayed onset infection after trabeculectomy with adjunctive mitomycin C or 5‐fluorouracil treatment. Br J Ophthalmol 199781877–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.DeBry P W, Perkins T W, Heatley G.et al Incidence of late‐onset bleb‐related complications following trabeculectomy with mitomycin. Arch Ophthalmol 2002120297–300. [DOI] [PubMed] [Google Scholar]
- 33.Bindlish R, Condon G P, Schlosser J D.et al Efficacy and safety of mitomycin‐C in primary trabeculectomy: five‐year follow‐up. Ophthalmology 20021091336–1341. [DOI] [PubMed] [Google Scholar]
- 34.Soltau J B, Rothman R F, Budenz D L.et al Risk factors for glaucoma filtering bleb infections. Arch Ophthalmol 2000118338–342. [DOI] [PubMed] [Google Scholar]
- 35.Mietz H. The toxicology of mitomycin C on the ciliary body. Curr Opin Ophthalmol 1996772–79. [DOI] [PubMed] [Google Scholar]
- 36.Schraermeyer U, Diestelhorst M, Bieker A.et al Morphologic proof of the toxicity of mitomycin C on the ciliary body in relation to different application methods. Graefes Arch Clin Exp Ophthalmol 1999237593–600. [DOI] [PubMed] [Google Scholar]
- 37.Anand N, Atherley C. Deep sclerectomy augmented with mitomycin C. Eye 200519442–450. [DOI] [PubMed] [Google Scholar]
- 38.Marchini G, Marraffa M, Brunelli C.et al Ultrasound biomicroscopy and intraocular‐pressure‐lowering mechanisms of deep sclerectomy with reticulated hyaluronic acid implant. J Cataract Refract Surg 200127507–517. [DOI] [PubMed] [Google Scholar]
- 39.Roters S, Luke C, Jonescu‐Cuypers C P.et al Ultrasound biomicroscopy and its value in predicting the long term outcome of viscocanalostomy. Br J Ophthalmol 200286997–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Matsuo H, Tomidokoro A, Tomita G.et al Topical application of autologous serum for the treatment of late‐onset aqueous oozing or point‐leak through filtering bleb. Eye 20051923–28. [DOI] [PubMed] [Google Scholar]
- 41.Wells A P, Cordeiro M F, Bunce C.et al Cystic bleb formation and related complications in limbus‐ versus fornix‐based conjunctival flaps in pediatric and young adult trabeculectomy with mitomycin C. Ophthalmology 20031102192–2197. [DOI] [PubMed] [Google Scholar]
- 42.Cordeiro M F, Constable P H, Alexander R A.et al Effect of varying the mitomycin‐C treatment area in glaucoma filtration surgery in the rabbit. Invest Ophthalmol Vis Sci 1997381639–1646. [PubMed] [Google Scholar]