Abstract
Aim
To report on the diagnosis of intraocular lymphoma by aqueous cytology.
Methods
Four patients suspected of having intraocular lymphoma were evaluated by anterior chamber (AC) paracentesis with cytology (cytospin technique). All had a history of non‐ocular lymphoma and presented with at least one plus anterior chamber cells despite intensive glucocorticoid therapy. A 25 gauge needle was inserted through clear cornea (bevel up), over the iris stroma, so as to drain the AC. The aqueous humour was sent for cytopathology (cytospin technique), culture, and sensitivity tests.
Results
All procedures were diagnostic. Three were lymphoma and the fourth was culture positive for Propionibacterium endophthalmitis. No secondary glaucoma, hyphaema, cataract or infections were related to AC paracentesis.
Conclusions
In this series, AC aspiration cytology enhanced by the cytospin technique was an effective, minimally invasive alternative to vitrectomy based biopsy. This technique should be considered to rule in the diagnosis of intraocular lymphoma in selected cases with cells in the anterior chamber.
Keywords: lymphoma, eye, biopsy, cytology, cytospin
Intraocular lymphoma can involve the uveal tract, subretinal space, retina, vitreous, and aqueous humour.1 Ultrasonographic evidence of intraocular invasion includes vitritis (77%), choroidal scleral thickening (46%), widening of the optic nerve (31%), elevated chorioretinal lesions (23%), and retinal detachment (15%).2 Suspected patients are evaluated for synchronous central nervous system (CNS) disease. Computed tomography (CT) of the brain may reveal isodense or hyperdense lesions, while magnetic resonance imaging (MRI) may reveal lesions that are hypointense on T1 and hyperintense on T2 weighted images.3 Cerebrospinal fluid (CSF) should be sent for cytological, chemical, and cytokine analysis.4
Intraocular lymphoma is most commonly diagnosed by vitrectomy.1 Reported complications include retinal breaks, detachment, and cataract. Less common PPV related complications include vitreous haemorrhage, massive fibrin accumulation, anterior segment neovascularisation, endophthalmitis, sympathetic ophthalmia, and recurrent corneal erosion.5 Fine needle aspiration biopsy (FNAB) of the vitreous and chorioretinal biopsy has also been used.6,7 Chorioretinal biopsy typically demonstrates tumour cells between the RPE and Bruch's membrane.6
Cytology, cell marker, and cytokine studies each can be used to establish the diagnosis of intraocular lymphoma.8 Such lymphomas are typically composed of monoclonal lymphocytes that stain for B cell markers such as CD19, CD20, and CD22. Cytomorphology, immunohistochemistry, and flow cytometry are employed as possible.8,9
This study examines the use of anterior chamber (AC) paracentesis cytology (with cytospin technique), culture, and sensitivity in cases of suspected intraocular lymphoma. Here we describe our surgical approach, cytological techniques, results, and complications.
Materials and methods
This study was conducted respecting the tenets of the Declaration of Helsinki. Each patient signed a treatment consent and Health Insurance Portability and Accountability Act of 1996 (HIPAA) form.
Anterior chamber biopsy technique
Patients were cleared for local anaesthesia with sedation, brought to the operating room, prepared, and draped utilising sterile technique. Anaesthetic blocks were placed, a speculum retracted the eyelids, and a 0.3 forceps was used to stabilise the eye. A 25 gauge needle was introduced (bevel up) through clear cornea over the iris stroma. The lens was avoided. Aqueous humour (0.1–0.2 ml) was withdrawn into a 3 ml syringe. Balanced salt solution was used to reform the chamber. A repeat paracentesis was performed. Drops of specimen were placed on a glass slide for Gram stain and culture medium. The bulk of the specimen was left in the syringe needle complex for cytological testing. Cytopathological evaluations were immediately performed.
Cytospin technique
The cytospin technique was used to maximise the yield of cells from the biopsy specimen. Our technique involves the use of cytospin slides that are cleaned with alcohol and assembled with a slide filter card and sample delivery chamber, secured by a metal clip. Typically, up to 0.4 ml of fluid sample (3–5 drops) was added to the chamber together with an equal amount of cytospin collection fluid. Cytospin slides, filter cards, sample chambers, metal clips, and collection fluid were all obtained from Thermo‐Shandon, Pittsburgh, PA, USA. After spinning at 1800 rpm for 2 minutes, slides were removed from the cytospin chamber, further fixed in cytology fixative (70% alcohol/formalin), and stained with haematoxylin and eosin.
Establishing monoclonality
In general, we were not able to establish monoclonality of the lymphocytes harvested with this technique. If we were able to retrieve several micrograms of tissue, IL‐10/IL‐6 ratios could have been performed by such molecular analysis as polymerase chain reaction (PCR). If were able to obtain more than 100 000 cells in a saline suspension, flow cytometry would have been employed. When we were able to harvest hundreds of cells in one cell block, we used immunohistochemistry.
In this series, most cases involved an analysis of morphology on a limited number of cells. Cytomorphological analysis requires the pathologist to form an impression about the monotony of cells. In practice, morphological analysis is combined with clinical information (for example, patient history and radiological imaging studies). Cytomorphology can be diagnostic of lymphoma.
Results
Case 1
A 49 year old man presented in his seventh year of remission from central nervous system (CNS) non‐Hodgkin's lymphoma. His visual acuity was 20/20 in the right eye and 20/30 in the left. Slit lamp biomicroscopy revealed fine filamentous keratoprecipitates (KP) and vitreous cells in both eyes. Magnetic resonance imaging (MRI) of the brain and orbits revealed no enhancing lesions. B‐scan ultrasonography revealed posterior vitreous detachment and vitreous cells in both eyes. Fluorescein angiography revealed normal filling of the choroid, major arteries, and veins of the retinas and optic nerves of both eyes.
Though cytology of his CSF was negative, intraocular lymphoma was still suspected. After being non‐responsive to 3 months of topical steroid treatment, he consented to an AC aqueous biopsy.
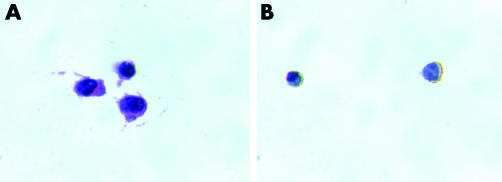
Cytopathology revealed a monotonous population of atypical lymphoid cells with irregular nuclear contours diagnostic of malignant lymphoma (fig 1). The patient received biweekly systemic chemotherapy followed by external beam radiation therapy (EBRT) for his ocular disease. Nine months after his ocular diagnosis, the anterior chamber and the vitreous contained few residual cells.
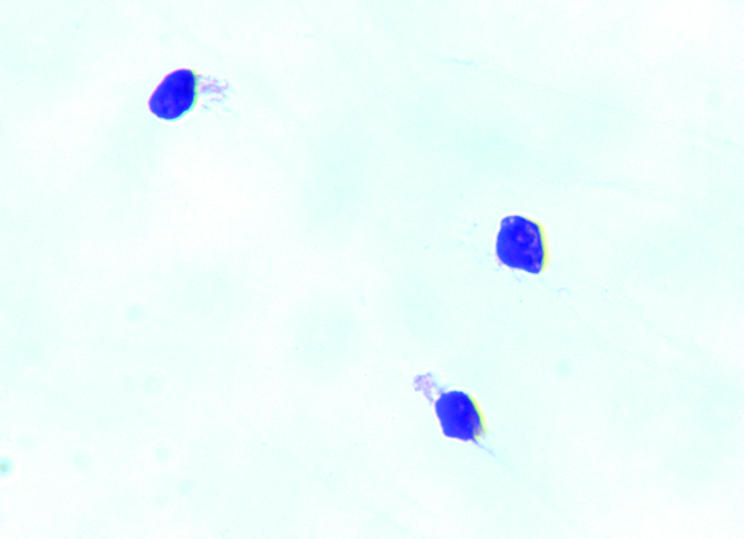
Figure 1 Case 1. Cytological evaluation of the anterior chamber fluid revealed a monotonous population of atypical lymphoid cells with irregular nuclear contours consistent with a diagnosis of malignant lymphoma (haematoxylin and eosin staining; original magnification ×100).
Case 2
An 83 year old woman with a history of B cell CNS lymphoma had been treated to remission with systemic chemotherapy. One year later, she was noted to have vitreous cells after cataract extraction from her left eye.
Her visual acuity was no light perception from her left eye; slit lamp examination revealed heterochromia, diffuse KP, and iris neovascularisation. Indirect ophthalmoscopy revealed a red haze and B‐scan ultrasonography showed a choroidal mass measuring 9.9×11.6 mm with a height of 6.0 mm. Aqueous biopsy was performed.
Cytopathology revealed CD20 staining B cells with large atypical lymphocytes with cytoplasmic membrane staining (fig 2). The stain for T cells showed irregular background staining. The left eye received EBRT (3600 cGy in 20 fractions) to control her B cell lymphoma.
Figure 2 Case 2. (A) Cytological evaluation revealed B cells with large atypical lymphocytes. (B) Immunohistochemical staining with CD20 demonstrated B cell atypical lymphocytes with cytoplasmic membrane staining (CD20 staining; original magnification ×100).
Case 3
A 60 year old man with had a history of cutaneous T cell lymphoma treated with chemotherapy (no previous ocular or CNS history of lymphoma). He presented with severe pain and decreased vision in his left eye. Examination of this right eye revealed a visual acuity of light perception, an intraocular pressure of 22 mm Hg and 3+ cells in the anterior chamber (with fibrin and scleritis). There was no ophthalmoscopic view into the eye and B‐scan revealed dense vitreous cells.
Aqueous paracentesis biopsy was diagnostic of lymphoma. The specimen revealed numerous medium sized monotonous malignant lymphocytes with moderate pleomorphism and focal necrotic cells (fig 3, left). In this case we could determine that the cells were T cell derived and CD4 positive while negative for CD3, CD5, CD7, CD8, CD56, and CD20 (fig 3, right). They were also positive for CD30 but not ALK 1 or EMA.
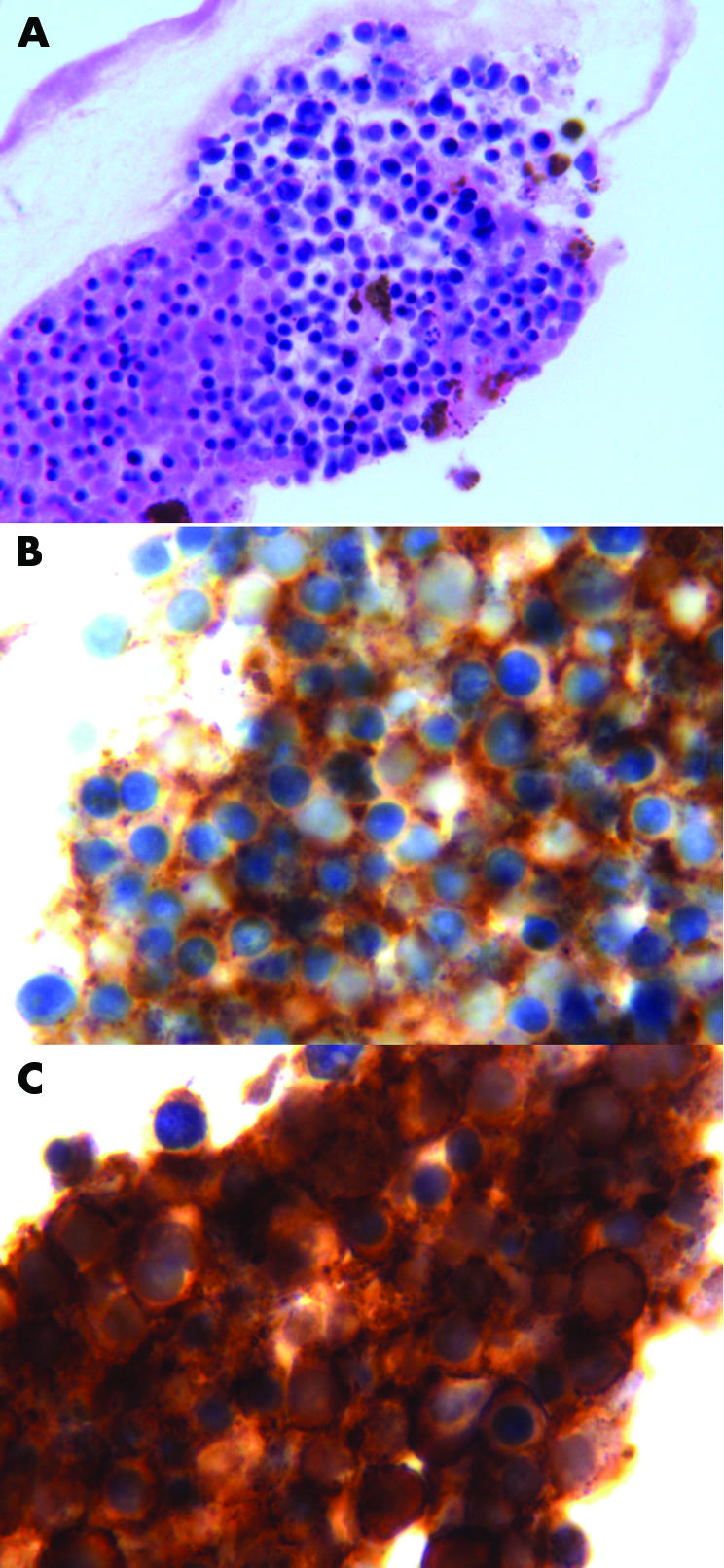
Figure 3 Case 3. (A) Cytological examination revealed numerous medium sized monotonous malignant lymphocytes with moderate pleomorphism and focal necrotic cells (haematoxylin and eosin staining; original magnification × 100). (B) Immunohistochemical staining demonstrated the cells were positive for CD 4 (CD 4 staining; original magnification × 100). (C) CD 30 positive (CD 30 staining; original magnification ×100).
Case 4
A 74 year old man with a 4 year history of systemic lymphoma was referred because of persistent cystoid macular oedema, vitritis and AC cells. He had undergone bilateral cataract extraction (3 and 4 months before our consultation) and was being treated with prednisolone acetate 1% and ketorolac tromethamine in both eyes. His visual acuity was 20/100 in both eyes. Slit lamp examination was significant for 4+ AC cells in both eyes (fig 4). Indirect ophthalmoscopy and photography with angiography revealed bilateral vitreous cells, multifocal choroidal thickening, macular and optic nerve oedema. B‐scan ultrasonography revealed vitreous cells in both eyes.
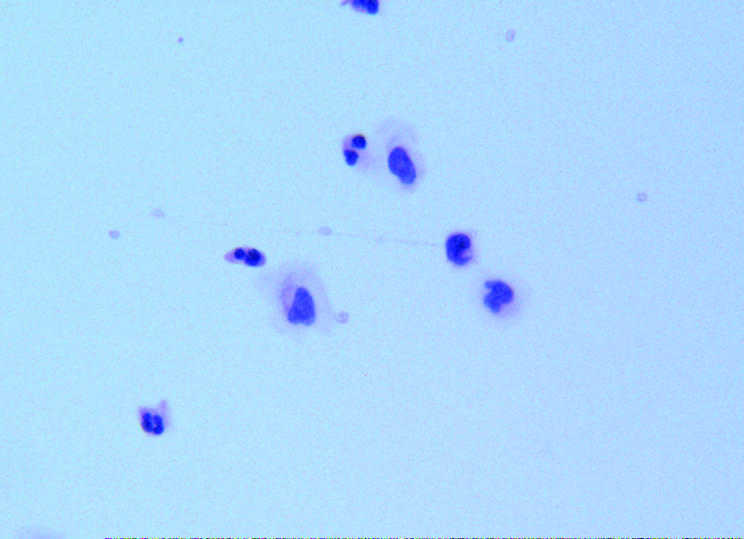
Figure 4 Case 4. Anterior chamber aqueous cytology demonstrated acute inflammatory cells without atypical lymphocytes (haematoxylin and eosin staining; original magnification × 40).
Anterior chamber paracentesis cytology revealed acute inflammatory cells without atypical lymphocytes. Though an immediate Gram stain was negative, Propionibacteriumacnes grew in subsequent culture studies. After intravitreal vancomycin in one eye and a vitrectomy in the other, he improved to 20/60 with persistent cystoid macular oedema in both eyes.
Discussion
Anterior chamber paracentesis biopsy was used to evaluate four patients with a history of systemic lymphoma and who were suspected of having intraocular lymphoma. We were able to obtain a diagnosis in all cases (3/3 were lymphoma). There were no acute operative or postoperative complications and no loss of visual acuity. One cataract developed within 1 year of biopsy (10 months after subsequent EBRT).
This study demonstrates that intraocular lymphoma can be diagnosed by fine needle “aqueous humour” biopsy. A review of previous individual case reports revealed that AC paracentesis of “hypopyon” was used to diagnose of lymphoma. For example, Corriveau reported a case of iritis with hypopyon that did not respond to steroid therapy. Fine needle aspiration of the hypopyon revealed abnormal lymphoid cells (with 60% monoclonal IgM kappa).10
We report on four cases where a clinical suspicion of intraocular lymphoma was present, aqueous cells were noted without hypopyon. This study suggests that paracentesis cytology (utilising an increased sensitivity offered by the cytospin technique) can be used to diagnose intraocular lymphoma. Therefore, it may be reasonable to perform an anterior chamber tap biopsy before performing a vitrectomy (in selected cases).
Abbreviations
AC - anterior chamber
CSF - cerebrospinal fluid
CT - computed tomography
EBRT - external beam radiation therapy
FNAB - fine needle aspiration biopsy
KP - keratoprecipitates
MRI - magnetic resonance imaging
Footnotes
Supported by The EyeCare Foundation and Research to Prevent Blindness, New York City, USA.
The authors have no proprietary interest in the products mentioned in this study. This work has not been published elsewhere.
References
- 1.Chan C C, Wallace D J. Intraocular lymphoma: update on diagnosis and management. Cancer Control 200411285–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ursea R, Heinemann M H, Silverman R H.et al Ophthalmic, ultrasonographic findings in primary central nervous system lymphoma with ocular involvement. Retina 199717118–123. [DOI] [PubMed] [Google Scholar]
- 3.DeAngelis L M. Brain Tumors. N Engl J Med 2001344114–123. [DOI] [PubMed] [Google Scholar]
- 4.Akpek E K, Ahmed I, Hochberg F H.et al Intraocular‐central nervous system lymphoma: clinical features, diagnosis and outcomes. Ophthalmology 19991061805–1810. [DOI] [PubMed] [Google Scholar]
- 5.Blumenkranz M S, Ward T, Murphy S.et al Applications and limitations of vitreoretinal biopsy techniques in intraocular large cell lymphoma. Retina 199299250–256. [DOI] [PubMed] [Google Scholar]
- 6.Kirmani M H, Thomas E L, Rao N A.et al Intraocular reticulum cell sarcoma: diagnosis by choroidal biopsy. Br J Ophthalmol 198771748–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lobo A, Lightman S. Vitreous aspiration needle tap in the diagnosis of intraocular inflammation. Ophthalmology 2003110595–599. [DOI] [PubMed] [Google Scholar]
- 8.Green W R. Diagnostic Cytopathology of ocular fluid specimens. Ophthalmology 198491726–749. [DOI] [PubMed] [Google Scholar]
- 9.Zaldivar R A, Martin D F, Holden J T.et al Primary intraocular lymphoma. Ophthalmology 20041111762–1767. [DOI] [PubMed] [Google Scholar]
- 10.Corriveau C, Easterbrook M, Payne D. Lymphoma simulating uveitis. Can J Ophthalmol 198621144–149. [PubMed] [Google Scholar]