Abstract
Aims
To determine long term graft survival rates and visual results for different indications for penetrating keratoplasty from a single institution over 10 years and compare these to national outcome data.
Methods
Retrospective chart analysis. 784 records were available for review of 1096 consecutive penetrating keratoplasty procedures performed between 1990 and 1999 (72%). Outcomes of graft survival, visual acuity, and astigmatism were analysed and compared to national outcome data supplied by the UK Transplant Service.
Results
At 5 year follow up, overall graft survival was 66%. This was subdivided into 98% for keratoconus, 86% for viral keratitis, 85% for Fuchs' dystrophy, 84% for pseudophakic bullous keratopathy, 55% for regrafts, and 57% for other diagnoses. There was a significantly higher graft survival rate for all diagnostic subgroups except Fuchs' dystrophy at 3 years of follow up compared to the national average. Best corrected visual acuity at 5 years was 6/18 or better in 53% of cases. The mean keratometric astigmatism was 3.4 dioptres.
Conclusion
Penetrating keratoplasty is a safe and effective treatment for selected corneal disorders. Penetrating keratoplasty for viral keratitis may achieve good results with long term antiviral treatment. Patients may achieve better outcomes if their surgery is performed at specialist centres.
Keywords: corneal transplantation, keratoplasty, penetrating, graft survival
Corneal transplantation is one of the most commonly performed allograft transplantations in the United Kingdom, with 2365 performed over 12 months in 2003–4.1 Many series have been published describing graft survival and risk factors for graft survival.2,3,4,5,6,7,8,9,10 Relatively few series have long term follow up of large numbers of patients with analysis of graft survival, postoperative astigmatism, and visual acuity based on preoperative diagnosis.11,12 The primary objective of this study was to evaluate long term corneal transplant outcome at our institution in terms of graft survival and visual acuity and compare these to national outcome data. The secondary objectives were to examine the influence of preoperative diagnosis on graft survival and astigmatism.
Patients and methods
The study methodology was a retrospective non‐comparative chart review. A total of 1096 patients underwent penetrating keratoplasty (PK) at the Queen Victoria Hospital, East Grinstead between 1990 and 1999. The corneoplastic unit at the Queen Victoria Hospital is a tertiary referral corneal unit that performs a large number of repeat and complicated PKs. Records of 784 PKs were available for review (72%). Follow up data were not available for 312 patients whose charts were destroyed when they did not attend the hospital for a prolonged period; this was usually because they were referred back to their referring institution, lived overseas, or were dead. Standard forms from United Kingdom Transplant (UKT) were used to collect data. Visual acuity (VA) was recorded preoperatively, and was compared with VA at 1 year and at 5 years of follow up. Astigmatism was taken from keratometry readings at the 5 year follow up or if not available, results were taken from last follow up available. Astigmatism results were analysed according to diagnosis categories. Survival rates were available for up to 8 years of follow up. Our survival results are reported for 5 years for ease of comparison with other studies. Grafts were considered to have failed if they became irreversibly opacified having been clear initially following surgery.
The technique for PK changed in 1994 when there was a change in consultant. From 1990 to 1993, techniques included freehand recipient trephination as well as use of the Krumeich guided trephine system (Rhein Medical). From 1994, freehand trephination became standard practice and donors were prepared using the Iowa PK Press (Bausch & Lomb). Donor corneas were stored in tissue culture medium (Optisol GS) for up to 7 days or organ culture medium for up to 28 days before surgery. From 1994 all grafted patients with underlying herpes simplex virus (HSV) received prophylactic oral antiviral coverage indefinitely (aciclovir 400–800 mg daily). Postoperative steroid drops were tapered over 6 months, and pseudophakic patients remained on long term low dose topical steroid unless there was a pressure rise. Most cases of regrafts had the initial graft performed elsewhere and were referred to our institution for repeat keratoplasty.
Nationwide outcome data for PKs were supplied by UKT. Data supplied included 3 year graft survival rates for 5856 patients. These data were collected from PKs performed in the United Kingdom between April 1999 and October 2003 and collated from standard follow up forms filled in at the time of surgery and periodic postoperative visits (1, 2, 3, and 5 years) by the operating unit. Outcomes were subdivided by preoperative diagnostic categories (personal communication, unpublished data).
Data were stored in a Microsoft Access database and analysed using SPSS statistical software. Kaplan‐Meier survival curves were used to determine graft survival rates for each main indication for keratoplasty. Follow up for probability of survival ranged from 1–100 months. Survival rates for the main indications for keratoplasty were compared using the Breslow and Mantel‐Cox (log rank) tests. Significance of diagnoses on astigmatism was assessed using the Kruskal‐Wallis test. Significance of differences between our results and national averages was determined by Fisher's exact test.
Results
Descriptive statistics
In all, 784 cases of PK were available for review; 54.7% were male and 45.3% were female. The mean age was 54.2 years with a standard deviation of 21.5 years. The indications for corneal transplant were 40.9% regrafts, 15.0% keratoconus, 9.3% Fuchs' endothelial dystrophy, 7.6% pseudophakic bullous keratopathy (PBK), 5.9% viral keratitis (herpes simplex and herpes zoster), and 21.3% other diagnoses. Detailed analysis of preoperative diagnosis, indications and subgroups for regrafting and surgical procedures performed at the same time as PK for this patient series has been published previously.13
Visual acuity
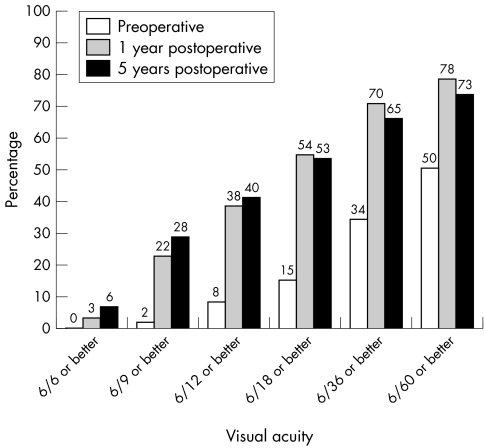
Figure 1 shows the best corrected visual acuity (BCVA) distribution preoperatively and at 1 year and 5 year follow up for all cases.
Figure 1 Best corrected visual acuity outcomes.
Astigmatism
The mean keratometric astigmatism was 3.4 dioptres. This was divided into 3.3 dioptres for keratoconus, 2.9 dioptres for viral keratitis, 2.6 dioptres for Fuchs' dystrophy, 2.3 dioptres for PBK, and 4.2 dioptres for regrafts. There was no statistically significant effect of preoperative diagnosis on the amount of astigmatism (p>0.05).
Survival analysis
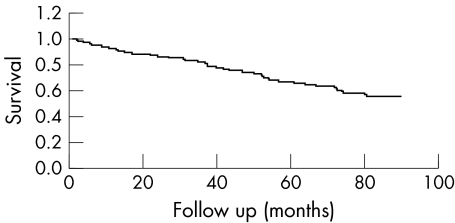
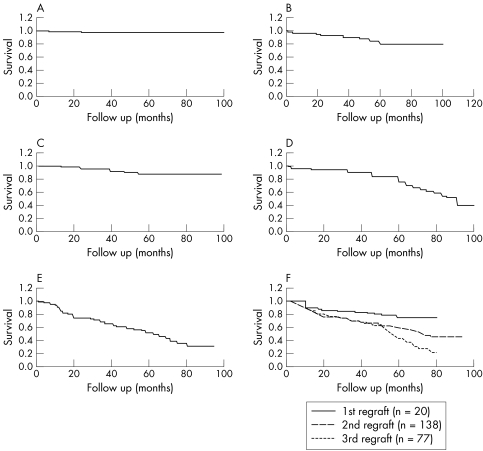
The overall graft survival at 5 year follow up was 66% (fig 2). At 5 year follow up, keratoconus had a survival rate of 98%, viral keratitis had a survival rate of 86%, Fuchs' dystrophy 85%, PBK 84%, and regrafts 55% (fig 3A–E). The regraft subgroup comprised 6% first regraft, 43% second regraft, 24% third regraft, and 27% four or more regrafts. Figure 3F shows the breakdown of survival rates for first, second, and third regrafts which were 80%, 60%, and 44% at 5 years, respectively. Graft survival for four or more regrafts was 52% at 5 years. Keratoconus showed a statistically significant higher survival rate compared with the other groups in the study (p<0.0001). Regrafts had a lower survival rate compared to all other groups combined (p<0.0001). At 5 year follow up, there was no statistically significant difference in the survival rates among Fuchs' dystrophy, PBK, and HSV (p>0.05). The survival rate for PBK decreased from 84% at 5 years to 42% by 8 years. This difference was statistically significant (p<0.001).
Figure 2 Kaplan‐Meier survival curve for all cases.
Figure 3 (A) Kaplan‐Meier survival curve for keratoconus. (B) Kaplan‐Meier survival curve for Fuchs' dystrophy. (C) Kaplan‐Meier survival curve for viral keratitis. (D) Kaplan‐Meier survival curve for pseudophakic bullous keratopathy. (E) Kaplan‐Meier survival curve for all regrafts. (F) Kaplan‐Meier survival curve for first, second, and third regrafts.
Comparison to national outcome data
Graft survival data at 3 years of follow up for 5856 eyes were provided by UKT. Diagnostic subgroup numbers were 1330 for keratoconus (23%), 1157 for Fuchs' dystrophy (20%), 964 for previously failed graft (16%), 920 for PBK (16%), 265 for viral keratitis (4%), and 1220 for others (21%). Table 1 shows graft survival data supplied by UKT compared to the 3 year survival rates from our centre. Graft survival rates were statistically significantly higher at our institution for all diagnostic subgroups except Fuchs' dystrophy. The overall graft survival was however not statistically different between our centre and UKT data. This is the result of the high number of repeat grafts performed at our centre compared to the national average, which skews the survival data because of their relatively poor outcome.
Table 1 Three year graft survival rates for national outcome data (UKT) and Queen Victoria Hospital (QVH).
| Diagnosis | UKT 3 year graft survival rates (%) | QVH 3 year graft survival rates (%) | p Value |
|---|---|---|---|
| Keratoconus | 93 | 98 | 0.019 |
| PBK | 65 | 90 | 0.00003 |
| Fuchs' dystrophy | 87 | 90 | 0.47 |
| Viral keratitis | 77 | 95 | 0.002 |
| Regrafts | 57 | 67 | 0.002 |
| Total | 79 | 81 | 0.15 |
Discussion
Penetrating keratoplasty is an effective treatment for selected corneal disorders, however, appropriate preoperative preparation, operative technique, and postoperative care influence long term outcomes. As demonstrated in a previous publication reporting the indications for penetrating keratoplasty in this series, the type of patients treated at this tertiary referral centre were a little more complex with higher rates of regrafts (40%).13 Nevertheless, over one half of the patients in this series of complicated patients achieved BCVA acuity of 6/18 or better.
We did not find any relation between preoperative diagnosis and postoperative astigmatism. This confirms that surgical factors such as trephination, graft placement and suture technique are among the most important factors in determining what the postoperative astigmatism will be.
Overall graft survival was 66% at 5 years. This is heavily influenced by the relatively low survival rate for regrafts, which made up 40.9% of cases. Graft survival was significantly worse for regrafts than all other groups combined. Survival rates for grafts for keratoconus, Fuchs' dystrophy, and pseudophakic bullous keratopathy were comparable with previously published series.5,6,7,8,12,14 These findings confirm that these indications for corneal transplantion do relatively well. The survival rate for pseudophakic bullous keratopathy was good compared to previously published rates at 5 years.2,5 With longer follow up, however, graft survival dropped to 42% by 8 years. The initially good results may be because of surgical technique or long term postoperative use of topical steroids. The long term reduction in graft survival suggests a gradual effect on the graft, due to chronic inflammation, the presence of the artificial intraocular lens, or a host rim heavily depleted of endothelial cells. Many of these patients also had trans‐sclerally sutured posterior chamber IOLs (57%) and extensive anterior segment reconstruction.
The survival rate for post‐herpetic corneal transplants of 86% at 5 years compares favourably with other published series. Cobo et al demonstrated a survival rate of 62% at 5 year follow up.15 Epstein et al have reported probability of survival for transplants following HSV as 75.6% at 2 years and 73.2% at 4 years and 6 years.16 Ficker et al had a probability of survival of 54% for first grafts done for HSV at 5 years follow up.17 We attribute the higher survival rate in our series to widespread indefinite use of oral antivirals postoperatively. Following initial dosing of aciclovir 400 mg four times daily postoperatively, this was tapered over the following 12 months to 400 mg aciclovir orally once daily in the majority of recipients. In addition, careful preoperative selection is important. Patients were typically grafted at least 6 months after their latest active viral episode and were not grafted if they had complete corneal anaesthesia. Van Rooij et al have recently demonstrated increased corneal transplant survival in a randomised trial of prophylactic oral aciclovir in cases of HSV keratitis.18 UKT analysing national data between April 1999 and October 2003 also demonstrated the value of antiviral prophylaxis in long term survival in grafts. Overall national survival of grafts at 5 years was less than 70% in both groups; however, the duration and dose of antivirals was not provided in this analysis.19
Long term survival for repeat corneal transplantation drops off rapidly with increasing number of previous transplants. This is in accordance with previously published studies.20,21 Particularly after two or more previous transplants, the chance of graft failure is much higher. Consideration should be given to additional immunosuppression in these patients, such as systemic prednisolone or ciclosporin A.22,23 We typically use ciclosporin A 1–3 mg per kg orally in patients at very high risk of graft failure. Early postoperative treatment with prednisolone (1 mg/kg) is also provided and rapidly tapered based on level of inflammation clinically. The majority of patients only received three daily doses in total.
Teenan et al, in a small series, showed higher graft survival following surgery by a corneal specialist compared to those performed by ophthalmologists performing relatively few PKs.3 Our study, with a much higher number of patients, confirms those findings. Graft survival after 3 years was significantly higher for all diagnostic subgroups except Fuchs' dystrophy at our specialist corneal centre compared to national average outcome data. This suggests that centres not performing large numbers of PKs should consider referring patients needing PK to specialist corneal units for their surgery, especially if the cases are not routine. This is particularly important given our confirmation of previous reports that patients having regrafts have significantly lower graft survival rates. A patient's first PK is the most likely to survive long term, and so all possible measures should be taken to ensure the first operation does well and is monitored through close surveillance in the postoperative period.
Abbreviations
BCVA - best corrected visual acuity
HSV - herpes simplex virus
PBK - pseudophakic bullous keratopathy
PK - penetrating keratoplasty
UKT - United Kingdom Transplant
VA - visual acuity
Footnotes
Competing interests: none.
References
- 1.UK Transplant Transplant activity report 2003–2004. 2004. p. 31.
- 2.Thompson R W, Jr, Price M O, Bowers P J.et al Long‐term graft survival after penetrating keratoplasty. Ophthalmology 20031101396–1402. [DOI] [PubMed] [Google Scholar]
- 3.Teenan D W, Sim K T, Hawksworth N R. Outcomes of corneal transplantation: a corneal surgeon vs the general ophthalmologist. Eye 200317727–730. [DOI] [PubMed] [Google Scholar]
- 4.Muraine M, Sanchez C, Watt L.et al Long‐term results of penetrating keratoplasty. A 10‐year‐plus retrospective study. Graefes Arch Clin Exp Ophthalmol 2003241571–576. [DOI] [PubMed] [Google Scholar]
- 5.Sit M, Weisbrod D J, Naor J.et al Corneal graft outcome study. Cornea 200120129–133. [DOI] [PubMed] [Google Scholar]
- 6.Ing J J, Ing H H, Nelson L R.et al Ten‐year postoperative results of penetrating keratoplasty. Ophthalmology 19981051855–1865. [DOI] [PubMed] [Google Scholar]
- 7.Williams K A, Muehlberg S M, Lewis R F.et al Long‐term outcome in corneal allotransplantation. The Australian Corneal Graft Registry. Transplant Proc 199729983. [DOI] [PubMed] [Google Scholar]
- 8.Williams K A, Muehlberg S M, Lewis R F.et al How successful is corneal transplantation? A report from the Australian Corneal Graft Register. Eye 19959(Pt 2)219–227. [DOI] [PubMed] [Google Scholar]
- 9.Vail A, Gore S M, Bradley B A.et al Clinical and surgical factors influencing corneal graft survival, visual acuity, and astigmatism. Corneal Transplant Follow‐up Study Collaborators. Ophthalmology 199610341–49. [DOI] [PubMed] [Google Scholar]
- 10.Vail A, Gore S M, Bradley B A.et al Corneal graft survival and visual outcome. A multicenter study. Corneal Transplant Follow‐up Study Collaborators. Ophthalmology 1994101120–127. [DOI] [PubMed] [Google Scholar]
- 11.Jonas J B, Rank R M, Budde W M. Visual outcome after allogenic penetrating keratoplasty. Graefes Arch Clin Exp Ophthalmol 2002240302–307. [DOI] [PubMed] [Google Scholar]
- 12.Claesson M, Armitage W J, Fagerholm P.et al Visual outcome in corneal grafts: a preliminary analysis of the Swedish Corneal Transplant Register. Br J Ophthalmol 200286174–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Al‐Yousuf N, Mavrikakis I, Mavrikakis E.et al Penetrating keratoplasty: indications over a 10 year period. Br J Ophthalmol 200488998–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lim L, Pesudovs K, Coster D J. Penetrating keratoplasty for keratoconus: visual outcome and success. Ophthalmology 20001071125–1131. [DOI] [PubMed] [Google Scholar]
- 15.Cobo L M, Coster D J, Rice N S.et al Prognosis and management of corneal transplantation for herpetic keratitis. Arch Ophthalmol 1980981755–1759. [DOI] [PubMed] [Google Scholar]
- 16.Epstein R J, Seedor J A, Dreizen N G.et al Penetrating keratoplasty for herpes simplex keratitis and keratoconus. Allograft rejection and survival. Ophthalmology 198794935–944. [DOI] [PubMed] [Google Scholar]
- 17.Ficker L A, Kirkness C M, Rice N S, Steele A D. Longterm prognosis for corneal grafting in herpes simplex keratitis. Eye 19882(Pt 4)400–408. [DOI] [PubMed] [Google Scholar]
- 18.Van Rooij J, Rijneveld W J, Remeijer L.et al Effect of oral acyclovir after penetrating keratoplasty for herpetic keratitis: a placebo‐controlled multicenter trial. Ophthalmology. 2003;110: 1916–9; discussion, 1919 [DOI] [PubMed]
- 19.Jones M M A, Collett D. Males JJ, et al. The use of antiviral prophylaxis following corneal grafts. http://www.uktransplant.org.uk/ukt/statistics/presentations/pdfs/april_05/viral_poster.pdf
- 20.Kirkness C M, Ezra E, Rice N S.et al The success and survival of repeat corneal grafts. Eye 19904(Pt 1)58–64. [DOI] [PubMed] [Google Scholar]
- 21.Weisbrod D J, Sit M, Naor J.et al Outcomes of repeat penetrating keratoplasty and risk factors for graft failure. Cornea 200322429–434. [DOI] [PubMed] [Google Scholar]
- 22.Hill J C. High risk corneal grafting. Br J Ophthalmol 200286945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reinhard T, Sundmacher R, Heering P. Systemic ciclosporin A in high‐risk keratoplasties. Graefes Arch Clin Exp Ophthalmol 1996234(Suppl 1)S115–S121. [DOI] [PubMed] [Google Scholar]