Abstract
Background
Gap junctions are intercellular channels composed of connexins, which mediate the direct passage of small molecules between neighbouring cells. They are involved in regulation of cell cycle, cell signalling, and differentiation, and probably invasion and metastasis. The role of connexins in the metastatic process is controversial, because some studies indicate that connexin expression is inversely correlated with metastatic capacity. In contrast, others demonstrate that connexins may be involved in metastasis. In addition, connexin status in breast cancer metastasis has not been widely studied.
Methods
We evaluated by immunohistochemistry the expression of connexin 26 (Cx26) and connexin 43 (Cx43) in primary breast tumours (PTs) and matched paired metastases to lymph nodes (MLNs).
Results
In PTs, we observed predominantly cytoplasmic localisation of evaluated connexins, indicating alterations in connexin expression in breast cancer cells. We demonstrated that expression of Cx26 and Cx43 was increased in MLNs compared with PTs (p<0.00001 and p<0.001, for CX26 and Cx43, respectively). In addition, Cx26 and Cx43 negative PTs developed Cx26 and Cx43 positive MLNs. Furthermore, besides increased cytoplasmic staining, enhanced membranous localisation of Cx43, typical of normal cells, was found in MLNs. Additionally, membranous Cx26 expression appeared only in metastatic breast cancer cells.
Conclusions
These findings suggest that connexins may contribute to the efficient metastasising of breast cancer to the lymph nodes.
Keywords: connexin 26, connexin 43, breast cancer, primary tumour, lymph node metastases
Gap junctional intercellular communication (GJIC) plays a critical role in tissue development, differentiation, and cell proliferation by regulation of signal transduction and the cell cycle. Previous studies suggested that loss of GJIC is an important event in tumour invasion,1,2 and metastasis.3,4,5 Each gap junction channel consists of two connexons, hexameric hemichannels belonging to the connexin family of structural proteins. Gap junctions are specialised cell membrane channels that allow small molecules (<1 kDa) and ions to flow from cell to cell.
To date, 20 different connexin isoforms have been found in humans.6 Three of them (Cx26, Cx32, and Cx43) have also been detected in normal rodent breast tissue. In normal human breast, Cx26 is present in the epithelium, mostly between the luminal cells of major ducts. Alveolar structures are less immunoreactive for this connexin. Cx43 expression was found between myoepithelial cells of ducts and a weaker immunoreactivity was associated with luminal/alveolar structures.7 GJIC is often impaired in cancerous cells and at tumour borders with surrounding normal tissue, thus decreased communication via gap junctions may be an important event in oncogenesis. In contrast, reconstitution of gap channels by upregulation of connexins has been shown to restore normal phenotypes and to retard tumour cell growth.8 Thus, the connexin genes have been classified as tumour suppressors.8 In several studies, lack of connexin expression and gap junction channel function was demonstrated in tumours.9,10,11 In addition to decreased connexin expressions, reduction in GJIC is often marked by aberrant localisation of connexins, for example, in the cytoplasm or nucleus of cancerous cells.12,13 Loss of GJIC could support growth of cancerous cells and enhance heterogeneity within the tumour cell population. It has been shown that disturbances in GJIC could provoke breast cancer cells to metastasise.14 In addition, loss of intercellular communication correlates with high metastatic potential of mammary adenocarcinoma cells.15 In addition, there is a growing body of evidence that connexins may be involved in intravasation and extravasation of cancerous cells.3,4,5 Moreover, connexin expression (especially of Cx26) was found in lymph node metastases of squamous cell carcinoma,16 while cancerous cells at invasive sites showed reduction in connexin expression. Nevertheless, it is still unclear whether and how connexins could participate in the metastatic process of breast cancer, especially to the lymph nodes. Consequently, the aim of this study was to compare expression of Cx26 and Cx43 in primary tumours (PT) of breast cancer and matched lymph node metastases.
METHODS
This study comprised 71 women treated surgically with partial or total mastectomy and lymph node dissection for primary breast cancer. Mean age of patients was 54.6 years (range 30– 80). Patients had not received any preoperative chemotherapy or hormone therapy. Tumour samples, adjacent normal tissue, and lymph nodes were collected immediately after surgical removal of tumour, fixed in 10% buffered formaldehyde solution for 48 hours, and then embedded in paraffin blocks at 56°C according to standard procedures. Tumour samples were cut into 5 μm thick sections and stained with haematoxylin and eosin.
For immunohistochemical studies of Cx26 and Cx43, we selected 51 matched pairs of PT and their metastases to lymph nodes. Connexins were investigated using polyclonal goat Cx26 antibody (1:300 dilution; Santa Cruz Biotechnology, Santa Cruz, USA) and polyclonal goat Cx43 antibody (1:200 dilution; Santa Cruz Biotechnology). All primary antibodies were diluted in phosphate buffered saline with 1.5% normal blocking serum. We applied the streptavidin biotin peroxidase complex technique to visualise the complexes of connexins and their specific antibodies (LSAB kit; Dako, Glostrup, Denmark). The immunohistochemical method has been described previously.17 Slides were counterstained with haematoxylin. Two independent pathologists (MS, SS) scored the intensity of developed immunoreactivity of connexins under light microscopy (Olympus BX40). In negative controls, the primary specific antibodies were omitted for the immunohistochemical staining. Expression of Cx26 and Cx43 was analysed in 10 different tumour fields and the presence of both connexins was assessed according to a 3 point scale (0 = <10% positive cells; 1+ = 10–50% positive cells; 2+ = >50% positive cells). The specimens were then divided into connexin positive (levels 1+ or 2+) and connexin negative (level 0) tumours based on this grading.
Statistical analysis
The significance of the associations between Cx26 and Cx43 were determined using Spearman's correlation analysis. Differences in Cx26 and Cx43 expression between PT and lymph node metastases were assessed using the Mann‐Whitney U and Wilcoxon rank sum W tests. Probabilities of p<0.05 were considered statistically significant.
RESULTS
Expression of Cx26 and Cx43 in primary tumours
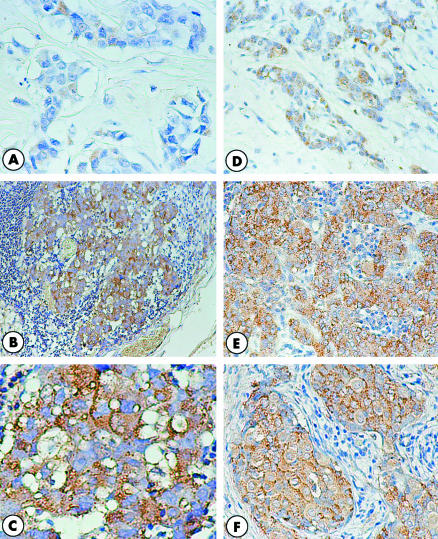
In PT, 27 of 51 cancers (53%) were positive for Cx26. Only cytoplasmic expression of this protein was seen (fig 1A). Immunoreactivity to Cx43 was observed in 42 of 51 of the evaluated tumours (82.4%). Cx43 expression in PTs was predominantly cytoplasmic, although a mixed (cytoplasmic and membranous) staining in a few cases was seen too (fig 1D). We found a statistically significant positive correlation between Cx26 and Cx43 in PTs (p<0.0001, r = 0.522).
Figure 1 (A–C) Cx26 expression in primary tumour of breast cancer and matched paired metastasis to the lymph node. (A) Individual tumour cells show a weak cytoplasmic staining pattern. This case was Cx26 negative. (B, C) In the lymph node, metastatic cells demonstrate strong granular immunostaining in the majority of cells, and a focally membranous localisation of Cx26 deposits is present. (D–F) Immunohistochemical detection of Cx43 in breast cancer primary tumour and matched lymph node metastasis. (D) About half of all tumour cells expressed Cx43 in the cytoplasmic compartment. (E–F) All metastatic cells show strong cytoplasmic and membranous staining pattern for Cx43. Original magnification: (A, B, D, E) ×200; (C, F) ×400.
Expression of Cx26 and Cx43 in lymph node metastases
In total, 45 of 51 cases (88.2%) of lymph node metastases (MLNs) were Cx26 positive. Similarly to PTs, a dominance of cytoplasmic staining was observed, although in some MLNs, a mixed (cytoplasmic and membranous) immunostaining pattern (fig 1B,C) was found. Positive Cx43 expression was present in 49 of 51 MLNs (96.1%). A cytoplasmic immunostaining pattern was predominant in MLNs; however, the number of cases with mixed expression of Cx43 was increased in comparison with PTs (fig 1E,F). Similarly to PTs, we also noted positive correlation between Cx26 and Cx43 expression in MLNs (p<0.0001, r = 0.554).
Comparison of Cx26 and Cx43 expression between primary tumours and matched lymph node metastases
To assess whether the expression of Cx26 and Cx43 undergoes changes during breast cancer progression, we studied 51 matched pairs of PT and their metastases to lymph nodes (tables 1). In 19/51 (37.3%) of the pairs, we observed the same intensity of immunoreactivity for Cx26 in PT and metastases to lymph nodes (table 1). Increased expression of Cx26 in metastases relative to primary tumour was observed in 29 of 51 cases (56.9%). It is important to note that 19 of 24 Cx26 negative PT (79.2%) developed Cx26 positive metastases to regional lymph nodes, but only 1 of 27 Cx26 positive PT led to Cx26 negative metastasis (table 1). In statistical analysis of matched pairs (Mann‐Whitney and Wilcoxon tests), we found that Cx26 expression was significantly increased in lymph node metastases compared with PT (p<0.00001).
Table 1 Comparison of Cx26 and Cx23 expression between the primary breast cancers and matching lymph node metastases.
| Expression level | Cx26 expression in metastatic regional lymph nodes | Cx43 expression in metastatic regional lymph nodes | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Negative (n = 6) | Positive (1+) (n = 180 | Positive (2+) (n = 27) | Total (%) (n = 51) | Negative (n = 2) | Positive (1+) (n = 14) | Positive (2+) (n = 35) | Total (%) (n = 51) | |||||||||
| Expression in PT | ||||||||||||||||
| Negative (n = 24) | 5 (9.8%) | 8 (15.7%) | 11 (21.5%) | 24 (47%) | 2 (3.9%) | 2 (3.9%) | 5 (9.8%) | 9 (17.6%) | ||||||||
| Positive (1+) (n = 19) | 1 (2%) | 8 (15.7%) | 10 (19.6%) | 19 (37.3%) | 0 (0%) | 6 (11.8%) | 11 (21.5%) | 17 (33.3%) | ||||||||
| Positive (2+) (n = 8) | 0 (0%) | 2 (3.9%) | 6 (11.8%) | 8 (15.7%) | 0 (0%) | 6 (11.8%) | 19 (37.3%) | 25 (49.1%) | ||||||||
| Total (%) (n = 51) | 6 (11.8%) | 18 (35.3%) | 27 (52.9%) | 51 (100%) | 2 (3.9%) | 14 (27.5%) | 35 (68.6%) | 51 (100%) | ||||||||
In parallel, we examined the status of Cx43 in 51 matched paired cases of PT and lymph node metastases (table 1). Cx43 expression was unchanged in 27 of 51 pairs (52.9%). In 18 of 51 cases, (35.3%) we noted increased expression of Cx43 in metastases compared with PT. None of Cx43 positive PT had Cx43 negative metastasis, while in seven of nine cases (77.8%), we observed Cx43 positive metastases despite Cx43 negative PT (table 1). There was a significant increase (p<0.001) in Cx43 expression for lymph node metastases compared with PT.
DISCUSSION
Metastasis of breast cancer is a complex process that involves multiple mechanisms, but the factors promoting metastasis are still not well known. It was suggested that loss of gap junction expression and disturbance of GJIC would be important events in invasion and metastasis.3,15,18 However, the role of connexins in metastagenicity remains controversial, because it is still unclear whether connexin expression is required for metastasising.19
In the present study, we found mostly cytoplasmic microgranular staining of Cx26 and Cx43. The normal punctate membranous staining was sporadically seen, but only for Cx43. Cytoplasmic expression of connexins may be an indirect evidence of lack of functional gap junction channels between cancerous cells, as suggested in previous findings,12,20 and our recent reports.21,22,23 Loss of GJIC might facilitate the local invasion of PT, because the reduction of cell to cell communication could contribute to cellular dissociation.16 If connexins do not assemble to create functional gap junction channels, they might cause alteration in expression of different genes in cooperation with other proteins,24,25,26 or they may function as adhesion proteins to form adhesive plaques that could severely impair signalling pathways.27
This study demonstrates for the first time that expression of both Cx26 and Cx43 increase in lymph node metastases of breast cancer compared with PT. Furthermore, the enhanced membranous immunostaining pattern of Cx43 was found in metastases to lymph nodes, while membranous Cx26 expression appeared only in metastatic breast cancer cells. Additionally, Cx26 and Cx43 negative PTs (83.3% and 77.8%, respectively) developed Cx26 and Cx43 positive MLNs.
Our results are in accordance with those of Kamibayashi et al,16 who immunohistochemically analysed the expression of Cx26 and Cx43 in different stages of mouse skin carcinogenesis. They discovered that, even though expression of studied connexins was reduced in early stages of mouse skin carcinogenesis and early invasion, Cx26 and, to a lesser extent, Cx43, was expressed on the plasma membrane of cells that metastasised into lymph nodes. It was thought that connexins may play an important role in the extravasation of cancerous cells into lymphoid tissues by formation of gap junctions between tumour cells and endothelial cells in lymph node vessels.16 The other probable interpretation of our results, which was also suggested by other authors, is that expression of connexins in lymph node metastases may reflect a higher degree of differentiation of metastatic tumour cells compared with cancer cells in the primary tumour.16,28 Our observations of connexin positive metastases derived from connexin negative tumours suggest that tumour cells must possess particular properties in order to acquire the capability to metastasise. It is quite possible that metastatic potential is only possessed by connexin positive clones of cancerous cells. In our opinion, the most important questions are why metastatic breast cancer cells need connexin proteins, and how connexins could participate in the complex process of metastasis. The partial answer to these questions may be provided by the studies of Kamibayashi et al16 and Ito et al,5 which evaluated GJIC between melanoma and endothelial cells. These authors showed that connexins may be involved in the process of intravasation around the PT.5 They observed that melanoma BL6 cells could form heterologous gap junctions with endothelial cells, but not between other BL6 cells. Therefore, such findings might suggest that formation of heterologous gap junctions between melanoma cells and endothelial cells might be responsible for emerging of metastases. Similar observations were made in a previous report by el‐Sabban and Pauli,3 in which they found that highly metastatic cells (B16‐F10 murine melanoma and R3230AC‐MET rat mammary adenocarcinoma cells) communicated with vascular endothelial cells via gap junctions, and that this interaction may play a critical role in tumour cell extravasation at secondary sites. Furthermore, Kapoor et al showed that breast cancer cells are capable of forming functional heterotypic gap junctions with osteoblastic cells (hFOB 1.19). However, the degree of heterotypic GJIC between breast cancer cell lines and osteoblastic cells did not correlate with metastatic potential.29 An additional observation was that an increase in heterotypic GJIC relative to homologous GJIC correlated with the metastatic potential of breast cancer cells. Kapoor et al suggested that heterotypic GJIC between breast cancer cells and other cells may characterise cells capable of metastasising from those incapable. In addition, it has been shown that Cx43 protein, by creation of functional heterocellular coupling between breast cancer cells and endothelial cells, enhances transendothelial migration (diapedesis) of cancerous cells.30
Donahue et al proposed a potential mechanism by which increased heterotypic GJIC could contribute to metastasis.31 Based on the results of studies made by Lewalle et al,32 they suggest that GJIC facilitates paracellular (transendothelial) migration of tumour cells, and pointed at a retraction of the cell layer through increasing cytosolic Ca2+ concentration in endothelial cells, which could be a mechanism by which tumour cells could migrate by endothelium. Consequently, it is possible that cell to cell contact elevates cytosolic Ca2+ in endothelial cells via GJIC.
Although some authors found that loss of gap junctions correlated with metastatic capability of cancerous cells,15,33,34 these and our results do not exclude the role of gap junctions in metastasis, because they analysed functional gap junctions between tumour cells. Lack of functional intercellular connections is also suggested in our evaluations, which may indirectly reflect a dominant, aberrant cytoplasmic accumulation of connexins in PT. The protein components of gap channels are probably stored in this compartment, because of their decreased uptake by cell membrane due to completely abolished or reduced construction of gap junctions.
It has been well documented that formation of functional gap junction channels also requires cell to cell adhesion.8 Cadherins are involved in GJIC and it is possible that one of the reasons for decreased membranous connexin expression is dysfunction of these proteins. E‐cadherin, which is present in epithelial cells, has been recognised as an important suppressor gene.35 Catenins are proteins that form cadherin catenin complexes mediating cell to cell adhesion. There is accumulating evidence that during carcinogenesis, loss or downregulation of cadherins and catenins is present, and dysfunction of these complexes correlates with invasion and metastasis.36,37 However, expression of both E‐cadherin and catenins is not always parallel in PT and lymph node metastasis. For instance, Byrne et al observed a tendency to a higher frequency of E‐cadherin positive cells in lymph node metastases compared with PT of bladder transitional cell carcinoma.38 Increased levels of E‐cadherin expression in metastases derived from E‐cadherin‐positive PT of gastric cancer was present in immunohistochemical studies from Mayer et al.39 Furthermore, Bukholm et al,40 studying immunohistochemically the expression of E‐cadherin, and α‐, β‐, and γ‐catenins in both PT and metastatic lesions of breast cancer, demonstrated re‐expression of E‐cadherin, and α‐, and β‐catenins in metastatic tissues. They suggested that re‐expression of adhesion molecules by cancerous cells after release from primary sites may be necessary for tumour cells to adhere to remote organs. These studies also lend support to a theory that there is more heterogeneity in the PT than in the metastases, as we have suggested above.
Taking into account this study and recent findings, we suggest that functional gap junction channels are formed at a particular time during the metastastic process, for example during transendothelial migration of tumour cells. Consequently, cancerous cells, which have the ability to produce connexin proteins, may then have a strong chance of creating metastases. This theory may partly explain our findings of increased connexin expression in lymph node breast cancer metastasis compared with PT. Additionally, enhancement of connexin expression in metastatic sites may be a symptom of cell differentiation. In summary, these findings imply that Cx26 and Cx43 should be recognised as potential factors that could determine the invasive phenotype of human breast cancer. These types of connexin could maintain indispensable intercellular contacts that are necessary for malignant cells to break tissue barriers and spread in the lymphatic vasculature.
TAKE HOME MESSAGES
It has been suggested that loss of gap junction expression and disturbance of gap junctional intercellular communication (GJIC) may be important events in invasion and metastasis, but the role of connexins in metastagenicity remains controversial.
There was predominantly cytoplasmic localisation of evaluated connexins in primary tumours, and metastases to lymph nodes (MLNs) had higher expression of Cx26 and Cx43 than did primary tumours.
Cx26 and Cx43 negative primary tumours developed Cx26 and Cx43 positive MLNs, and membranous Cx26 expression was only found in metastatic breast cancer cells.
Connexins may contribute to the efficient metastasising of breast cancer to the lymph nodes.
Abbreviations
Cx26 - connexin 26
Cx43 - connexin 43
GJIC - gap junctional intercellular communication
PT - primary breast tumour
MLN - metastasis to lymph node
References
- 1.Aasen T, Hodgins M B, Edward M.et al The relationship between connexins, gap junctions, tissue architecture and tumour invasion, as studied in a novel in vitro model of HPV‐16‐associated cervical cancer progression. Oncogene 2003227969–7980. [DOI] [PubMed] [Google Scholar]
- 2.Lin J H, Takano T, Cotrina M L.et al Connexin 43 enhances the adhesivity and mediates the invasion of malignant glioma cells. J Neurosci 2002224302–4311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.el‐Sabban M E, Pauli B U. Cytoplasmic dye transfer between metastatic tumor cells and vascular endothelium J Cell Biol19911151375–1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.el‐Sabban M E, Pauli B U. Adhesion‐mediated gap junctional communication between lung‐metastatatic cancer cells and endothelium. Invasion Metastasis 199414164–176. [PubMed] [Google Scholar]
- 5.Ito A, Katoh F, Kataoka T R.et al A role for heterologous gap junctions between melanoma and endothelial cells in metastasis J Clin Invest 20001051189–1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Willecke K, Eiberger J, Degen J.et al Structural and functional diversity of connexin genes in the mouse and human genome. Biol Chem 2002383725–737. [DOI] [PubMed] [Google Scholar]
- 7.Monaghan P, Clarke C, Perusinghe N P.et al Gap junction distribution and connexin expression in human breast. Exp Cell Res 199622329–38. [DOI] [PubMed] [Google Scholar]
- 8.Trosko J E, Ruch R J. Cell‐cell communication in carcinogenesis. Front Biosci 19983208–236. [DOI] [PubMed] [Google Scholar]
- 9.Umhauer S, Ruch R J, Fanning J. Gap junctional intercellular communication and connexin 43 expression in ovarian carcinoma. Am J Obstet Gynecol 2000182999–1000. [DOI] [PubMed] [Google Scholar]
- 10.Ruch R J, Porter S, Koffler L D.et al Defective gap junctional intercellular communication in lung cancer: loss of an important mediator of tissue homeostasis and phenotypic regulation Exp Lung Res 200127231–243. [DOI] [PubMed] [Google Scholar]
- 11.Gee J, Tanaka M, Grossman H B. Connexin 26 is abnormally expressed in bladder cancer. J Urol 20031691135–1137. [DOI] [PubMed] [Google Scholar]
- 12.Krutovskikh V, Mazzoleni G, Mironov N.et al Altered homologous and heterologous gap‐junctional intercellular communication in primary human liver tumors associated with aberrant protein localization but not gene mutation of connexin 32. Int J Cancer 19945687–94. [DOI] [PubMed] [Google Scholar]
- 13.Defamie N, Mograbi B, Roger C.et al Disruption of gap junctional intercellular communication by lindane is associated with aberrant localization of connexin43 and zonula occludens‐1 in 42GPA9 Sertoli cells. Carcinogenesis 2001221537–1542. [DOI] [PubMed] [Google Scholar]
- 14.Navolotski A, Rumjnzev A, Lu H.et al Migration and gap junctional intercellular communication determine the metastatic phenotype of human tumor cell lines. Cancer Lett 1997118181–187. [DOI] [PubMed] [Google Scholar]
- 15.Nicolson G L, Dulski K M, Trosko J E. Loss of intercellular junctional communication correlates with metastatic potential in mammary adenocarcinoma cells. Proc Natl Acad Sci USA 198885473–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kamibayashi Y, Oyamada Y, Mori M.et al Aberrant expression of gap junction proteins (connexins) is associated with tumor progression during multistage mouse skin carcinogenesis in vivo. Carcinogenesis 1995161287–1297. [DOI] [PubMed] [Google Scholar]
- 17.Kanczuga‐Koda L, Sulkowski S, Koda M.et al Expression of connexins 26, 32 and 43 in the human colon–an immunohistochemical study. Folia Histochem Cytobiol 200442203–207. [PubMed] [Google Scholar]
- 18.Brauner T, Schmid A, Hulser D F. Tumor cell invasion and gap junctional communication. I. Normal and malignant cells confronted in monolayer cultures. Invasion Metastasis 19901018–30. [PubMed] [Google Scholar]
- 19.Carystinos G D, Bier A, Batist G. The role of connexin‐mediated cell‐cell communication in breast cancer metastasis. J Mammary Gland Biol Neoplasia 20016431–440. [DOI] [PubMed] [Google Scholar]
- 20.Krutovskikh V A, Troyanovsky S M, Piccoli C.et al Differential effect of subcellular localization of communication impairing gap junction protein connexin43 on tumor cell growth in vivo. Oncogene 200019505–513. [DOI] [PubMed] [Google Scholar]
- 21.Kanczuga‐Koda L, Sulkowska M, Koda M.et al Expression of connexin 43 in breast cancer in comparison with mammary dysplasia and the normal mammary gland. Folia Morphol 200362439–442. [PubMed] [Google Scholar]
- 22.Kanczuga‐Koda L, Sulkowski S, Tomaszewski J.et al Connexin26 and 43 correlate with Bak, but not with bcl‐2 protein in breast cancer. Oncol Rep 200514325–329. [PubMed] [Google Scholar]
- 23.Kanczuga‐Koda L, Sulkowski S, Koda M.et al Alterations in connexin26 expression during colorectal carcinogenesis. Oncology 200568217–222. [DOI] [PubMed] [Google Scholar]
- 24.Chen S C, Pelletier D B, Ao P.et al Connexin43 reverses the phenotype of transformed cells and alters their expression of cyclin/cyclin‐dependent kinases. Cell Growth Differ 19956681–690. [PubMed] [Google Scholar]
- 25.Lecanda F, Towler D A, Ziambaras K.et al Gap junctional communication modulates gene expression in osteoblastic cells. Mol Biol Cell 199892249–2258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kanczuga‐Koda L, Sulkowski S, Koda M.et al Connexin 26 correlates with Bcl‐xL and Bax proteins expression in colorectal cancer. World J Gastroenterol 2005111544–1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lin J H, Takano T, Cotrina M L.et al Connexin 43 enhances the adhesivity and mediates the invasion of malignant glioma cells. J Neurosci 2002224302–4311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mareel M, Leroy A. Clinical, cellular, and molecular aspects of cancer invasion. Physiol Rev 200383337–376. [DOI] [PubMed] [Google Scholar]
- 29.Kapoor P, Saunders M M, Li Z.et al Breast cancer metastatic potential: correlation with increased heterotypic gap junctional intercellular communication between breast cancer cells and osteoblastic cells. Int J Cancer 2004111693–697. [DOI] [PubMed] [Google Scholar]
- 30.Pollmann M, Shao Q, Laird D W.et al Connexin 43 mediated gap junctional communication enhances breast tumor cell diapedesis in culture. Breast Cancer Res 20057522–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Donahue H J, Saunders M M, Li Z.et al A potential role for gap junctions in breast cancer metastasis to bone. J Musculoskelet Neuronal Interact 20033156–161. [PubMed] [Google Scholar]
- 32.Lewalle J M, Cataldo D, Bajou K.et al Endothelial cell intracellular Ca2+ concentration is increased upon breast tumor cell contact and mediates tumor cell transendothelial migration. Clin Exp Metastasis 19981621–29. [DOI] [PubMed] [Google Scholar]
- 33.Hamada J, Takeichi N, Ren J.et al Junctional communication of highly and weakly metastatic variant clones from a rat mammary carcinoma in primary and metastatic sites. Invasion Metastasis 199111149–157. [PubMed] [Google Scholar]
- 34.Ren J, Hamada J, Takeichi N.et al Ultrastructural differences in junctional intercellular communication between highly and weakly metastatic clones derived from rat mammary carcinoma. Cancer Res 199050358–362. [PubMed] [Google Scholar]
- 35.Hirohashi S. Inactivation of the E‐cadherin‐mediated cell adhesion system in human cancers. Am J Pathol 1998153333–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Berx G, Van Roy F. The E‐cadherin/catenin complex: an important gatekeeper in breast cancer tumorigenesis and malignant progression. Breast Cancer Res 20013289–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bremnes R M, Veve R, Hirsch F R.et al The E‐cadherin cell‐cell adhesion complex and lung cancer invasion, metastasis, and prognosis. Lung Cancer 200236115–124. [DOI] [PubMed] [Google Scholar]
- 38.Byrne R R, Shariat S F, Brown R.et al E‐cadherin immunostaining of bladder transitional cell carcinoma, carcinoma in situ and lymph node metastases with long‐term follow up. J Urol 20011651473–1479. [PubMed] [Google Scholar]
- 39.Mayer B, Johnson J P, Leitl F.et al E‐cadherin expression in primary and metastatic gastric cancer: down‐regulation correlates with cellular dedifferentiation and glandular disintegration. Cancer Res 1993531690–1695. [PubMed] [Google Scholar]
- 40.Bukholm I K, Nesland J M, Borresen‐Dale A L. Re‐expression of E‐cadherin, alpha‐catenin and beta‐catenin, but not of gamma‐catenin, in metastatic tissue from breast cancer patients. J Pathol 200019015–19. [DOI] [PubMed] [Google Scholar]