Apocrine glands are most frequent in the axillae, groin, external auditory canal, eyelids and on the nipple. Apocrine hidrocystomas are benign adenomatous cystic proliferations derived from apocrine sweat glands, often occuring as solitary translucent cystic lesions, most commonly on the head and neck, especially in periocular tissues (on both the upper and lower eyelids). They have also been reported to occur on the ears, scalp, chest and shoulders. Rarely, they occur on the penis, the vulva, in the axillae and in the anal region. Histologically, the epithelium in apocrine hidrocystoma is lined by a row of columnar secretory cells with apocrine characteristics. Peripheral to this is a layer of myoepithelial cells.1,2
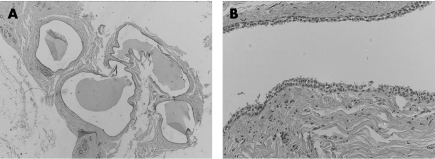
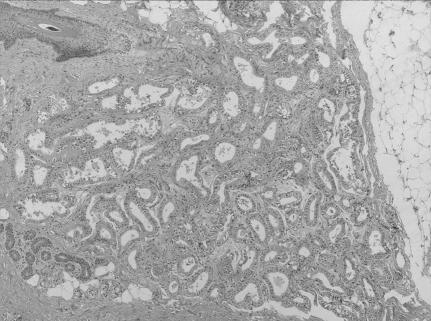
We report a case of bilateral multiple axillary apocrine hidrocystomas associated with apocrine gland hyperplasia of both axillae. The patient is a 39‐year‐old woman, who presented with longstanding fullness and discomfort in both axillae. Clinical examination and mammography were strongly suggestive of accessory breast tissue. The two masses were resected and sent for histopathological examination. Microscopic examination of both axillae showed multiple apocrine hidrocystomas (fig 1) located adjacent to multiple areas of hyperplastic apocrine glands (fig 2). No cellular atypia or increased mitotic activity was seen. The lesion was mainly in the dermis and extended to the subcutaneous tissue. No ductal or lobular breast tissue was identified.
Figure 1 (A) Low‐power view showing multiple cystic areas of apocrine hidrocystoma. Haematoxylin and eosin stain; original magnification ×25. (B) High‐power view of the lining of apocrine hidrocystoma. The decapitation secretion is prominent. Haematoxylin and eosin stain; original magnification ×400.
Figure 2 Apocrine gland hyperplasia. Haematoxylin and eosin stain; original magnification ×25.
Apocrine hidrocystomas are often regarded as adenomas, because the secretory cells are not flattened and they have papillary projections extending into the lumen.1 Multiple apocrine hidrocystomas seem to be uncommon, and axillary lesions are even less common. Of 167 cases studied by Anzai et al,2 the tumour was found in only 15 (9.0%) cases in apocrine gland‐bearing regions, such as the axillae and groin. Only 7 (4.3%) cases have been found in the axillae.
A recent article in this journal3 reported a case of axillary apocrine carcinoma in an elderly man with apocrine hyperplasia in both axillae. Only five cases of axillary apocrine carcinoma with benign apocrine tumours are reported in the literature.3,4,5,6,7 All these cases were of elderly Japanese men who had bilateral benign apocrine tumours. The Japanese authors suggested that apocrine hyperplasia is a precursor of cancer and that apocrine adenoma, hyperplasia and carcinoma may be successive steps in the linear progression to carcinoma.3
The presence of multiple apocrine hidrocystoma may be a marker of two rare inherited disorders: the Schopf–Schulz–Passarge syndrome and the Goltz–Gorlin syndrome.8 The Schopf–Schulz–Passarge syndrome is a rare autosomal recessive form of ectodermal dysplasia characterised by hypodontia, hypoplastic nails, hypotrichosis, palmoplantar keratoderma, cysts of the eyelid margins and multiple periocular apocrine hidrocystomas.8 The Goltz–Gorlin syndrome is sporadic in nature in most cases, but it is assumed to have an X‐linked dominance mode of inheritance, as it occurs more commonly in women. The disorder, also called focal dermal hypoplasia, is characterised by its broad spectrum of meso‐ectodermal defects associated with the skin as well as with the eyes, skeletal system and teeth. Reported cutaneous associations include linear or reticulated atrophic hypopigmented or hyperpigmented skin lesions, papillomas, lipomatous nodules and periocular multiple hidrocystomas.9
Our patient did not have any features suggestive of either disorder.
To our knowledge, our report is the first one describing the association between multiple apocrine hidrocystomas and apocrine hyperplasia occurring in both axillae. No link has been reported so far between apocrine hidrocystomas and apocrine gland carcinomas in the axillae.
Footnotes
Competing interests: None declared.
Informed consent was obtained for publication of the patient's details in this report.
References
- 1.Klein W, Chan E, Seykora J T. Tumors of the epidermal appendages. In: Elder DE, ed. Lever's histopathology of the skin. 9th edn. Philadelphia, PA: Lippincott Williams & Wilkins, 2005892–893.
- 2.Anzai S, Goto M, Fujiwara S.et al Apocrine hidrocystoma: a case report and analysis of 167 Japanese cases. Int J Dermatol 200544702–703. [DOI] [PubMed] [Google Scholar]
- 3.Miyamoto T, Hagari Y, Inoue S.et al Axillary apocrine carcinoma with benign apocrine tumours: a case report involving a pathological and immunohistochemical study and review of the literature. J Clin Pathol 200558757–761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nishikawa Y, Tokusashi Y, Saito Y.et al A case of apocrine adenocarcinoma associated with hamartomatous apocrine gland hyperplasia of both axillae. Am J Surg Pathol 199418832–836. [DOI] [PubMed] [Google Scholar]
- 5.Yoshida A, Kodama Y, Hatanaka S.et al Apocrine adenocarcinoma of the bilateral axillae. Acta Pathol Jpn 199141927–932. [DOI] [PubMed] [Google Scholar]
- 6.Isei T, Yasuda H, Haradaet A.et al A case of axillary apocrine adenocarcinoma arising from apocrine adenoma. Skin Cancer 199510156–159. [Google Scholar]
- 7.Amo Y, Kawano N. A case of ductal apocrine carcinoma in the left axilla with tubular apocrine adenoma in the right axilla. J Dermatol 20033072–75. [PubMed] [Google Scholar]
- 8.Hampton P J, Angus B, Carmichael A J. A case of Schopf‐Schulz‐Passarge syndrome. Clin Exp Dermatol 200530528–530. [DOI] [PubMed] [Google Scholar]
- 9.Sacoor M F, Motswaledi M H. Three cases of focal dermal hypoplasia (Goltz syndrome). Clin Exp Dermatol 20053035–37. [DOI] [PubMed] [Google Scholar]