Abstract
Aims
To assess the long term functional and structural outcomes of premature babies who received diode laser photocoagulation for threshold retinopathy of prematurity (ROP).
Methods
25 patients (43 eyes) treated with laser were recalled for assessment at a mean follow up of 11 years. A further seven patients (14 eyes) with subthreshold ROP, which had regressed spontaneously without laser treatment, were also examined. All children underwent distance acuity, near acuity, contrast sensitivity (CS), and colour vision assessments followed by a dilated fundal examination and cycloplegic autorefraction.
Results
The laser treated eyes had a mean distance visual acuity of 0.37 logMAR, a mean near visual acuity of 0.39 logMAR, a mean contrast sensitivity of 1.49 log CS units, and a mean spherical equivalent of −2.10D. An unfavourable distance visual acuity outcome occurred in five eyes (13.5%). An unfavourable near visual acuity outcome was also noted in the five eyes (13.5%) with poor distance visual outcome. 7% had an unfavourable structural outcome. On comparison with the control group, there was no significant difference in near acuity, CS, refraction, or colour vision between the two groups. However, there was a statistically significant difference in terms of distance visual acuity (p = 0.03).
Conclusions
Laser treated eyes with favourable structural outcome have a good visual outcome. The results show a long term benefit from diode laser photocoagulation in preserving distance and near vision in eyes with threshold ROP.
Keywords: diode laser photocoagulation, retinopathy of prematurity, visual outcome, infants
Retinopathy of prematurity (ROP) is a potentially blinding condition of premature babies. Ten year follow up data from the CRYO‐ROP study have demonstrated the long term beneficial effect of cryotherapy on eyes with threshold ROP.1,2 Laser photocoagulation has replaced cryotherapy as the established treatment for ROP in most centres. Although no randomised trial has been conducted on the scale of the CRYO‐ROP study, meta‐analysis of smaller studies has shown laser treatment to be at least as effective as cryotherapy in the treatment of threshold ROP.3,4,5,6
However, there is limited information available on the long term functional outcome after laser therapy for ROP. The clinical objective of this study was to evaluate the long term outcomes of a cohort of premature infants who were treated with diode laser photocoagulation for threshold ROP. Mean follow up was 11 years.
Methods
In all, 41 premature babies who received laser for ROP, 9 years or more previously, were identified from a register of treated children at the neonatal unit of the National Maternity Hospital, Dublin. In all cases, laser treatment was placed, under sedation, anterior to the fibrovascular ridge in accordance with the Royal College of Ophthalmologists' guidelines for ROP treatment.7 Four of these patients had died before the age of 9 months (deaths not related to laser treatment). Of the remaining 37 children, 25 were contactable. All were recruited and reviewed with informed parental consent.
A total of 18 patients, also with 9 years or more of follow up, were identified as potential controls (at least stage 2, zone II−III ROP with spontaneous regression) from a logbook of babies screened for ROP in the neonatal unit (screening criteria of <31 weeks gestational age or ⩽1500 g birth weight). These children were selected for inclusion in the study with view to having a control population which closely matched the study population in terms of prematurity and severity of ROP.8,9,10 Six of these children were not contactable and there were five parental refusals. The remaining seven children participated in the study.
The patients were recalled to the eye clinic at the Children's Hospital for assessment by a single observer (EML). For all measurements of visual function, testing was performed monocularly with the children wearing their normal spectacle correction, where applicable.
Visual acuity
Best corrected distance visual acuity (BCDVA) was recorded using a back illuminated Distance ETDRS chart (Lighthouse Inc, New York, NY, USA) at a test distance of 4 metres. Visual acuity was estimated as the logMAR value of the last line on which the child could correctly identify three of the five available letters. In order to include all data in the statistical analysis, any eye with vision less than 1/60 was assigned a logMAR score of 2.0.
Best corrected near visual acuity (BCNVA) was recorded using the Near ETDRS chart (Lighthouse Inc) at the standard test distance of 40 cm. The procedure and scoring used were the same as for the distance vision testing.
Contrast sensitivity and colour vision
Contrast sensitivity (CS) was assessed using two Pelli‐Robson charts (one per eye) at a test distance of 1 metre and estimated as the log contrast value of the last triplet on which the child identified at least two of the three letters correctly and also by the total number of letters identified correctly.11,12
Colour vision was tested using the HRR pseudoisochromatic plates (Richmond Products, Inc, 3rd ed) at a test distance of 75 cm. There are four demonstration plates and 20 test plates, of which six are screening plates and 14 are diagnostic plates. For each eye, any incorrect test plates were noted as well as the corresponding colour defect.
Structural assessment and refraction
After visual function testing, a full eye examination was conducted including a cover/uncover test, alternate cover test, extraocular movement assessment, and dilated fundal check (cyclopentolate 1%). Cycloplegic refraction was performed using a desktop autorefractometer (Model AR‐630A, Nidek Co Ltd, Japan).
Data analysis
In order to allow comparison of our results with the 10 year findings of the CRYO‐ROP study, we adopted the same definitions of unfavourable visual and structural outcomes as used in that study.1,2 An unfavourable distance or near visual outcome was defined as a Snellen visual acuity of 6/60 (logMAR 1.0) or worse. An unfavourable contrast sensitivity outcome was defined as a score of 26 letters or less on the Pelli‐Robson chart. An unfavourable structural outcome was defined as a partial or total retinal detachment involving the fovea (stage 4b–5), a retinal fold involving the fovea, retrolental membrane, corneal opacity, or enucleation.
Statistical analysis
Analysis was performed using Matlab 6.5 (Statistics Toolbox 4.0). In order to address any problems with the normality of the data, continuous outcomes were compared using both the parametric Student's t test and the non‐parametric Wilcoxon rank sum test. However, both tests provided consistent results throughout. Consequently, only Student's t test p values are reported in the paper. Fisher's exact test was used to compare categorical outcomes. A p value of less than 0.05 was considered significant.
Results
Of the 25 children in the laser group, 18 had bilateral treatment and seven had unilateral treatment for threshold ROP, yielding a total of 43 treated eyes. The control group comprised seven children (14 eyes). The demographic characteristics of both groups did not differ significantly (table 1).
Table 1 Baseline characteristics of the study population.
| Variable | Laser group (25 patients/43 eyes) | Control group (7 patients/14 eyes) | Laser v control (p value) |
|---|---|---|---|
| GA (weeks) (mean (SD)) | 26.5 (1.7) | 27.4 (1.5) | 0.21 |
| BW (g) (mean (SD)) | 888.8 (184.3) | 941.9 (256.6) | 0.54 |
| Follow up (years) (mean (SD)) | 11.0 (1.0) | 11.5 (1.3) | 0.29 |
| Sex, n (%) | |||
| Male | 16 (64) | 5 (71) | 0.55 |
| Female | 9 (36) | 2 (29) | 0.54 |
| Neurological problems, n (%) | |||
| IVH | 9 (36) | 1 (14) | 0.27 |
| ONH | 5 (20) | 0 (0) | 0.26 |
| Sixth nerve palsy | 1 (4) | 0 (0) | 0.78 |
GA, gestational age; BW, birth weight; SD, standard deviation; IVH, intraventricular haemorrhage; ONH, optic nerve hypoplasia.
In the laser group, 24 patients (96%) had at least five contiguous or eight cumulative clock hours of stage 3 disease in zone II with plus at the time of treatment. Only one patient (4%) had zone I rush disease in both eyes (that is, ROP in zone I with plus disease which progressed rapidly within days). Diode laser treatment was performed at a median postmenstrual age of 34.6 weeks (range 33.3–40.1 weeks). A mean of 2.1 laser treatment sessions were required per eye to achieve regression of ROP.
Structural outcome
Of the 43 laser treated eyes, two eyes (4.7%) progressed to bilateral total retinal detachments despite diode laser treatment. Both eyes belonged to the one patient who had zone I rush disease. One eye of another patient was noted to have a retinal fold involving the fovea. None of the remaining treated eyes had any evidence of macular ectopia or disc dragging. Overall, 40 eyes (93%) had a favourable structural outcome. None of the 14 control eyes with spontaneous regression of ROP showed any evidence of long term sequelae.
Eight of the 25 laser patients (32%) had strabismus; four were convergent and four were divergent. Five patients (20%) were treated for amblyopia; four of whom had strabismus and one of whom had myopic anisometropia. Three patients (12%) were noted to have nystagmus. Of the seven control patients, one (14.3%) had a convergent squint. None had amblyopia or nystagmus.
Visual outcome: laser group
Within the laser treated group, three patients with a history of severe intraventricular haemorrhage (IVH) had severe cognitive impairment as a result of cerebral palsy and were unable to cooperate with assessments of visual function. All three had bilateral optic nerve hypoplasia but otherwise normal retinal structure. Therefore, data on visual outcome and refraction were available on 22 patients (37 eyes). This information is summarised in table 2.
Table 2 Functional outcome of the laser group.
| Patient | Sex | BCDVA (logMAR) | BCNVA (logMAR) | Contrast sensitivity (log CS units) | Spherical equivalent (D) | ||||
|---|---|---|---|---|---|---|---|---|---|
| Right | Left | Right | Left | Right | Left | Right | Left | ||
| 1*‡ | M | 0.3 | 0.3 | 0.1 | 0.0 | 1.65 | 1.65 | −15.00 | −17.00 |
| 2 | M | – | −0.2 | – | 0.1 | – | 1.80 | – | +1.25 |
| 3 | F | 0.0 | 0.1 | 0.0 | 0.1 | 1.65 | 1.65 | −1.38 | −1.25 |
| 4† | F | 0.9 | – | 0.4 | – | 1.20 | – | −5.63 | – |
| 5‡§¶ | M | 0.4 | 1.8 | 0.7 | 1.6 | 1.95 | 0.00 | +1.00 | −4.25 |
| 6§¶ | M | 0.2 | 1.0 | 0.1 | 1.3 | 1.80 | 0.90 | +0.38 | −5.75 |
| 7§ | M | −0.1 | 0.4 | 0.1 | 0.5 | 1.80 | 1.65 | +5.13 | +2.13 |
| 8 | F | 0.1 | 0.1 | 0.0 | 0.3 | 1.65 | 1.65 | +0.75 | +1.00 |
| 9*‡ | M | 0.1 | – | 0.0 | – | 1.50 | – | +2.75 | – |
| 10 | F | – | 0.0 | – | −0.1 | – | 1.65 | – | −2.88 |
| 11 | F | 0.2 | 0.4 | 0.7 | 0.8 | 1.65 | 1.65 | +1.25 | +0.75 |
| 12 | M | 0.0 | 0.0 | −0.1 | −0.1 | 1.95 | 1.80 | +1.00 | +1.00 |
| 13 | M | 0.0 | −0.1 | 0.1 | 0.0 | 1.80 | 1.80 | +0.63 | +0.63 |
| 14 | M | 0.1 | – | 0.4 | – | 1.80 | – | +1.50 | – |
| 15†¶ | M | 0.8 | 0.3 | 0.9 | 0.3 | 0.75 | 1.95 | −8.25 | −5.25 |
| 16 | M | – | −0.1 | – | 0.0 | – | 1.65 | – | +2.50 |
| 17‡ | F | 0.1 | 0.2 | 0.1 | 0.1 | 1.80 | 1.80 | −5.50 | −7.38 |
| 18** | F | 0.0 | 1.8 | 0.3 | 2.0 | 1.95 | 0.00 | −6.25 | NA |
| 19 | M | 0.2 | 0.2 | 0.1 | 0.1 | 1.65 | 1.65 | −6.75 | −5.50 |
| 20‡ | F | 0.1 | 0.2 | −0.1 | −0.1 | 1.80 | 1.80 | −0.63 | +4.75 |
| 21 | M | – | 0.0 | – | −0.1 | – | 1.65 | – | −1.00 |
| 22ࠠ | M | 2.0 | 2.0 | 2.0 | 2.0 | 0.00 | 0.00 | NA | NA |
GA, gestational age in weeks; BW, birth weight in grams; BCDVA, best corrected distance visual acuity; BCNVA, best corrected near visual acuity; NA, not available as refraction not possible.
– indicates eyes that did not receive laser treatment as patients had unilateral threshold ROP.
*Optic nerve hypoplasia.
‡Intraventricular haemorrhage.
†Right eye amblyopic.
§Left eye amblyopic.
¶Manifest nystagmus of both eyes.
**Patient 18 had a retinal fold involving the left fovea.
††Patient 22 had bilateral total retinal detachments.
The laser treated eyes had a mean BCDVA of 0.37 logMAR with 27 eyes (73%) achieving 6/12 or better vision. An unfavourable distance visual acuity outcome occurred in five eyes (13.5%). Three of these eyes also had an unfavourable structural outcome as outlined above. The other two eyes (left eyes of two patients) were divergent and amblyopic. A further five eyes (13.5%) also had moderate visual loss (>0.3 to <1.0 logMAR); three were amblyopic, one had manifest nystagmus, and one was unexplained.
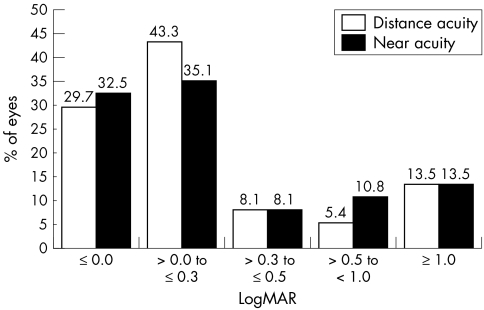
In terms of near visual acuity, 25 eyes (67.6%) achieved a Snellen equivalent of 6/12 or better vision with an overall mean BCNVA of 0.39 logMAR. An unfavourable near vision outcome was also noted in the five eyes (13.5%) with poor distance visual outcome (fig 1). Seven eyes (18.9%) had moderate visual loss. These included the five eyes with moderate distance visual loss and two others with no obvious cause for the visual loss.
Figure 1 Distance and near acuities in laser group.
The mean contrast sensitivity was 1.49 log CS units (32.4 letters correct); 31 eyes (83.8%) read 27 or more letters correctly on the Pelli‐Robson chart and were therefore considered to have had a favourable outcome. For the overall data, a strong correlation existed between BCDVA and contrast sensitivity (r = −0.95, p<0.0001). This correlation was not evident when only those eyes with BCDVA of 0.5 logMAR or better were considered; (r = −0.09, p = 0.65).
Fifty per cent of the laser treated eyes were myopic with an overall mean spherical equivalent of −2.10D.
Visual outcome: comparison with the control group
The control group data on visual outcome and refraction are given in table 3.
Table 3 Functional outcome of the control group.
| Patient | Sex | BCDVA (logMAR) | BCNVA (logMAR) | Contrast sensitivity (log CS units) | Spherical equivalent (D) | ||||
|---|---|---|---|---|---|---|---|---|---|
| Right | Left | Right | Left | Right | Left | Right | Left | ||
| 1 | M | −0.1 | −0.1 | 0.1 | 0.1 | 1.95 | 1.95 | +0.88 | +0.63 |
| 2 | F | 0.0 | 0.0 | 0.2 | 0.3 | 1.65 | 1.80 | +7.38 | +8.13 |
| 3 | M | 0.0 | 0.0 | −0.1 | −0.1 | 1.65 | 1.80 | +0.25 | +0.13 |
| 4 | M | −0.2 | −0.2 | −0.1 | −0.1 | 1.80 | 1.80 | +0.25 | +0.38 |
| 5* | M | 0.0 | 0.0 | −0.1 | −0.1 | 1.80 | 1.65 | +1.50 | +1.13 |
| 6 | M | −0.1 | 0.0 | 0.2 | 0.1 | 1.80 | 1.95 | −0.63 | −0.75 |
| 7 | F | −0.2 | −0.2 | −0.1 | −0.1 | 1.95 | 1.95 | −0.25 | +0.00 |
GA, gestational age in weeks; BW, birth weight in grams; BCDVA, best corrected distance visual acuity; BCNVA, best corrected near visual acuity.
*Intraventricular haemorrhage.
For statistical purposes, only one eye per patient in both the laser and control groups was included in the comparative analysis to assess for the effect of the diode laser on visual outcome. The right eye was chosen in all cases where data were available for both eyes. One patient in the control group had grade 1 IVH (subependymal haemorrhage). Higher grades of IVH have been associated with reduced visual function.13,14 Therefore, laser treated patients with grade 2 or more IVH (n = 4) were excluded from the comparative analysis; two of these patients also had ONH and one patient had bilateral retinal detachments (table 2). As all of the control eyes had normal fundal structure with no amblyopia or nystagmus, a further three eyes were also excluded, two with ambylopia and one with nystagmus. The comparative data on visual outcome are given in table 4.
Table 4 Comparison of functional outcomes.
| Variable | Modified laser group (15 eyes) | Control group (7 eyes) | Laser v control | ||||
|---|---|---|---|---|---|---|---|
| Mean | SD | 95% CI | Mean | SD | 95% CI | p value | |
| BCDVA (logMAR) | 0.03 | 0.11 | 0.06 | −0.09 | 0.09 | 0.08 | 0.03 |
| BCNVA (logMAR) | 0.13 | 0.23 | 0.13 | 0.01 | 0.15 | 0.13 | 0.26 |
| Contrast sensitivity (logMAR) | 1.75 | 0.11 | 0.06 | 1.80 | 0.12 | 0.11 | 0.35 |
| Spherical equivalent (dioptres) | −0.69 | 3.37 | 1.86 | +1.34 | 2.75 | 2.46 | 0.18 |
BCDVA, best corrected distance visual acuity; BCNVA, best corrected near visual acuity.
SD, standard deviation; CI, confidence interval.
Only BCDVA differed significantly between the two groups (p = 0.03).
Colour vision
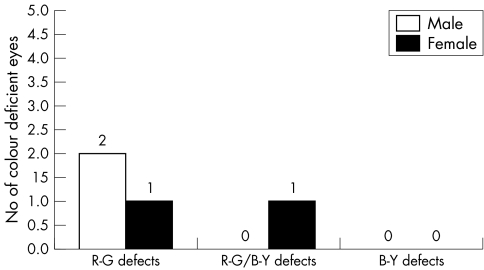
Of the 25 children in the laser group, four were unable to appreciate the HRR demonstration plates (three had severe cognitive impairment and one had bilateral total retinal detachments). Only one eye of each the 21 remaining patients was included in the colour vision analysis. All of these 21 eyes identified the diagnostic plates correctly. However, four eyes (19%) failed to correctly identify some of the symbols on the six screening plates (which are the most difficult with the lowest saturations) and thus were considered to have mild colour defects.15 None of the four children had neurological defects. The class of defect and sex distribution of the colour deficient children are given in figure 2. All seven of the children in the control group had normal colour vision. The observed increase in colour deficient eyes in the laser group was not statistically significant (p = 0.29).
Figure 2 Colour defects in 21 laser treated eyes.
Discussion
An ideal control group for this study would consist of patients with threshold ROP randomised to observation without laser treatment. However, in light of the unequivocal benefit of treatment demonstrated in the CRYO‐ROP study, this is obviously unethical.16 In view of this, we selected controls with significant ROP which failed to reach threshold level and which regressed spontaneously.
Our comparative visual outcome results showed that the control group had statistically significant better distance visual acuity than the laser treated eyes. It is not clear whether this difference is attributable to a direct effect of the diode laser itself or to the fact that the control group had less severe ROP from the outset. It is, however, encouraging to note that our laser group still performed well in terms of functional visual acuity. Our overall mean BCDVA of 0.37 logMAR (Snellen equivalent of 20/47) compares favourably with the findings of other investigators as presented in table 5.17,18,19
Table 5 Summary of studies on long term outcomes of laser therapy for ROP.
| Study | No of eyes | Type of laser | Mean follow up | Mean BCDVA | BCDVA ⩾6/12 | Eyes with total RD |
|---|---|---|---|---|---|---|
| Ospina et al17 | 42 | Argon | 6.2 years | 20/98 | 71.4% | 2.4% |
| Shalev et al18 | 10 | Diode | 7.0 years | 20/33 | 70.0% | 0.0% |
| Ng et al19 | 23 | Argon and diode | 9.9 years | 20/66 | 61.9% | 8.7% |
| Our study | 37 | Diode | 11.0 years | 20/47 | 73.0% | *4.7% |
*43 eyes in structural outcome analysis.
The mean BCDVA in these studies ranges from approximately 0.2 to 0.7 logMAR which equates to a five line difference in reported distance visual outcome. This is partly attributable to the fact that, as the children were younger at the time of assessment in some of the other studies, a variety of methods were employed for distance visual acuity measurement including Teller acuity cards, HOTV letter recognition charts, linear tumbling “E” cards, and Snellen charts. As our study cohort had longer follow up, all of the patients were old enough to be assessed with the ETDRS chart. Ng et al also used the ETDRS chart for the majority of their patients but, compared to our findings, their reduced mean BCDVA reflects a higher rate of poor structural outcome in their study.19
While 73% of laser treated eyes achieved 6/12 or better distance visual acuity, 13.5% had severe visual loss (<6/60) and a further 13.5% had moderate visual loss (<6/12 but >6/60). Only three of the 10 eyes with reduced vision had abnormal structural outcomes. Six eyes with normal fundal structure had visual loss associated with problems such as amblyopia, strabismus, and nystagmus, thus emphasising the importance of long term follow up of these children regardless of structural outcome. Interestingly, one eye with normal fundal structure had unexplained reduced distance vision (0.4 logMAR). Ohlsson et al described similar cases with unexplained visual loss in a study of 12–13 year old Swedish children and diagnosed them as having subnormal visual acuity syndrome.20
Near vision has not previously been documented in eyes treated with diode laser for threshold ROP. Our laser group had an overall mean BCNVA of 0.39 logMAR. In the comparative analysis, the laser group did not differ significantly from the control group, suggesting that diode laser treatment does not adversely affect near visual acuity.
Within the laser treated group, BCDVA worse than 0.5 logMAR was consistently associated with poor contrast sensitivity. However, a significant correlation between BCDVA and contrast sensitivity was not evident for those eyes with BCDVA of 0.5 logMAR or better. As the Pelli‐Robson chart uses letters of low spatial frequency it is unaffected by mild visual acuity losses and, therefore, may not have been sensitive enough to detect subtle contrast sensitivity dysfunction in those eyes with small reductions in BCDVA.11 It also explains why even in the presence of a significant difference in terms of distance visual acuity there was no significant difference in contrast sensitivity between the modified laser and control groups. In future studies, it may be more appropriate to use tests such as the functional acuity contrast test (FACT) which employ several spatial frequencies and are capable of detecting small changes in contrast sensitivity.21
Fifty per cent of the laser treated eyes were myopic with 35% having more than 4D of myopia. Ospina et al reported similar results with 62% of their laser treated eyes being myopic and 48% having more than 4D of myopia.17 Only 21% of our subthreshold untreated eyes were myopic; all were less than −1D. As increasing severity of ROP has been shown to contribute to the development of myopia, it is likely that the increased myopia in the laser group was the result of the more severe ROP in these eyes.22 It is not possible from our study to determine whether the diode laser treatment itself contributed to the myopia in the treated patients.
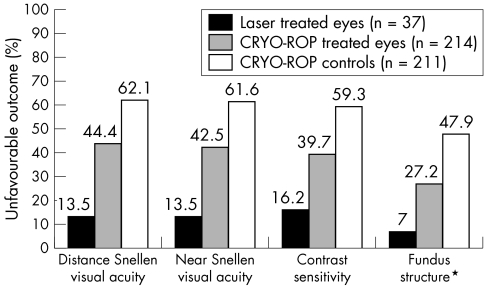
Figure 3 compares the unfavourable outcome rate of our laser treated eyes with the 10 year outcome data from the CRYO‐ROP study.1,2 The data show an overall reduction in unfavourable outcomes of 69.6% for distance acuity, 68.2% for near acuity, 59.2% for contrast sensitivity, and 74.3% for fundus structure in eyes treated with diode laser compared with eyes treated with cryotherapy for threshold ROP. The underlying reason for this difference in long term visual outcome after these two treatments is not clear. We are aware that this comparative analysis is potentially biased as the CRYO‐ROP eyes are historical controls. Many advances in perinatal medicine have occurred since the switch to laser treatment for threshold ROP. These advances may be responsible for the improved ocular outcomes for severe ROP rather than the change in treatment. Furthermore, the CRYO‐ROP patients differed from our laser cohort in terms of mean birth weight (799 (166) g v 889 (184) g, respectively) although the mean gestational ages of both groups were similar (26.3 (1.8) weeks v 26.5 (1.7) weeks, respectively). However, Ng et al also concluded from a randomised prospective trial of cryotherapy versus laser therapy in eyes with threshold ROP that laser treated eyes had better structural and functional outcome compared with eyes treated with cryotherapy.19 They also noted that eyes which received cryotherapy were more likely to develop macular dragging, which was associated with poorer visual acuities, and speculated that the more widespread nature of the thermal injury from cryotherapy accounts for the additional dragging in these patients.
Figure 3 Comparison with CRYO‐ROP results. *For fundus structure outcome, the number of patients in each group was 43, 217, and 215 for laser treated eyes, CRYO‐ROP treated eyes, and CRYO‐ROP controls respectively.
It is interesting that the two eyes which developed stage 5 ROP in our study belonged to a child who had documented zone I rush disease which progressed despite laser treatment. Although treatment proved to be efficacious in zone II threshold disease in the CRYO‐ROP study, it was disappointing in zone I threshold disease with 90% having an unfavourable outcome.16,23
Our study has several limitations; the numbers are relatively small, our controls had less severe ROP at outset and, because of cognitive impairment in three patients, there was variable participation in the different examinations performed. While we recognise these limitations, we nevertheless think that this study provides valuable information regarding the long term benefits of diode laser photocoagulation in the treatment of threshold ROP. At a mean follow up of 11 years, patients who received diode laser photocoagulation for threshold ROP had a satisfactory visual outcome with 73% of eyes achieving 6/12 or better distance vision and 67.6% achieving 6/12 or better near vision. Only 7% had poor structural outcome. Laser treated eyes with favourable structural outcome have a good visual outcome. Our results show no adverse effect from the diode laser on near vision, contrast sensitivity, or colour vision.
Abbreviations
BCDVA - best corrected distance visual acuity
BCNVA - best corrected near visual acuity
CS - contrast sensitivity
IVH - intraventricular haemorrhage
ROP - retinopathy of prematurity
Footnotes
The corresponding author declares on behalf of all authors that there are no competing interests.
References
- 1.Cryotherapy for Retinopathy of Prematurity Cooperative Group Multicenter trial of cryotherapy for retinopathy of prematurity. Ophthalmological outcomes at 10 years. Arch Ophthalmol 20011191110–1118. [DOI] [PubMed] [Google Scholar]
- 2.Cryotherapy for Retinopathy of Prematurity Cooperative Group Contrast sensitivity at age 10 years in children who had threshold retinopathy of prematurity. Arch Ophthalmol 20011191129–1133. [DOI] [PubMed] [Google Scholar]
- 3.Laser ROP Study Group Laser therapy for retinopathy of prematurity. Arch Ophthalmol 1994112154–156. [DOI] [PubMed] [Google Scholar]
- 4.McNamara J A, Tasman W, Brown G C.et al Laser photocoagulation for stage 3+ retinopathy of prematurity. Ophthalmology 199198576–580. [DOI] [PubMed] [Google Scholar]
- 5.White J, Repka M X. Randomised comparison of diode laser photocoagulation versus cryotherapy for threshold retinopathy of prematurity: 3‐year outcome. J Pediatr Ophthalmol Strabismus 19973483–87. [DOI] [PubMed] [Google Scholar]
- 6.O'Keefe M, O'Reilly J, Lanigan B. Longer term visual outcome of eyes with retinopathy of prematurity treated with cryotherapy or diode laser. Br J Ophthalmol 1998821246–1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Report of a joint working party of the Royal College of Ophthalmologists and British Association of Perinatal Medicine Retinopathy of prematurity: guidelines for screening and treatment. Early Hum Dev 199646239–258. [PubMed] [Google Scholar]
- 8.McGinnity F G, Bryars J H. Controlled study of ocular morbidity in school children born preterm. Br J Ophthalmol 199276520–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dowdeswell H J, Slater A M, Broomhall J.et al Visual deficits in children born at less than 32 weeks gestation with and without ocular pathology and cerebral damage. Br J Ophthalmol 199279447–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O'Connor A R, Stephenson T J, Johnson A.et al Visual function in low birth weight children. Br J Ophthalmol 2004881149–1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pelli D G, Robson J G, Wilkins A J. The design of a new letter chart for measuring contrast sensitivity. Clin Vis Sci 19882187–199. [Google Scholar]
- 12.Elliot D B, Bullimore M A, Bailey I L. Improving the reliability of the Pelli‐Robson contrast sensitivity test. Clin Vis Sci 19916471–475. [Google Scholar]
- 13.Powls A, Botting N, Cooke R W.et al Visual impairment in very low birthweight children. Arch Dis Child 199776F82–F87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hungerford J, Stewart A, Hope P. Ocular sequelae of preterm birth and their relation to ultrasound evidence of cerebral damage. Br J Ophthalmol 198670463–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Birch J. Clinical use of the American Optical Company (Hardy, Rand & Ritter) pseudoisochromatic plates for red‐green colour deficiency. Ophthalmic Physiol Opt 199717248–254. [PubMed] [Google Scholar]
- 16.Cryotherapy for Retinopathy of Prematurity Cooperative Group Multicenter trial of cryotherapy for retinopathy of prematurity. Preliminary results. Arch Ophthalmol 1988106471–477. [DOI] [PubMed] [Google Scholar]
- 17.Ospina L H, Lyons C J, Matsuba C.et al Argon laser photocoagulation for retinopathy of prematurity: long term outcome. Eye 2004181–6. [DOI] [PubMed] [Google Scholar]
- 18.Shalev B, Farr A K, Repka M X. Randomised comparison of laser photocoagulation versus cryotherapy for retinopathy of prematurity: seven year outcome. Am J Ophthalmol 200113276–80. [DOI] [PubMed] [Google Scholar]
- 19.Ng E, Connolly B P, McNamara J A.et al A comparison of laser photocoagulation with cryotherapy for threshold retinopathy of prematurity at 10 years. Part 1: Visual function and structural outcome . Ophthalmology 2002109928–935. [DOI] [PubMed] [Google Scholar]
- 20.Ohlsson J, Villarreal G, Sjostrom A.et al Visual acuity, residual amblyopia and ocular pathology in a screened population of 12–13 year old children in Sweden. Acta Ophthalmol Scand 200179589–595. [DOI] [PubMed] [Google Scholar]
- 21.Ginsburg A P.Functional acuity contrast test (FACT). Chicago IL: Stereooptical Co Inc, 1993
- 22.Quinn G E, Dobson V, Repka M X.et al Cryotherapy for Retinopathy of Prematurity Cooperative Group. Development of myopia in infants with birth weights less than 1251 grams. Ophthalmology 199299329–340. [DOI] [PubMed] [Google Scholar]
- 23.Cryotherapy for Retinopathy of Prematurity Cooperative Group Multicenter trial of cryotherapy for retinopathy of prematurity: 3½‐year outcome‐structure and function. Arch Ophthalmol 1993111339–344. [PubMed] [Google Scholar]