Abstract
Background
Seasonal variation in the incidence of and mortality from myocardial infarction (MI) has been well recognised for many years. Haemopericardium (HP) is usually a fatal complication of MI. No data exist in the literature with regard to the seasonal variation in mortality from HP.
Aims
To perform a necropsy based study to confirm seasonal variation in mortality from MI in a London population and to determine whether seasonal variation in mortality from HP can be established.
Methods
Postmortem causes of death issued by several pathologists, working in two public London mortuaries over a five year period from 1999 to 2004 were analysed. Deaths caused by HP secondary to traumatic or iatrogenic causes were specifically excluded, as were deaths caused by HP secondary to bicuspid aortic valve and aortic dissection. The results were subdivided into winter (1 November to 31 March) and summer (1 April to 31 October).
Results
In total, there were 2266 cases of MI and 135 cases of HP. Significantly more deaths from HP (83 of 135; 61.5%; p = 0.004) and MI (1051 of 2266; 46.4%; p = 0.016) occurred in the five month winter period. Furthermore, there was a significantly higher incidence of HP compared with MI during the winter (83/1051; 7.9%) than the summer (52/1215; 4.3%; p<0.001). There was no significant difference in the age or sex of patients dying in either the winter or summer.
Conclusion
There is seasonal variation in mortality from both MI and HP in the London population, as confirmed by a postmortem study.
Keywords: myocardial infarction, postmortem, seasonal, haemopericardium, mortality
The propensity for a circadian pattern in the incidence of myocardial infarction (MI), with a peak in the early morning, has been known for some time, and the increase in mortality from MI in the winter months was first noticed and reported in the 1930s.1,2 Since these initial observations a large number of studies, varying in their approach and design, have confirmed that the incidence of MI and mortality from MI shows a seasonal variation.3,4,5,6 Some of these papers focused on the incidence of MI obtained from hospital admissions or used death certification data without postmortem confirmation, which are known to be inaccurate.7 Other studies have shown that although this variation holds true in temperate climates with seasonal variations in temperature, the pattern is lost in environments without temperature extremes.8 It seems that this peak winter incidence of MI is particularly applicable to older patients,9 and indeed it has been suggested that for patients younger than 45, there may be a spring peak in hospital admissions for MI.6
“We could find no published data relating to the seasonal variation in death as a result of haemopericardium”
Haemopericardium (HP) is a complication of MI caused by full thickness ventricular wall infarction and subsequent rupture into the pericardium. This is frequently the first cardiac event, and in one necropsy series it was the first and fatal cardiac event in 83% of patients.10 Consequently, we would expect the seasonal variation in the incidence of mortality from HP to follow a similar trend to the incidence of mortality from MI, for any given geographical population. We could find no published data relating to the seasonal variation in death as a result of HP. Therefore, we undertook the present retrospective review of postmortem confirmed cases of MI and HP over a five year period to determine whether such a variation could be established.
Materials and methods
Reports of every postmortem examination performed at two public mortuaries in the east end of London by several pathologists were analysed over a five year period from May 1999 to May 2004. We included all cases of acute MI and HP. However, for the HP group, we excluded all HP cases that were not a direct result of rupture of the ventricular wall caused by MI. This meant that traumatic and iatrogenic causes of HP and HP secondary to bicuspid aortic valve causing aortic dissection were excluded. We subdivided the results into two categories. Winter, if the deaths occurred in the five month period from the 1 November to 31 March, and summer if they occurred in the seven month period from the 1 April to 31 October. An independent samples t test was performed on the winter and summer groups for both the MI and HP cases to compare the mean numbers of HP and MI cases between the two seasons. This test was also performed to determine whether there was a difference in the mean age of the patients dying in the winter compared with the summer, and also whether the mean numbers of men and women dying in the two seasons were different. Finally, we analysed the data to determine whether the proportion of HP to MI varied between the two seasons.
Results
We investigated 2266 deaths caused by MI and 135 deaths caused by HP. One thousand and fifty one of the 2266 (46.4%) deaths from MI and 83 of the 135 (61.5%) deaths from HP occurred in the five winter months. In the winter period there was a mean increase of 36.63 MI cases/month and 8.97 HP cases/month compared with the summer period (table 1). Both of these results were significant.
Table 1 Mean number of HP and MI cases each month.
| Winter | Summer | Mean difference | 95% CI | p Value (2 tailed) | |
|---|---|---|---|---|---|
| HP (mean no cases/month) | 16.40 | 7.43 | 8.97 | 3.6 to 14.3 | 0.004 |
| MI (mean no cases/month) | 210.20 | 173.57 | 36.63 | 8.3 to 65.0 | 0.016 |
CI, confidence interval; HP, haemopericardium; MI, myocardial infarction.
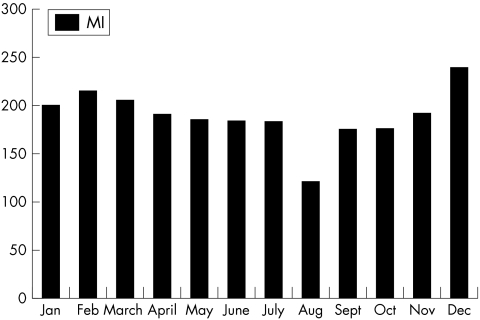
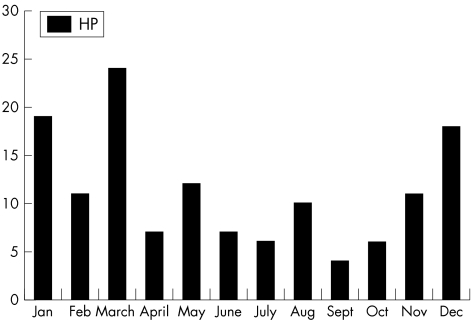
December was the month with the peak number of MI deaths (239 of 2266; 10.5%). There was a steady decline in the number of cases from February through to July, followed by a marked reduction in the number of MI cases in August. The autumnal months again saw a steady increase until December (fig 1). Figure 2 shows the monthly data for deaths from HP. There was a peak in the number of deaths from HP in March (24 of 135; 17.8%), and a general trend for lower numbers of deaths in the summer months and higher numbers in the winter months. In the winter period there were 83 deaths caused by HP out of a total number of 1051 deaths caused by MI (7.9%; 95% confidence interval, 6.3% to 9.6%). This compares with 52 of 1215 (4.3%; (95% confidence interval, 3.3% to 5.6%) in the summer period. The ranges do not overlap and the difference is significant (p < 0.001). Thus, a greater proportion of MIs are complicated by HP in the winter months than in the summer months.
Figure 1 Number of deaths caused by myocardial infarction (MI) each month.
Figure 2 Number of deaths caused by haemopericardium (HP) each month.
Given the known association of a spring peak of deaths from MI in young men,6 and the propensity for HP to be a primary fatal cardiac event in those with left ventricular free wall rupture,11 we analysed the March peak of patients dying from HP in more detail. Of the 24 patients in this group there were 14 men and 10 women and the average ages were 74.4 and 76.9 years (overall average, 75.4). Table 2 shows the average age of patients dying of each condition in either summer or winter, and also the sex of patients dying of each condition in either summer or winter. There was no significant difference in the ages of the patients dying from HP in March compared with the other winter months. Furthermore, there were no significant differences in either the age or sex of patients dying in winter compared with their summer counterparts.
Table 2 Analysis of sex and age variation between the two groups.
| Table 2 | HP winter | HP summer | HP March | MI winter | MI summer |
|---|---|---|---|---|---|
| Men (N) | 44 | 26 | 14 | 512 | 583 |
| Women (N) | 39 | 26 | 10 | 539 | 632 |
| Mean age (men) | 71.7 | 70.3 | 74.4 | 72.0 | 69.8 |
| Mean age (women) | 77.3 | 75.1 | 76.9 | 76.0 | 73.2 |
HP, haemopericardium.
Discussion
Our results show that death from MI and its complication of HP does show a seasonal variation for a London based population. This is to be expected, because HP is usually a direct complication of MI as a result of rupture of the ventricular wall. Seasonal variation in MI for a London population has been studied before,12 but this was based on patients admitted with MI to a coronary care unit, and thus measured the incidence, not the mortality from MI. To our knowledge, this is the first necropsy based analysis of London MI mortality data showing a positive seasonal correlation.
There are many hypotheses to explain the increased risk of MI in the winter months. Sympathetic tone is known to increase in cold weather13 and Bradley and colleagues12 showed that, with regard to the London population rate of MI admissions, not only was there a seasonal variation, but also there was a higher rate of admissions on colder summer days. The authors of these studies suggest that cold temperature per se plays a role, irrespective of the season. Haematological variables are also affected in the winter, with increases in β thromboglobulin and platelet factor 4, which in turn enhance platelet aggregation.14 Other studies have suggested that the increase in winter may be attributable to concurrent chest infections.15,16 Elderly patients are particularly prone to suffering from these additional risk factors and this may explain the increased seasonal variation in the older age groups. Although we did not demonstrate a significant difference in the age of patients dying during the winter months, as has been reported in other series,9 this may be because of the relatively small sample size of our study.
“The likelihood of ventricular wall rupture after myocardial infarction is greater in winter than in summer”
We have found no data in the literature to back up or contradict our other main finding of a parallel seasonal variation in the incidence of HP in the same London based population group. The peak incidence of HP was in March. This is interesting given the fact that in a necropsy study of 100 consecutive cases of left ventricular free wall rupture, the ruptured infarction represented the subject's first MI,10 and the observed spring peak in incidence of MI in young men.6 However, in our series the deaths from HP in March were not seen in younger patients than those that occurred in other months. Of the patients dying of MI over this five year study period, 135 of 2266 (6.0%) were complicated by HP. This figure is of a similar magnitude to the incidence of cardiac rupture in patients admitted to hospital with MI, which has been previously reported as 2.3%.17 In 89.6% of these patients the rupture was fatal. Perhaps of greater note, our data also show that the proportion of deaths from MI that were complicated by HP was significantly different between the two seasons (7.9% in winter and 4.3% in summer). Thus, the likelihood of ventricular wall rupture after MI is greater in winter than in summer. It may be that the general increase in baseline sympathetic tone in cold weather and the consequent increased force of cardiac contractility is more likely to rupture the vulnerable, newly formed infarct during the winter months.
Take home messages
In a postmortem study of an east London population, there were significantly more deaths from haemopericardium (HP) and myocardial infarction (MI) in the five month winter period than in the seven month summer period
There was no significant difference in the age or sex of patients dying from MI and HP in either the winter or summer
During winter a significantly higher number of MIs are likely to be complicated by HP
Our study is based on two mortuaries—both in east London—and may not be ethnically representative of the London population as a whole. However, it is the first necropsy based study on MI mortality in London and has confirmed that, as would be expected, a seasonal variation in mortality from MI and its complication of HP is present. Furthermore, during winter a significantly higher number of MIs are likely to be complicated by HP.
Acknowledgements
Thanks to E Stearns, HM Coroner for the Eastern District of Greater London, for her help and permission to present these findings and C Fernandez, Mayday Hospital, for his statistical input.
Abbreviations
HP - haemopericardium
MI - myocardial infarction
References
- 1.Masters A M, Dack S, Jaffe H L. Factors and events associated with onset of coronary artery thrombosis. JAMA 1937109546–549. [Google Scholar]
- 2.Rosahn P D. Incidence of coronary thrombosis. JAMA 19371091294–1299. [Google Scholar]
- 3.Gonzalez Hernandez E, Cabades O'Callaghan A, Cebrian Domenech J.et al Seasonal variations in admissions for acute myocardial infarction. The PRIMVAC study. Rev Esp Cardiol 20045712–19. [PubMed] [Google Scholar]
- 4.Spencer F A, Goldberg R J, Beckeret al Seasonal distribution of acute myocardial infarction in the second National Registry of Myocardial Infarction. J Am Coll Cardiol 1998311226–1233. [DOI] [PubMed] [Google Scholar]
- 5.Sharovsky R, Ce sar L A. Increase in mortality due to myocardial infarction in the Brazilian city of Sao Paulo during winter. Arq Bras Cardiol 200278106–109. [DOI] [PubMed] [Google Scholar]
- 6.Douglas A S, Dunnigan M G, Allan T M.et al Seasonal variation in coronary heart disease in Scotland. J Epidemiol Community Health 199549575–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alderson M R, Bayliss R I S, Clarke C A.et al Death certification. BMJ 1983287444–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ku C S, Yang C Y, Lee W J.et al Absence of a seasonal variation in myocardial infarction onset in a region without temperature extremes. Cardiology 199889277–282. [DOI] [PubMed] [Google Scholar]
- 9.Sheth T, Nair C, Muller J.et al Increased winter mortality from acute myocardial infarction and stroke. The effect of age. J Am Coll Cardiol 1999331916–1919. [DOI] [PubMed] [Google Scholar]
- 10.Batts K P, Ackermann D M, Edwards W D. Postinfarction rupture of the left ventricular free wall: clinicopathological correlates in 100 consecutive autopsy cases. Hum Pathol 199021530–535. [DOI] [PubMed] [Google Scholar]
- 11.Mann J M, Roberts W C. Rupture of the left ventricular free wall during acute myocardial infarction: analysis of 138 necroscopy patients and comparison with 50 necroscopy patients with acute myocardial infarction without rupture. Am J Cardiol 199862847–859. [DOI] [PubMed] [Google Scholar]
- 12.Bradley M, Kulasegaram R, Stevenson R.et al Circadian and seasonal factors in the pathogenesis of acute myocardial infarction: the influence of environmental temperature. Br Heart J 199369385–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hiramatsu K, Yamada T, Katakura M. Acute effects of cold on blood pressure, renin–angiotensin–aldosterone system, catecholamines and adrenal steroids in man. Clin Exp Pharmacol Physiol 198411171–179. [DOI] [PubMed] [Google Scholar]
- 14.Kawahara J, Sano H, Fukuzaki H.et al Acute effects of exposure to cold on blood pressure platelet function and sympathetic nervous system activity in humans. Am J Hypertens 19892724–726. [DOI] [PubMed] [Google Scholar]
- 15.Spodick D H, Flessas A P, Johnson M M. Association of acute respiratory symptoms with onset of acute myocardial infarction: prospective investigation of 150 consecutive patients and matched control patients. Am J Cardiol 198453481–482. [DOI] [PubMed] [Google Scholar]
- 16.Mattila K J. Viral and bacterial infections in acute myocardial infarction. J Intern Med 1989225293–296. [DOI] [PubMed] [Google Scholar]
- 17.Tanaka K, Sato N, Yasutake M.et al Clinical course, timing of rupture and relationship with coronary recanalization therapy in 77 patients with ventricular free wall rupture following acute myocardial infarction. J Nippon Med Sch 200269481–488. [DOI] [PubMed] [Google Scholar]