Abstract
The diagnosis of thymic epithelial neoplasm has been a topic of controversy for many years. Reasons for this include the lack of predictive value associated with the morphology of these tumours and the multiplicity of classification schemes and terminologies proposed over the years. Recently, a new classification schema was introduced by the World Health Organization (WHO) in an attempt to standardise nomenclature and facilitate the diagnosis of primary thymic epithelial neoplasms. This schema, although not originally intended as a new histological classification, but rather as a means for translating equivalent terms from the various existing classifications, has represented a major step forward in this direction. However, problems still exist with the WHO schema, particularly with some of the criteria for the various histological subtypes as well as with issues of interobserver reproducibility. For this reason, we favour using a much more simplified approach to the morphological classification of thymic epithelial neoplasms. A personal approach to the morphological diagnosis of thymoma is described, with a brief explanation for the rationale for simplifying the existing diagnostic categories.
The morphological diagnosis of thymoma has traditionally posed difficulties for pathologists because of the great histological variability and intratumoral heterogeneity of these tumours. A cogent and easily reproducible morphological classification for these tumors has therefore been difficult to conceptualise. Many attempts were made in the past to devise a classification based on pure morphology (ie, shape and proportion of the tumour cells), histogenesis and immunophenotype. Most of these approaches have proved cumbersome, difficult to reproduce in clinical practice and, in general, have failed to provide a sensible solution to the problem. Currently, the most widely used approach to the classification of thymic epithelial neoplasms is that proposed by the World Health Organization (WHO).1,2 We will first review the rationale and basis for this approach.
WHO classification of thymoma
The WHO classification of thymic epithelial neoplasms was first introduced in 1999.2 This schema was the result of extensive deliberation by an international panel of experts. The classification used a combination of letters and numbers to designate various common (and some uncommon) morphological appearances of thymoma. There was no anatomical, functional, histogenetic or other type of stated rationales underlying the schema, and the classification was essentially based on the shape of the neoplastic epithelial cells—that is, whether they adopted an oval or spindle shape (thymoma type A), a round or polygonal shape (type B) or a combination of the two (type AB). A fourth category, thymoma type C, was also introduced and defined as a tumour showing overt cytological features of malignancy, independent of the shape of the cells. The tumours in the type C group lacked any similarity to the other groups of thymoma and resembled instead a variety of carcinomas arising in other organs. Type B thymoma was further subclassified into three types (B1, B2 and B3) based on the proportional increase (in relation to the lymphocytes) and emergence of atypia of the neoplastic epithelial cells. A disclaimer was offered in the WHO monograph by the authors to the effect that this schema was not intended to replace any of the existing classifications, but rather to serve as a means for translating the different terms used by the already existing classifications, mainly the traditional classification of Bernatz et al3 and the histogenetic classification of Kirchner and Muller‐Hermelink,4 into a common language. A revised version of the WHO classification was more recently published in 2004,1 which essentially retained the three basic morphotypes introduced in the original proposal (types A, B and AB), and excluded type C, segregating it into a separate category of thymic carcinoma. The updated version also introduced several unusual morphological types of thymoma that could not be easily placed into any of the other existing categories.
WHO type A thymoma is a tumour that is essentially characterised by a neoplastic population of oval to spindle cells devoid of any marked cytological atypia admixed in variable proportions with small (usually few) lymphocytes. This tumour essentially represents the counterpart of “spindle‐cell thymoma” in the traditional classification proposed by Bernatz et al3 from the Mayo Clinic in 1961. Type AB thymoma is defined as a tumour in which foci having features of type A thymoma are admixed with foci showing features of type B thymoma. Type B1 thymoma is defined as a tumour that resembles the normal functional thymus and combines large expanses indistinguishable from the normal thymic cortex with areas resembling the thymic medulla. The neoplastic epithelial cells are scant and composed of oval cells with pale round nuclei and small nucleoli, although it is also stated that in some cells they may be large and occasionally have conspicuous nucleoli. This tumour is regarded as the equivalent of the lymphocyte‐rich thymoma in the traditional classification.3 Type B2 thymoma is defined as a tumour in which the neoplastic thymic epithelial cells are increased in number and appear as scattered plump cells among a heavy population of lymphocytes. The epithelial cells are described as large, polygonal cells, with large vesicular nuclei and central prominent nucleoli. The tumour cells show a tendency to palisade around vessels and fibrous septa. Dilated perivascular spaces are commonly found. These tumours are regarded as the equivalent of mixed lymphoepithelial thymoma in the traditional3 classification. The main difference between types B1 and B2 seems to be the size of the epithelial cells, these being “larger and more numerous”, and with no areas of “medullary” differentiation in type B2 compared with type B1. Type B3 thymoma corresponds to tumours composed predominantly of epithelial cells having a round or polygonal shape and exhibiting negligible or mild atypia. Type C thymoma is defined as a tumour exhibiting clear‐cut cytological atypia and a set of cytoarchitectural features no longer specific to the thymus, but rather analogous to those seen in carcinomas of other organs. They lack immature T lymphocytes; the lymphocytes present are usually mature T lymphocytes or B lymphocytes and are often admixed with plasma cells. Another designation for these tumours is thymic carcinoma. A variety of histological types are recognised, most having their counterpart in identical tumours arising from other organs, including keratinising squamous cell carcinoma, non‐keratinising squamous cell carcinoma, lymphoepithelioma‐like carcinoma, sarcomatoid carcinoma, clear‐cell carcinoma, basaloid carcinoma, mucoepidermoid carcinoma, papillary carcinoma and undifferentiated carcinoma.
Although the WHO classification has been greeted enthusiastically by many investigators,5,6,7,8,9 several shortcomings and problem areas have been noted that limit its application. The main problems associated with this classification seem to centre on issues of poor interobserver reproducibility and the lack of clinical relevance for some of its histological subtypes; these have been discussed elsewhere and is not reviewed in detail here.9,10,11,12 Another major problem with the WHO classification is that it shows considerable overlap in morphological criteria between many of its subtypes, making precise classification difficult and sometimes arbitrary, often necessitating the help of an expert consultant for proper categorisation of the lesions.11,12 Also, as the original schema was devised as a means of “decoding” the terminology used by the other competing and already existing classifications, a clear rationale or common substrate to the schema was lacking. Although the authors of the new rendition of the WHO classification have repeatedly emphasised that their schema is based on the histogenetic principles of the Kirchner and Muller‐Hermelink classification of thymoma (and, indeed, all of the histogenetic categories in that classification are represented in the WHO schema),1 the fact is that the WHO schema has no demonstrable histogenetic basis. Moreover, the existence of any histogenetic correspondence has been disclaimed in both the original and the revised versions of the WHO books.1,2 These, and other problems associated with the use of this classification, in my opinion, limit the value and utility of the WHO schema for clinical practice.
Suster and Moran classification of thymoma
Owing to the various difficulties that we were experiencing with the existing thymoma classifications, in 1999 we presented a novel proposal for the histological classification of thymic epithelial neoplasms.13 This proposal essentially represented a simplified approach to the morphological classification of these tumours that separated thymic epithelial neoplasms into three broad categories based on their degrees of organotypical differentiation. In our proposal, the histological grading of these tumours was based on the premise that, as in other organs, primary thymic epithelial neoplasms form part of a continuous spectrum of lesions that range from well differentiated to moderately differentiated to poorly differentiated neoplasms. Well‐differentiated tumours would correspond to tumours designated by convention as thymoma; poorly differentiated neoplasms are those conventionally designated as thymic carcinomas; and tumours showing intermediate features of differentiation are designated as atypical thymoma (table 1). The determination of the degree of differentiation for any given tumour in this system is established on the presence or absence of the characteristic organotypical features of differentiation of the normal thymus and on the degree of cytological atypia of the proliferating epithelial cells.13,14 Thus, tumours displaying most or all of the organotypical features of thymic differentiation (such as lobulation, dual cell population with a mixture of thymic epithelial cells and immature T lymphocytes, perivascular spaces, areas of so‐called medullary differentiation, and so on) and absence of cytological atypia are classified as well‐differentiated thymic epithelial neoplasms (ie, thymoma); tumours that retain some of the organotypical features of differentiation of the thymus, but which already display mild to moderate cytological atypia are classified as moderately differentiated thymic epithelial neoplasms (ie, atypical thymoma); and tumours characterised by total absence of the organotypical features of the thymus and showing overt cytological evidence of malignancy correspond to poorly differentiated thymic epithelial neoplasms (ie, thymic carcinoma). This classification is simple, easy to reproduce and does not depend on any purported histogenetic considerations or require the use of special stains or other specialised techniques. It can be easily applied on the basis of the examination of routinely stained slides by haematoxylin and eosin, and requires only familiarity with the organotypical features of differentiation for the different stages of maturation of the normal thymus, along with attention to the degree of cytological atypia displayed by the neoplastic epithelial cells.13 Moreover, the division of these tumours based on degrees of differentiation (as is the norm for most other organs) provides a functional substrate for a rational classification of these tumours, as the various organotypical features of differentiation of the thymus closely parallel the functional status of the organ.13
Table 1 Suster and Moran classification of thymic epithelial neoplasms.
| Tumour type | Grading | Histological criteria |
|---|---|---|
| Thymoma | Well differentiated | Preservation of organotypical features of thymic differentiation; no cytological evidence of atypia |
| Atypical thymoma | Moderately differentiated | Partial preservation of organotypical features of differentiation; mild to moderate cytological atypia |
| Thymic carcinoma | Poorly differentiated | Loss of organotypical features of differentiation; presence of overt cytological evidence of malignancy |
Reprinted with permission from Suster and Moran.17
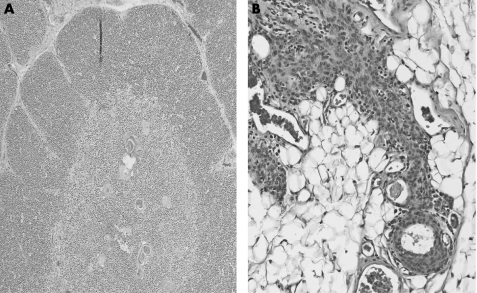
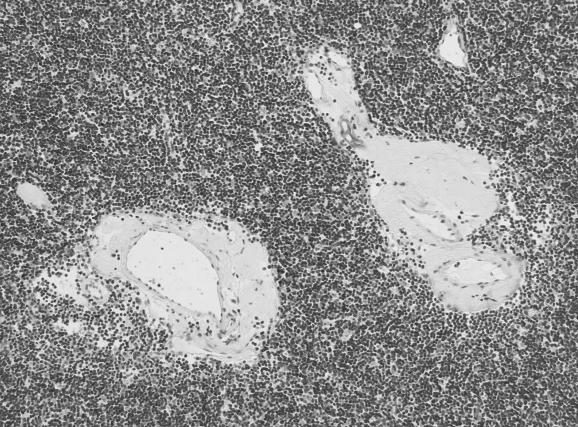
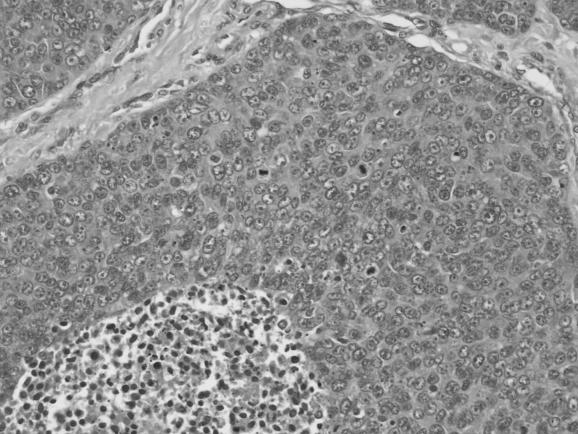
One of the problems for understanding the relationship between organotypical differentiation and the functional status of the organ in the past has been the failure to realise that the thymus is unique among human organs in that its “normal” morphotype can vary considerably depending on the age of the patient and the stage of maturation of the organ.15 Unlike most other organs in the human body, the thymus reaches its functional maturity during childhood and adolescence and undergoes a process of loss of functional activity and progressive involution thereafter. This results in an organ whose “normal” histological appearance can vary widely depending on the age of the patient (fig 1A,B). Recent studies by Hale16 have mapped this process and shown that with loss of functional maturity, the lymphocytic component of the thymus is progressively replaced by fat and, although the thymus retains its normal size and shape even with advancing age, the residual thymic elements become atrophic and reduced to microscopic remnants. The epithelial cell component also undergoes a process of involution and with loss of functional activity, the cells lose their round shape and become smaller, with oval to spindle nuclei and scant cytoplasm.15,16 Well‐differentiated thymic epithelial neoplasms (ie, thymoma) therefore can show a wide spectrum of morphological appearances that can vary depending on whether the neoplastic cells are attempting to recapitulate the normal, mature thymus of infancy and adolescence or whether they resemble the normal involuted thymus of the adult.13,14,15 Most tumours that recapitulate the normal thymus of infants and adolescents are characterised by well‐developed lobules, with a predominance of small immature T lymphocytes and few intermingled neoplastic thymic epithelial cells (fig 2). The lobules are usually separated by fibrous bands of variable thickness that are often angulated. Dilated perivascular spaces are commonly present in these tumours. Focal areas of medullary differentiation characterised by pale foci containing a smaller number of lymphocytes than the surrounding tissue can also be seen. The proportion of small lymphocytes to epithelial cells can vary widely among tumours and within different areas of the same tumour. The epithelial cells are round, with large vesicular nuclei and single small eosinophilic nucleoli, and are surrounded by abundant cytoplasm with indistinct cell borders. The cells usually do not show any marked cytological atypia and are devoid of mitotic activity. Mitoses can often be observed in the more immature lymphoid cell elements. These tumours are the equivalent of the lymphocyte‐rich thymoma and mixed (lymphoepithelial) thymoma of the traditional classification,3 of the cortical and predominantly cortical thymoma of the Kirchner and Muller‐Hermelink classification,4 and of the types B1 and B2 in the WHO schema.1
Figure 1 (A) Normal, mature thymus of childhood. (B) Normal thymus in a 57‐year‐old man. Note the massive involution of the thymus with extensive replacement by fat and thin strands of flattened, atrophic, spindle thymic epithelial cells.
Figure 2 Thymoma showing features that recapitulate the mature, functionally active thymus of childhood and adolescence, with predominance of immature T lymphocytes admixed with scattered large, round thymic epithelial cells.
Tumours recapitulating the features of the normal involuted thymus of the adult are characterised by a solid proliferation of oval to spindle cells, with small elongated nuclei showing a dense chromatin pattern with occasional small, inconspicuous nucleoli and scant rim of cytoplasm (fig 3). The cells often adopt a fascicular growth pattern, but may grow as sheets admixed with variable numbers of small lymphocytes, or they can adopt a variety of unusual growth patterns, such as the creation of rosette‐like structures, storiform pattern, hemangiopericytic pattern, micronodular pattern, trabecular (adenoid) pattern and others.17 The epithelial tumour cells are completely devoid of cytological atypia or mitotic activity. These tumours are usually characterised by a paucity of lymphocytes, although some cases can show a considerable number of T lymphocytes admixed with the epithelial cells. These tumours correspond to the spindle cell type of thymoma in the traditional classification3 and to the medullary type of thymoma in the Kirchner and Muller‐Hermelink classification,4 and are also the equivalent of type A thymoma in the WHO schema.1 Patients showing admixtures of spindle cell areas with round cells and lymphocyte‐rich areas are often encountered and correspond to the mixed category in the Kirchner and Muller‐Hermelink classification4 and to the type AB thymoma in the WHO schema.1
Figure 3 Thymoma showing features that recapitulate the atrophic or involuted, non‐functional thymus of the adult. Sheets of bland‐appearing spindled epithelial cells with occasional small T lymphocytes can be observed.
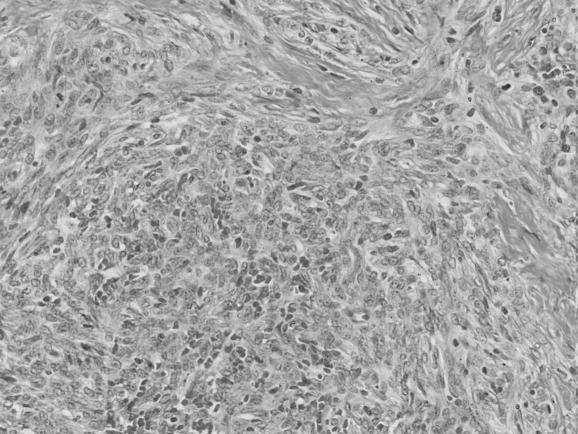
Moderately differentiated thymic epithelial neoplasms (ie, atypical thymomas) are defined as tumours that retain some of the organotypical features of differentiation of the thymus, but already show some degree of cytological atypia in the neoplastic epithelial cells (fig 4). Such tumours are the equivalent of the predominantly epithelial thymomas in the traditional classification,3 of the well‐differentiated thymic carcinoma of the Kirchner and Muller‐Hermelink classification4 and of the type B3 thymoma in the WHO schema.1 The tumours are histologically characterised by sheets of large, round to polygonal epithelial cells with large, irregular and hyperchromatic nuclei showing frequent prominent eosinophilic nucleoli and occasional mitotic figures. The nuclei often have irregular, raisin‐like contours. The cytoplasm of the cells is generally abundant and deeply eosinophilic, with very sharp cell borders often imparting the lesion with a “squamoid” appearance. Foci of early squamous differentiation can be encountered. The cells can sometimes show clear cytoplasm and often show a tendency to palisade around vessels or perivascular spaces. The tumours also show at least some of the organotypical features of the thymus, such as lobulation, prominent dilated perivascular spaces and an admixture of epithelial cells with small lymphocytes. These tumours are more often invasive than other types of thymoma, with a tendency for earlier recurrences. Atypical thymoma can also be composed of spindle to oval cells rather than round or polygonal cells. In such instances, the spindle cells will show increased nuclear size, with prominent nucleoli and occasional mitotic figures.
Figure 4 Atypical thymoma, characterised by partial preservation of the organotypical features of the thymus (perivascular spaces and dual cell population), but showing paucity of lymphocytes and sheets of large polygonal epithelial cells with nuclear atypia and dense chromatin pattern.
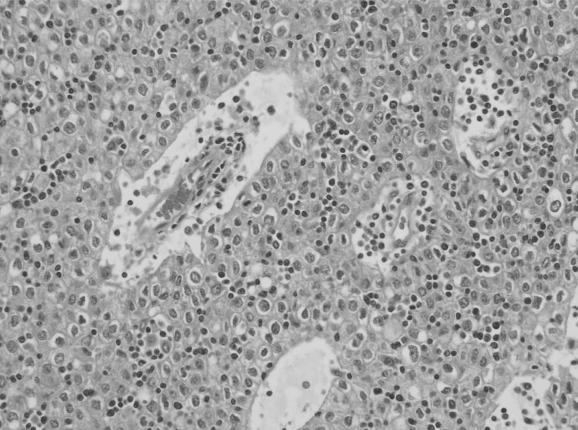
Poorly differentiated thymic epithelial neoplasms (ie, thymic carcinoma) are characterised by loss of the organotypical features of differentiation of the thymus and the presence of marked or overt cytological features of malignancy (fig 5). These tumours are the equivalent of thymoma type C in the original proposal of the WHO classification2 and they essentially resemble carcinomas similar to those arising in other epithelial organs.17 Thymic carcinoma represents a diagnosis of exclusion. Currently, as no reliable specific markers are available that can help us determine the primary nature of these tumours, definitive diagnosis depends on the demonstration of the absence of a primary tumour elsewhere by thorough clinical and imaging studies or at the time of autopsy.18,19 A large variety of histological variants have been described, including keratinising squamous cell carcinoma, non‐keratinising, poorly differentiated (lymphoepithelioma‐like) squamous cell carcinoma, mucoepidermoid carcinoma, clear cell carcinoma, basaloid carcinoma, spindle cell (sarcomatoid) carcinoma, anaplastic carcinoma, neuroendocrine carcinoma and others.17,18,19 The main problem associated with their diagnosis lies in making a determination as to whether they are primary or metastatic.
Figure 5 Thymic carcinoma characterised by absence of the organotypical features of the thymus, with overt cytological evidence of malignancy.
Although our proposal was initially severely criticised, this approach has been recently validated in a large study of thymoma in which it was shown that further simplification of the WHO schema into three subgroups led to classes with good discriminatory power with respect to survival and superior interobserver agreement.20 Thus, by simplifying the WHO classification (ie, merging types A, AB, B1 and B2 into a single group, B3 as a separate group and type C as another group), three subgroups with distinct survival could be identified in that study.20 The authors concluded “our results are in favour of classifications that permit accurate allocation of these neoplasms into simple and reproducible diagnostic categories, as proposed by Suster and Moran”.20 This simplified approach also has the advantage of allowing general pathologists to confidently report thymomas without the need to struggle with often conflicting, confusing or ambiguous histological criteria that define some of the WHO categories11,12 (table 2).
Table 2 Comparison of World Health Organization schema and the Suster and Moran histological classification of thymoma.
| WHO | Suster and Moran |
|---|---|
| Type A | Thymoma |
| Type AB | Thymoma |
| Type B1 | Thymoma |
| Type B2 | Thymoma |
| Type B3 | Atypical thymoma |
WHO, World Health Organization.
My approach to the diagnosis of thymoma
The most important step in the diagnosis of thymoma is, firstly, to make sure that we are indeed dealing with a thymoma. The most common problem brought to my attention in my personal consultation material is the failure by other pathologists to recognise a given tumour as a thymoma, or of mistakenly diagnosing something else as a thymoma. Clinical features that should raise the possibility of thymoma in the differential diagnosis of a mediastinal mass include location of the tumour in the anterior or anterior–superior mediastinal compartment, the description of a well‐circumscribed, lobulated mass surrounded by a fibrous capsule, the absence of malignancy elsewhere on thorough clinical history and clinical examination, and a history of myasthenia gravis or other paraneoplastic syndromes.17 The next step in the diagnosis of thymoma lies in the histological examination of a biopsy sample or resection specimen. The most critical step for histopathological diagnosis rests on identifying the organotypical features of thymic differentiation associated with the different stages of maturation of the normal thymus (table 1). The vast majority of thymomas are well differentiated and organotypical. The morphology of well‐differentiated thymoma, however, can vary considerably depending on whether it is trying to recapitulate the normal thymus of childhood or adolescence or the normal thymus of adults. A multitude of variations on the theme can be seen, with many gradations being possible in the size and shape of the epithelial cells within the same tumour, as well as the relative proportion of thymic epithelial cells to lymphocytes. Unusual morphological variants, including cases showing a micronodular configuration with abundant B cells or plasma cells in the stroma, unusual growth patterns (ie, adenoid, trabecular, hyalinising, hemangiopericytic, rosette forming, and so on) and tumours with variable proportions of thymic epithelial cells in relation to the background lymphocytes can be seen.14 For as long as the proliferating thymic epithelial cells lack evidence of cytological atypia, and some of the organotypical features of thymic differentiation can still be recognised, they should all be regarded as examples of well‐differentiated thymomas. Increase in cytological atypia, such as increase in nuclear size, nucleolar prominence, hyperchromasia and mitotic figures, in a tumour that still retains some of the organotypical features of thymic differentiation define a moderately differentiated neoplasm (atypical thymoma). The shape of the cells in atypical thymoma can be either round–polygonal or oval–spindle. The important feature is the presence of cytological atypia beyond what is normally encountered in normal thymic epithelial cells, whether those of the mature thymus in childhood or adolescence, or of the involuted thymus of the adult. The diagnosis of a poorly differentiated thymic epithelial neoplasm (thymic carcinoma) is made when the cells show overt cytological evidence of malignancy and the tumour no longer shows any organotypical attributes of the normal thymus, but instead resembles a carcinoma arising in other organs. This diagnosis is more often a diagnosis of exclusion and can only be made a priori under exceptional circumstances.
Differential diagnosis
The differential diagnosis for thymoma is quite broad and includes several epithelial and mesenchymal tumours, both primary and metastatic. The most important differential diagnosis for well‐differentiated thymoma with a predominantly lymphocytic component is with lymphoma, in particular lymphoblastic lymphoma. The most important step in the differential diagnosis in this setting is to carry out a cytokeratin stain to identify the scattered thymic epithelial cells, which are singly scattered in the background of the lymphocytic population. Misdiagnosis of thymoma for lymphoma is one of the most common pitfalls encountered in this clinical setting. The spindle cell variant of thymoma can occasionally be confused for a variety of mesenchymal spindle cell tumours, including solitary fibrous tumour and synovial sarcoma, as well as for a neuroendocrine neoplasm when the tumour is predominantly composed of rosette‐like or trabecular structures. The absence of appreciable cytological atypia and identification of some of the organotypical features of thymic differentiation will help separate these tumours from other conditions. Additionally, strong and diffuse positivity for cytokeratin and negative results for other differentiation markers can help arrive at the correct diagnosis. Other immunohistochemical markers that can be of help for the diagnosis of thymoma under certain circumstances include CD1a, CD3, TdT and CD99, all of which mark immature T lymphocytes whose presence is a constant feature (in varying proportions) of well‐differentiated thymic epithelial neoplasms.
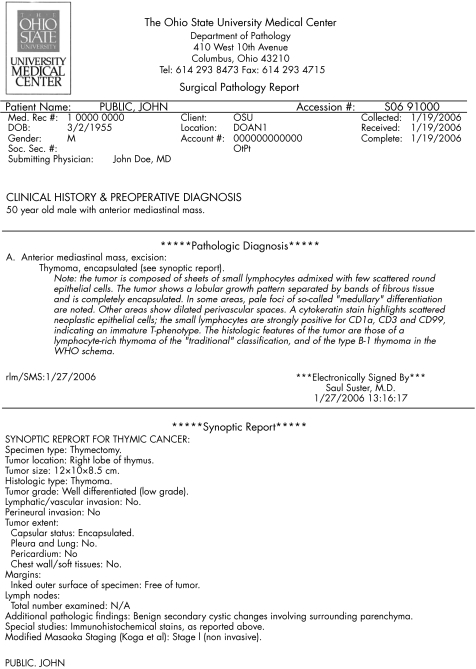
Surgical pathology report
Once a diagnosis of thymoma has been established, the surgical pathology report should include three essential components: the main‐line diagnosis; a comment; and the synoptic report (fig 6). In the line diagnosis, I simply indicate whether the tumour corresponds to a thymoma or an atypical thymoma, followed by whether the tumour is encapsulated or invasive. In the comment section (or note), I usually provide a short description of the morphology and indicate the salient histological features of the tumour, usually accompanied by a categorisation into one of the histological types in the traditional classification (if possible), and with an indication of its equivalence in the current WHO schema (if possible). I mention that in the note if the tumour cannot be fitted into any of the current WHO types or if precise categorisation is not possible. In this section, I also provide the results of any relevant immunohistochemical stains that support my diagnosis or the results of any other ancillary studies carried out (ie, electron microscopy, cytogenetics, flow cytometry and so on).
Figure 6 Example of a surgical pathology report for thymoma (no actual patient). The top half contains the line diagnosis and a supplementary explanatory comment; the bottom half lists the synoptic report.
In recent years, both the College of American Pathologists (CAP) and the Association of Directors of Anatomic and Surgical Pathology in the USA have proposed the use of diagnostic checklists or “templates” that summarise, under a separate heading, all of the relevant information on a case that will be needed by the clinician or oncologist for proper staging of the disease and for the planning of patient management. Thus, the most salient features of the tumour required for clinical staging and management are also listed in the section under synoptic report (fig 6, bottom half). I also recommend becoming familiarised with the protocol for the examination of specimens from patients with thymic epithelial tumours published by the Cancer Committee of the CAP.21 The CAP developed these protocols as an educational tool to assist pathologists in providing clinically useful and relevant information when reporting results of surgical specimen examinations. The type of information necessary for producing a complete and accurate reporting of thymic epithelial neoplasms, including clinical information, macroscopic examination and microscopic evaluation, is detailed in the CAP guidelines.21
Staging of thymoma
Staging of thymoma continues to be a controversial issue. Clinical staging of thymoma was first introduced by Berg et al22 and later modified by Wilkins and Castleman.23 The most popular staging system for thymoma was published in 1981 by Masaoka et al24 and this is the one that has been most widely used in most of the published studies on thymoma. A modification of the Masaoka staging scheme has been more recently introduced by Koga et al,25 in which the four original categories (ie, stages I, II, III and IV) have been retained. However, the authors noted that the survival curves for their tumours between stages I and II as well as for the tumours between stages III and IV did not differ markedly. They therefore concluded that the staging of thymoma could be simplified into two groups: non‐invasive for stages I and II (ie, tumours that are still confined to the anterior mediastinum, without invasion of neighbouring organs) and invasive for stages III and IV (ie, tumours showing invasion of adjacent organs and metastases). I use the non‐invasive and invasive scheme25 in my synoptic report, and also include it implicitly in my line diagnosis, where I always indicate whether the tumour is invasive or non‐invasive. I prefer to designate stage II, however, as “minimally invasive”, to distinguish it from stage III, which is widely invasive, because the two are associated with dramatically different prognoses.25 A somewhat similar, simplified system has been proposed recently by Bedini et al,26 which stages the tumours into three tiers: locally restricted disease, locally advanced disease and systemic disease.
Take‐home messages
A simplified three‐tiered histologic classification (thymoma, atypical thymoma and thymic carcinoma; or low‐, intermediate and high‐grade tumours) is favoured over more complex histologic classifications for the reporting of thymic epithelial neoplasms.
The equivalent type in the current WHO schema is appended in a comment (whenever possible) to facilitate comparison with other classification schemes.
Staging is a more important predictive parameter for prognosis than histology.
The simplified modification of the Masaoka clinical staging scheme proposed by Koga et al is recommended, which categorises these tumours into non‐invasive (confined to the mediastinum) and invasive (with infiltration of adjacent structures).
Use of a synoptic report to summarise the salient clinical information is recommended.
No universally accepted staging scheme for thymic carcinoma exists yet, and these tumours are not included in the latest edition of the Cancer Staging Manual of the American Joint Commission on Cancer.27 In the largest series published on thymic carcinoma, the authors applied the original Masaoka staging scheme for the staging of tumours in their patients.18 Until additional information becomes available or a consensus is developed, it is probably best to use the modified Masaoka staging of thymoma for these tumours in the same way that it is applied for thymomas.
Summary
Although much emphasis in recent years has been placed on the histological classification of thymoma, the bulk of the evidence continues to point to clinical staging as the most important parameter for prognostication, particularly for well‐differentiated thymic epithelial neoplasms.9,10,17 For this reason, I believe the most relevant information for the clinician in the main‐line diagnosis of the pathology report should be whether the tumour is well, moderately or poorly differentiated, and whether the tumour is invasive or non‐invasive. Assigning a tumour to any particular WHO subtype is, in my opinion, of secondary importance, particularly for types A, AB, B1 and B2. All of these tumours essentially represent examples of well‐differentiated neoplasms that retain most of the organotypical features of differentiation of the thymus and are devoid of marked cytological atypia. The status of capsular integrity in such cases will be a more accurate predictor of their biological potential and future behaviour than the histology. The specific WHO subtype in this context, although of academic interest for the pathologist, is of secondary importance to the clinician and may actually contribute to create confusion when provided in the line diagnosis. The simplified approach to the reporting of thymic epithelial neoplasms offered here provides all of the pertinent information for our clinical colleagues, including the WHO subtype (whenever applicable) in the comment section, with minimal chance for error and confusion. Owing to its simplicity and the reduced potential for confusion, this is the format that I favour and use in my clinical practice for the reporting of thymoma.
Abbreviations
CAP - College of American Pathologists
WHO - World Health Organization
Footnotes
Competing interests: None declared.
References
- 1.Travis W D, Brambilla E, Muller‐Hermelink H K.et al Pathology and genetics of tumors of the lung, pleura, thymus and heart. In: World Health Organization classification of tumours. Lyon: IARC Press, 2004
- 2.Rosai J. Histological typing of tumors of the thymus. In: World Health Organization international histological classification of tumors. 2nd edn. Berlin: Springer‐Verlag, 1999
- 3.Bernatz P E, Harrison E G, Claggett O T. Thymoma. A clinicopathologic study. J Thorac Cardiovasc Surg 196142424–444. [PubMed] [Google Scholar]
- 4.Kirschner T, Muller‐Hermelink H K. New approaches to the diagnosis of thymic epithelial tumors. Prog Surg Pathol 198910167–189. [Google Scholar]
- 5.Okumura M, Ohta M, Miyoshi S.et al Oncological significance of WHO histological thymoma classification. A clinical study based on 286 patients. Jpn J Torac Cardiovasc Surg 200250189–194. [DOI] [PubMed] [Google Scholar]
- 6.Kim D J, Yang W I, Choi S S.et al Prognostic and clinical relevance of the World Health Organization schema for the classification of thymic epithelial tumors: a clinicopathologic study of 108 patients and literature review. Chest 2005127755–761. [DOI] [PubMed] [Google Scholar]
- 7.Park M S, Chung K Y, Kim K D.et al Prognosis of thymic tumors according to the new World Health Organization histologic classification. Ann Thorac Surg 200478992–997. [DOI] [PubMed] [Google Scholar]
- 8.Kondo K, Yoshizawa K, Tsuyuguchi M.et al WHO histologic classification is a prognostic indicator in thymoma. Ann Thorac Surg 2004771183–1188. [DOI] [PubMed] [Google Scholar]
- 9.Chalabreysse L, Roy P, Cordier J ‐ F.et al Correlation of the WHO schema for the classification of thymic epithelial neoplasms with prognosis. A retrospective study of 90 tumors. Am J Surg Pathol 2002261605–1611. [DOI] [PubMed] [Google Scholar]
- 10.Rieker R J, Hoegel J, Morresi‐Hauf A.et al Histologic classification of thymic epithelial tumors: comparison of established classification schemes. Int J Cancer 200298900–906. [DOI] [PubMed] [Google Scholar]
- 11.Suster S, Moran C A. Thymoma classification: current status and future trends. Am J Clin Pathol 2006125542–554. [DOI] [PubMed] [Google Scholar]
- 12.Suster S, Moran C A. Problem areas and inconsistencies in the WHO classification of thymoma. Semin Diagn Pathol 200522188–197. [DOI] [PubMed] [Google Scholar]
- 13.Suster S, Moran C A. Thymoma, atypical thymoma and thymic carcinoma. A novel conceptual approach to the classification of neoplasms of thymic epithelium. Am J Clin Pathol 1999111826–833. [DOI] [PubMed] [Google Scholar]
- 14.Suster S, Moran C A. Primary thymic epithelial neoplasms. Spectrum of differentiation and histologic features. Semin Diagn Pathol 1999162–17. [PubMed] [Google Scholar]
- 15.Suster S, Rosai J. The thymus. In: Sternberg SS, ed. Histology for pathologists. 2nd edn. Philadelphia: Raven‐Lippincott, 1997687–706.
- 16.Hale L P. Histologic and molecular assessment of human thymus. Ann Diagn Pathol 2004850–60. [DOI] [PubMed] [Google Scholar]
- 17.Suster S, Moran C A. The mediastinum. In: Weidner N, Cote R, Suster S, Weiss LM, eds. Modern surgical pathology. Philadelphia: WB Saunders, 2003439–504.
- 18.Suster S, Rosai J. Thymic carcinoma. A clinicopathologic study of 60 cases. Cancer 1991672350–2355. [DOI] [PubMed] [Google Scholar]
- 19.Suster S, Moran C A. Thymic carcinoma: spectrum of differentiation and histologic types. Pathology 199830111–122. [DOI] [PubMed] [Google Scholar]
- 20.Rieker R J, Hoegel J, Morresi‐Hauf A.et al Histologic classification of thymic epithelial tumors: comparison of established classification schemes. Int J Cancer 200298900–906. [DOI] [PubMed] [Google Scholar]
- 21.Marchevsky A M, Hammond E H, Moran C A.et al Protocol for the examination of specimens from patients with thymic epithelial tumors located in any area of the mediastinum. Arch Pathol Lab Med 20031271298–1303. [DOI] [PubMed] [Google Scholar]
- 22.Berg N P, Gatzinsky P, Larsson S.et al Tumors of the thymus and thymic region. I. Clinicopathological studies on thymomas. Ann Thorac Surg 19782591–98. [DOI] [PubMed] [Google Scholar]
- 23.Wilkins E W, Castleman B. Thymoma: a continuing survey at the Massachusetts General Hospital. Ann Thorac Surg 197928252–256. [DOI] [PubMed] [Google Scholar]
- 24.Masaoka A, Monden Y, Nakahara K.et al Follow‐up study of thymoma with special reference to their clinical stages. Cancer 1981482485–2492. [DOI] [PubMed] [Google Scholar]
- 25.Koga K, Matsuno Y, Noguchi M.et al A review of 79 thymomas: modification of staging system and reappraisal of conventional division into invasive and non‐invasive thymoma. Pathol Int 199444359–367. [DOI] [PubMed] [Google Scholar]
- 26.Bedini A V, Andreani S M, Tavecchio L.et al Proposal for a novel system for the staging of thymic epithelial tumors. Ann Thorac Surg 2005801994–2000. [DOI] [PubMed] [Google Scholar]
- 27.American Joint Committee on Cancer AJCC cancer staging manual. 6th edn. Berlin: Springer‐Verlag, 2002