Abstract
Aim
To investigate multiple bone cytokines produced by prostate carcinoma (PCa) as a novel strategy to differentiate potential aggressiveness in localised PCa using immunohistochemical analysis.
Methods
A total of 47 cases of PCa undergoing radical prostatectomy or transurethral prostatic resection at our institution (Fundación Jiménez Díaz (Grupo Capio), Madrid, Spain) between January 1991 and June 1998 were identified as low‐grade (⩽4; n = 22) or high‐grade (⩾7, excluding 7 (3+4) cases; n = 25) PCa according to Gleason grade. PCa specimens were immunostained for: parathyroid hormone (PTH)‐related protein (PTHrP), the PTH1 receptor, osteoprotegerin and receptor activator of nuclear factor‐κ B ligand (RANKL), as well as Ki67 (a proliferation marker) and CD34 (an angiogenesis marker).
Results
PCa samples showed an increased immunostaining for both osteoprotegerin and RANKL, associated with tumour grade and PTHrP positivity, in the tumoral epithelium. Using a score value of 4—corresponding to moderate staining—as cut‐off, the best sensitivity value was for PTHrP (with C‐terminal antiserum C6; 100 %); wheras the best specificity value was for RANKL (95 %).
Conclusions
All the evaluated factors are overexpressed mainly in the high‐grade tumours. Our findings indicate that, in most patients with PCa (with Ki67 values between 1% and 9%), sequential determination of C‐terminal PTHrP and RANKL immunoreactivities is a useful approach to discriminate low‐grade and high‐grade tumours.
Prostate carcinoma (PCa) is the most common cancer in men in western societies.1 With increasing age, most men develop microscopic PCa foci, and a small percentage of these become invasive PCa. The invasive PCa is related to the development of bone metastases resulting in increased osteoblastic lesions associated with an increased bone turnover.2 The challenge in PCa today is the identification of stage‐specific tumour markers to differentiate indolent tumours from those agressive malignancies that justify radical treatment. Histological criteria (Gleason grade, number of neoplastic cylinders, tumour volume, ploidia and perineural invasion) are commonly used for stratifying patients with PCa, but progression of PCa is highly variable and cannot be satisfactorily predicted by these criteria alone.3,4 Thus, biochemical parameters, including the apoptosis‐related proteins bax and bcl‐2, cell cycle‐related protein p27, vascular endothelial growth factor and components of the renin–angiotensin system, are currently investigated to predict PCa aggressiveness.5,6,7,8,9,10,11,12
Parathyroid hormone (PTH)‐related protein (PTHrP), the main factor responsible for malignant hypercalcaemia, and its PTH1 receptor (PTH1R) are expressed in a variety of normal and malignant tissues.13,14 Using in situ hybridisation, PTHrP was detected in neuroendocrine cells in the normal prostate.15 Despite the rarity of hypercalcaemia in PCa, PTHrP is often increased in this malignancy, compared with normal prostate or benign prostatic hyperplasia.15,16,17,18,19 Some investigators found a positive association between Gleason grade and PTHrP positivity in PCa; although others failed to find this to be so.16,18 Recent studies indicate that intracrine effects of PTHrP might affect processes such as cell proliferation, apoptosis and angiogenesis in PCa.20,21 PTHrP‐overexpressing PCa cells injected in rodents were found to induce the development of osteolytic metastases.22,23 Moreover, various PCa cell lines derived from skeletal and other metastatic lesions express and show a proliferative response to PTHrP.20 This protein thus seems to have complex actions involved in promoting PCa progression.
Current evidence supports the notion that malignant cells, including PCa cells, co‐opt the physiological mechanisms that increase bone resorption to invade bone.24 Therefore, they release factors (eg, PTHrP) which favour the production of osteoclast activators, notably the receptor activator of nuclear factor‐κB ligand (RANKL), in the bone environment.25 RANKL activity is regulated by osteoprotegerin (OPG), a soluble tumour necrosis factor receptor family member that binds RANKL preventing its interaction with receptor activator of nuclear factor‐κB and thus inhibits bone resorption.25 Both OPG and RANKL are produced by PCa cells, wherein the OPG protein may act as a survival factor.26,27 In addition, the number of PCa cells showing OPG and RANKL immunoreactivities was markedly increased in bone metastases, compared with nonosseous metastases or with the primary tumour.26 Moreover, OPG was also found to be increased in the serum of patients with bone metastases.28 The levels of these proteins might thus influence the interaction of PCa cells with the bone environment.2
We carried out a comprehensive study to examine PTHrP, OPG and RANKL immunoreactivities in PCa specimens. We hypothesised that a significant link occurs between PTHrP, OPG and RANKL and other well characterised factors, namely Ki67 (a marker of proliferation) and CD34 (an angiogenesis marker), to distinguish less and more aggressive PCa tumours.
Materials and methods
Patient samples
This retrospective study included 47 patients (aged 51–82 years) diagnosed with localised PCa, undergoing radical prostatectomy (n = 23) or transurethral prostatic resection (n = 24) between January 1991 and June 1998 at our institution (Fundación Jiménez Díaz (Grupo Capio), Madrid, Spain). Archived paraffin‐embedded primary tissue specimens were divided into two groups, according to low Gleason (⩽4; n = 22) or high Gleason (⩾7, excluding 7 (3+4); n = 25) grade. Sections were examined by a pathologist to confirm the presence of localised malignant tissue and PCa score. None of the patients had any evidence of metastases or had received PCa treatment at the time of sampling. The study was performed in accordance with the ethical standards of the Helsinki Declaration.
Immunohistochemistry
Tissue sections (3‐μm thick) were immunostained using an Envision+ system (Dako, Glostrup, Denmark). Antigen retrieval was performed by either pressure cooker treatment in 10 mM citrate buffer, pH 6 (CD34, PTHrP, PTH1R, OPG and RANKL) or microwave treatment (Ki67). The samples were then incubated for 30 min at room temperature or overnight at 4°C (PTHrP and the PTH1R) with the primary antibodies. PTHrP immunostaining was performed using several rabbit polyclonal antisera with different specificities: antiserum C6, recognising the highly conserved C‐terminal epitope 107–111 in the intact PTHrP molecule;29 antiserum C13, detecting an N‐terminal epitope in intact PTHrP and also the PTHrP (1–36) fragment; and antiserum C7, which mainly recognises the C‐terminal peptide PTHrP (107–139),29,30 each at 1:600 dilution. For the PTH1R receptor staining, we used affinity‐purified polyclonal antibody Ab‐IV (Covance, Berkeley, California, USA), at 1:150 dilution. OPG and RANKL staining was carried out with rabbit polyclonal antibodies, H‐249 (OPG) and FL‐317 (RANKL) (Santa Cruz Biotechnology, Santa Cruz, California, USA), at 1:100 and 1:40 dilution, respectively. Ki67 (clone MIB1) (Dako, Glostrup, Denmark) and CD34 (Novocastra, Newcastle, UK) were immunostained with specific mouse monoclonal antibodies, at 1:100 and 1:30 dilution, respectively. The tissue sections were subsequently incubated with a polymer‐peroxidase complex and 3,3′‐diaminobenzidine, and counterstained with haematoxylin (ChemMate, Dako). Some sections were incubated without the primary antibody or with non‐immune rabbit serum as negative controls. PCa specimens that had previously shown a marked positivity for each antibody were also routinely included in each tissue array as positive controls.
Immunohistological evaluation
Immunostainings were evaluated in five ×200 microscopic fields by a pathologist and another independent observer in a blinded fashion. Ki67 staining was expressed as the number of stained nuclei per total nuclei (%), and CD34 staining was analysed using the following score (number of microvessels per field): 1 (25–50), weak; 2 (51–75), moderate; and 3 (>75), strong. Positivity for PTHrP, PTH1R, OPG and RANKL was assessed according to a scoring system evaluating both the immunostained epithelial area and the staining intensity. The former was graded according to the score (%): 1 (<25), 2 (25–75), and 3 (>75), using an image analysis software (Optimas 6.5; Media Cybernetics, Silver Spring, Washington, USA). Staining intensity was scored from 1 to 3+ (most intense). The product of the two scores determined the final score value as follows: 0, negative; 1–3, weak; 4, moderate; and 6–9, strong.
Statistical analysis
The Mann–Whitney U test was used to compare score values in the neoplastic areas from low‐grade and high‐grade PCa, and Spearman's rho for correlation analysis. A simple Wilcoxon's rank test was performed to compare score values between neoplastic and adjacent non‐tumoral areas. Specificity and sensitivity were calculated using as reference limits: the score values of 1, 2 and 3 for CD34; and those corresponding to quartiles 1 and 3, as well as the score value of 4 (moderate staining) for each bone cytokine studied. Significance was considered at p<0.05.
Results
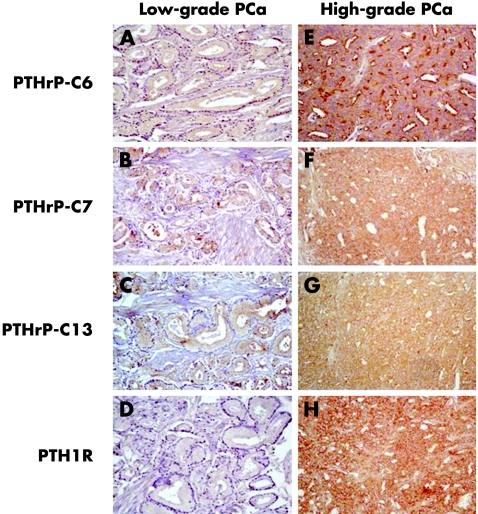
Most samples from high‐grade tumours showed moderate to strong immunoreactivity for Ki67 (⩾5%) and CD34 (⩾2), and for PTHrP, PTH1R, OPG and RANKL (⩾4) in the neoplastic area. Immunostaining for the last four factors mainly localised to the acinar cells, but some staining was observed in the stroma (figs 1, 2). Patchy positivity for the PTH1R and RANKL was evident in epithelial cell membranes from the more intensely stained tumours (figs 1, 2). In contrast, a lower and variable number of low‐grade tumour samples had score values for these factors in this range (table 1).
Figure 1 Evaluation of several factors in low‐grade and high‐grade prostate carcinoma (PCa). Immunostaining for Ki67 (A,E); CD34 (B,F); osteoprotegerin (OPG; C,G); and receptor activator of nuclear factor‐κ B ligand (RANKL; D,H) was performed with specific antibodies. Representative examples of a low‐grade PCa (A‐D) and a high‐grade PCa (E‐H) are shown. Negative controls (without corresponding primary antibody) exhibited no positivity (data not shown). Original amplifications, ×200.
Figure 2 Evaluation of several factors in low‐grade and high‐grade prostate carcinoma (PCa). Immunostaining for parathyroid hormone‐related protein (PTHrP; with antiserum C6; A,E); PTHrP (with antiserum C7; B,F); PTHrP (with antiserum C13; C,G); and parathyroid hormone1 receptor (PTH1R; D,H) was performed with specific antibodies. Representative examples of a low‐grade PCa (A–D) and a high‐grade PCa (E–H) are shown. Negative controls (without corresponding primary antibody) exhibited no positivity (data not shown). Original amplifications, ×200.
Table 1 Diagnostic sensitivity and specificity of CD34, parathyroid hormone‐related protein (with antisera C6 and C7), parathyroid hormone1 receptor, osteoprotegerin and receptor activator of nuclear factor‐κ B ligand to distinguish patients with low‐grade and high‐grade prostate carcinoma.
| Cut‐off* | Low‐grade PCa (⩾ cut‐off/total) | High‐grade PCa (⩾ cut‐off/total) | Sensitivity (95% CI) (%) | Specificity (95% CI) (%) | |
|---|---|---|---|---|---|
| CD34 | 1 | (22/22) | (23/23) | 100 | 0 |
| 2 | (9/22) | (19/23) | 83 (72 to 94) | 59 (45 to 73) | |
| 3 | (2/22) | (5/23) | 22 (10 to 34) | 91 (83 to 99) | |
| PTHrP‐C6 | 3 | (15/22) | (25/25) | 100 | 32 (19 to 45) |
| 4 | (10/22) | (25/25) | 100 | 54 (40 to 68) | |
| 6 | (7/22) | (23/25) | 92 (84 to 100) | 68 (55 to 81) | |
| PTHrP‐C7 | 2 | (14/22) | (23/25) | 96 (90 to 100) | 36 (22 to 50) |
| 4 | (8/22) | (21/25) | 84 (74 to 94) | 64 (50 to 78) | |
| 6 | (6/22) | (12/25) | 48 (34 to 62) | 73 (60 to 86) | |
| PTH1R | 3 | (15/22) | (24/25) | 96 (90 to 100) | 32 (19 to 45) |
| 4 | (11/22) | (22/25) | 88 (79 to 97) | 50 (36 to 64) | |
| 6 | (9/22) | (18/25) | 72 (59 to 85) | 59 (45 to 73) | |
| OPG | 2 | (21/22) | (25/25) | 100 | 4 (0 to 10) |
| 4 | (12/22) | (21/25) | 84 (74 to 94) | 45 (31 to 59) | |
| 6 | (1/22) | (14/25) | 56 (42 to 70) | 95 (89 to 100) | |
| RANKL | 2 | (14/22) | (23/25) | 92 (84 to 100) | 36 (22 to 50) |
| 4 | (1/22) | (18/25) | 72 (59 to 85) | 95 (89 to 100) | |
| 6 | (0/22) | (13/25) | 52 (38 to 66) | 100 |
PCa, prostate carcinoma; PTH1R, parathyroid hormone1 receptor; PTHrP, parathyroid hormone‐related protein; OPG, osteoprotegerin; RANKL, receptor activator of nuclear factor‐κ B ligand.
*The score values used as reference limits were: 1, 2 and 3 (for CD34); quartile 1, moderate staining (4), and quartile 3 (for each bone cytokine studied), as described in the text.
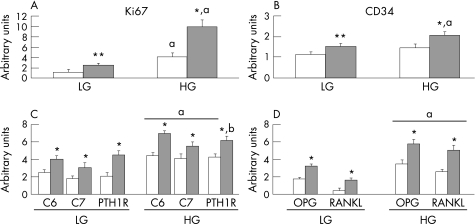
Only 6/22 low‐grade tumours had Ki67 <1%, whereas score values for this marker were consistently ⩾1% in high‐grade tumours. On the other hand, 13/25 of the high‐grade tumours had Ki67 >9%, whereas all low‐grade tumours failed to show values above this percentage. The mean score values for both Ki67 and CD34 were significantly higher in the neoplastic area than in the adjacent non‐tumoral region in both groups studied (fig 3A, B).
Figure 3 Immunohistochemical score values for Ki67 (A) and CD34 (B), parathyroid hormone‐related protein (with antisera C6 and C7) and the parathyroid hormone1 receptor (PTH1R; C), osteoprotegerin (OPG) and receptor activator of nuclear factor‐κ B ligand (RANKL; D) in low‐grade (LG) and high‐grade (HG) groups with prostate carcinoma. White and grey bars denote the corresponding values as mean (standard error of the mean) in non‐tumoral and neoplastic area, respectively. *p<0.01; **p<0.05 vs corresponding values in non‐tumoral area (by Wilcoxon's rank test). ap<0.01; bp<0.05 vs corresponding values in LG tumours (by Mann–Whitney U test).
PTHrP (with antisera C6 or C7) immunoreactivity was diffuse and localised to the cytoplasm of epithelial cells and the stromal tissue in both tumoral and adjacent non‐tumoral areas. PTH1R positivity was also present in epithelial cells, in both cytoplasm and cell membranes (fig 2). Staining intensity for both PTHrP and the PTH1R was stronger in the neoplastic than in non‐tumoral epithelium, and in the high‐grade compared with the low‐grade tumours (fig 3C). Using antiserum C6, 100% of high‐grade tumours had moderate to strong positivity (score value ⩾4) in the neoplastic epithelium. Significant correlations were observed between score values for PTHrP‐C6 and those for Ki67 (p<0.01), PTH1R (p<0.01), or PTHrP‐C7 (p<0.01), and also between PTHrP‐C7 and PTH1R values (p<0.05).
Previous evaluation of PTHrP in PCa found a lower incidence of PTHrP immunostaining using N‐terminal antibodies.15,18,19 In this study, some of the low‐grade (n = 19) and high‐grade (n = 19) tumours were also stained for PTHrP using N‐terminal antiserum C13. The staining pattern with this antiserum was similar although less intense than that observed with the other PTHrP antisera used (fig 2). PTHrP‐C13 score values significantly correlated with those of PTHrP‐C6 (p<0.05), PTHrP‐C7 (p<0.01), or PTH1R (p<0.01). However, 5% and 10 % high‐grade and low‐grade tumours, respectively, showed no staining for PTHrP in the neoplastic epithelium using antiserum C13. In contrast, by using the C‐terminal PTHrP antisera, all tumours were positive with antiserum C6, and only 4 % of low‐grade tumours were negative with antiserum C7.
We failed to find any significant correlation between the score values for CD34 and those for PTHrP (with all antisera used) or the PTH1R in the neoplastic area in all the PCa samples studied.
Positivity for RANKL and OPG in the neoplastic area was found in most PCa samples: 82% and 100% (low‐grade tumours) and 96% and 100 % (high‐grade tumours), respectively. Both OPG and RANKL immunoreactivities were stronger in the neoplastic than in non‐tumoral epithelium, and in the high‐grade than in the low‐grade tumours (fig 3D). In the low‐grade tumours, the mean RANKL/OPG score ratios were 0.51 and 0.26, in the neoplastic and non‐tumoral areas, respectively; which were significantly (p<0.05) lower than those in the high‐grade tumours: 0.87 and 0.72, respectively. OPG score values were correlated with those of either RANKL (p<0.01), PTHrP‐C6 (p<0.01) and PTHrP‐C7 (p<0.05), and those for RANKL also significantly correlated with PTHrP‐C6 values (p<0.01).
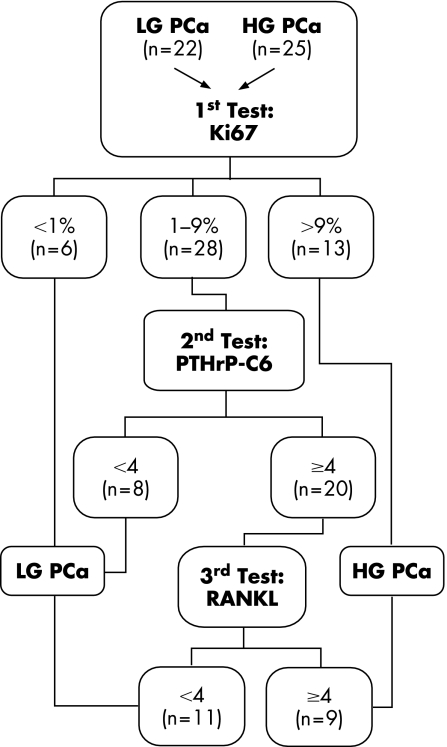
The best sensitivity and specificity values (%) were for PTHrP‐C6 and RANKL, respectively, using a score value of 4—corresponding to moderate staining—as cut‐off (table 1). Therefore, using the PTHrP‐C6 immunostaining followed by the RANKL staining allowed us to correctly classify 44/47 cases. In contrast, after PTHrP‐C6 staining, evaluation of either OPG or RANKL positivity by using the third quartile as cut‐off, which also yields a high specificity (table 1), incorrectly diagnosed 12/47 cases. Figure 4 thus shows a proposed algorithm to differentiate low‐grade and high‐grade PCa in those tumours which cannot be distinguished by Ki67 scores (in the range 1–9%), based on subsequent immunostaining for PTHrP‐C6 and RANKL.
Figure 4 Proposed algorithm to discriminate low‐grade and high‐grade prostate carcinoma (PCa). By using this manuever, 44/47 patients were correctly classified according to Gleason score. HG, high‐grade; LG, low‐grade; PTHrP, parathyroid hormone‐related protein; RANKL, receptor activator of nuclear factor‐kB ligand.
Discussion
A variety of biochemical factors have been examined as putative stage‐specific markers or prognostic factors in patients with PCa.5,6,7,8,9,10,11,12 Thus, an increase of either proliferative index, as measured by Ki67, or apoptotic index, and changes in the cell cycle arresting protein p27 have all been shown to be adversely prognostic in PCa.12 In addition, vascular endothelial growth factor has recently been suggested to promote osteoblastic lesions at PCa bone metastasis.6 Furthermore, various renin–angiotensin system components, including ACE as well as angiotensin II and its AT1 receptor subtype, are present in the human prostate and overexpressed in PCa, mainly in advanced disease.5,7,8,9 Interestingly, a recent study found the presence of an ACE genotype associated with the greatest ACE activity correlating with high‐grade PCa.8
As expected, we found high positivity for CD34 (a marker of angiogenesis) and Ki67 (a proliferation marker) in PCa samples.11,31 In addition, we showed that all of bone cytokines studied are overstained in the neoplastic area of PCa, mainly in the high‐grade tumours.
Most previous studies showing a high incidence of positive PTHrP immunostaining in PCa have used antibodies against mid‐region or C‐terminal epitopes.15,18,19 Moreover, staining by these antibodies in contrast to that by N‐terminal antibodies has shown to correlate with the histological grade of PCa.16,18,19 We presently found a higher number of negative cases and a lower staining intensity with an N‐terminal PTHrP antiserum compared with the use of two different C‐terminal PTHrP antisera in PCa samples. Thus, our present findings support the notion that PTHrP fragments other than its N‐terminal fragment might be preferentially present in PCa.15 Furthermore, we found that all of the PCa samples immunostained for the PTH1R, and this positivity correlated with PTHrP immunostaining in the neoplastic epithelium; this is in contrast to previous findings using in situ hybridisation for the PTH1R detection.16 Differences in patient population and/or methods to evaluate the PTH1R in the tumour samples might explain the different results in that report and this study. We found no significant correlation between CD34 and either PTHrP or the PTH1R immunostaining score values in the tumoral area in the PCa samples studied. PTHrP, by interaction with the PTH1R, has been shown to inhibit tumour angiogenesis in a PCa cell line.32 However, PTHrP can also induce the expression of interleukin‐8, an angiogenic factor, in PCa cells by an intracrine mechanism.20 This is in contrast to the consistent stimulatory effect of PTHrP on PCa cell proliferation which has been reported to occur through autocrine/paracrine and intracrine mechanisms.21 Collectively, these data and the present results therefore suggest that the mitogenic action of PTHrP may predominate over angiogenesis to favour PCa growth.
A previous immunohistochemical study failed to detect OPG in most (8/10) primary PCa tissues (with Gleason score of 6–9).26 Using a sensitive immunohistochemical procedure, we were able to detect both OPG and RANKL in the neoplastic areas of the majority of both tumour groups studied. In addition, an important and novel finding of this study was that the neoplastic epithelium showed an increased immunostaining for both osteoclastogenesis‐related proteins associated with tumour grade and PTHrP positivity. PTHrP might affect the expression of these proteins by PCa cells, as occurs in osteoblasts.33 We also found a significantly higher RANKL/OPG ratio in the high‐grade PCa samples. In these tumours, this osteomimetic feature might facilitate the successful interaction with bone and thus the risk of skeletal involvement.2
In conclusion, identification of stage‐specific PCa markers is now evolving towards more accurate molecular systems. We report here that combined determination of PTHrP (with an antiserum recognising a C‐terminal epitope) and RANKL by immunohistochemistry can successfully distinguish less and more aggressive tumours in most patients with PCa.
Take‐home messages
We report an immunohistochemical study to evaluate some bone cytokines in localised prostate carcinoma (PCa) specimens.
This is a common malignancy in men whose progression is highly variable and cannot be satisfactorily predicted by histological criteria alone.
The combined determination of C‐terminal parathyroid hormone‐related protein and receptor activator of nuclear factor‐κ B ligand immunoreactivities in most patients with PCa (with Ki67 values between 1 % and 9 %) is a useful approach to discriminate low‐grade and high‐grade tumours.
Acknowledgements
Dr JJ Garnizo and T Carrizosa provided technical support. FCP‐M and VA are fellows of Fundación Conchita Rábago. This work was supported in part by Fundación de Investigación en Urología and Instituto de Salud Carlos III (C03/08).
Abbreviations
OPG - osteoprotegerin
PCa - prostate carcinoma
PTH - parathyroid hormone
PTH1R - PTH1 receptor
PTHrP - PTH‐related protein
RANKL - receptor activator of nuclear factor‐κ B ligand
Footnotes
Competing interests: None.
References
- 1.Jemal A, Murray T, Samuels A.et al Cancer statistics, 2003. CA Cancer J Clin 2003535–26. [DOI] [PubMed] [Google Scholar]
- 2.Keller E T. The role of osteoclastic activity in prostate cancer skeletal metastases. Drugs Today (Barc) 20023891–102. [DOI] [PubMed] [Google Scholar]
- 3.Blute M L, Bergstralh E J, Partin A W.et al Validation of parting tables for predicting pathological stage of clinically localized prostate cancer. J Urol 2000641591–1595. [PubMed] [Google Scholar]
- 4.Kattan M W, Eastham J A, Stapleton A M.et al A preoperative nomogram for disease recurrence following radical prostatectomy for prostate cancer. J Natl Cancer Inst 199890766–771. [DOI] [PubMed] [Google Scholar]
- 5.Uemura H, Hasumi H, Ishiguro H.et al Renin‐angiotensin system is an important factor in hormone refractory prostate cancer. Prostate 200666822–830. [DOI] [PubMed] [Google Scholar]
- 6.Dai J, Kitagawa Y, Zhang J.et al Vascular endothelial growth factor contributes to the prostate cancer‐induced osteoblast differentiation mediated by bone morphogenetic protein. Cancer Res 200464994–999. [DOI] [PubMed] [Google Scholar]
- 7.O'Mahony O A, Barker S, Puddefoot J R.et al Synthesis and secretion of angiotensin II by the prostate gland in vitro. Endocrinology 2005146392–398. [DOI] [PubMed] [Google Scholar]
- 8.Medeiros R, Vasconcelos A, Costa S.et al Linkage of angiotensin I‐converting enzyme gene insertion/deletion polymorphism to the progression of human prostate cancer. J Pathol 2004202330–335. [DOI] [PubMed] [Google Scholar]
- 9.Wennemuth G, Aumuller G. Angiotensin II‐mediated calcium signals and mitogenesis in human prostate stromal cell line hPCPs. Br J Pharmacol 20051443–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Prtilo A, Leach F S, Markwalder R.et al Tissue microarray analysis of hMSH2 expression predicts outcome in men with prostate cancer. J Urol 20051741814–1818. [DOI] [PubMed] [Google Scholar]
- 11.Rubio J, Ramos D, López‐Guerrero J A.et al Immunohistochemical expression of ki‐67 antigen, cox‐2 and bax/bcl‐2 in prostate cancer; prognostic value in biopsies and radical prostatectomy specimens. Eur Urol 200548745–751. [DOI] [PubMed] [Google Scholar]
- 12.Quinn D I, Henshall S M, Sutherland R L. Molecular markers of prostate cancer outcome. Eur J Cancer 200541858–887. [DOI] [PubMed] [Google Scholar]
- 13.Rankin W, Grill V, Martin T J. Parathyroid hormone‐related protein and hypercalcaemia. Cancer 1997801564–1571. [DOI] [PubMed] [Google Scholar]
- 14.Clemens T L, Cormier S, Eichinger A.et al Parathyroid hormone‐related protein and its receptors: nuclear functions and roles in the renal and cardiovascular systems, the placental trophoblasts and the pancreatic islets. Br J Phamacol 20011341113–1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu G, Iwamura M, di Sant'Agnese P A.et al Characterization of the cell‐specific expression of parathyroid hormone‐related protein in normal and neoplastic prostate tissue. Urology 199851110–120. [DOI] [PubMed] [Google Scholar]
- 16.Iddon J, Bundred N J, Hoyland J.et al Expression of parathyroid hormone‐related protein and its receptor in bone metastases from prostate cancer. J Pathol 2000191170–174. [DOI] [PubMed] [Google Scholar]
- 17.Asadi F, Kukreja S. Parathyroid hormone‐related protein in prostate cancer. Crit Rev Eukaryot Gene Expr 20051515–28. [DOI] [PubMed] [Google Scholar]
- 18.Iwamura M, di Sant'Agnese P A, Wu G.et al Immunohistochemical localization of parathyroid hormone‐related protein in human prostate cancer. Cancer Res 1993531724–1726. [PubMed] [Google Scholar]
- 19.Asadi F, Farraj M, Sharifi R.et al Enhanced expression of parathyroid hormone‐related protein in prostate cancer as compared with benign prostatic neoplasia. Hum Pathol 1996271319–1323. [DOI] [PubMed] [Google Scholar]
- 20.Gujral A, Burton D W, Terkeltaub R.et al Parathyroid hormone‐related protein induces interleukin‐8 production by prostate cancer cells via a novel intracrine mechanism not mediated by its classical nuclear localization sequence. Cancer Res 2001612282–2288. [PubMed] [Google Scholar]
- 21.Tovar Sepulveda V A, Falzon M. Parathyroid hormone‐related protein enhances PC‐3 prostate cancer cell growth via both autocrine/paracrine and intracrine pathways. Regul Pept 2002105109–120. [DOI] [PubMed] [Google Scholar]
- 22.Rabbani S A, Gladu J, Harakidas P.et al Over‐production of parathyroid hormone‐related peptide results in increased osteolytic metastasis by prostate cancer cells in vivo. Int J Cancer 199980257–264. [DOI] [PubMed] [Google Scholar]
- 23.Deftos L J, Barken I, Burton D W.et al Direct evidence that PTHrP expression promotes prostate cancer progression in bone. Biochem Biophys Res Commun 2005327468–472. [DOI] [PubMed] [Google Scholar]
- 24.Goltzman D. Osteolysis and cancer. J Clin Invest 20011071219–1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Theoleyre S, Wittrant Y, Tat S K.et al The molecular triad OPG/RANK/RANKL: involvement in the orchestration of pathophysiological bone remodelling. Cytokine Growth F R 200415457–475. [DOI] [PubMed] [Google Scholar]
- 26.Brown J M, Corey E, Lee Z D.et al Osteoprotegerin and RANK ligand expression in prostate cancer. Urology 200157611–616. [DOI] [PubMed] [Google Scholar]
- 27.Holen I, Croucher P I, Hamdy F C.et al Osteoprotegerein (OPG) is a survival factor for human prostate cancer cells. Cancer Res 2002621619–1623. [PubMed] [Google Scholar]
- 28.Jung K, Stephan C, Semjonow A.et al Serum osteoprotegerin and receptor activator of nuclear factor‐κ B ligand as indicators of disturbed osteoclastogenesis in patients with prostate cancer. J Urol 20031702302–2305. [DOI] [PubMed] [Google Scholar]
- 29.Albar J P, de Miguel F, Esbrit P.et al Immunohistochemical detection of parathyroid hormone‐related protein in a rare variant of hepatic neoplasm (sclerosing hepatic carcinoma). Hum Pathol 199627728–731. [DOI] [PubMed] [Google Scholar]
- 30.Valin A, García‐Ocaña A, de Miguel F.et al Antiproliferative effect of the C‐terminal fragments of parathyroid hormone‐related protein, PTHrP (107–111), on osteoblastic osteosarcoma cells. J Cell Physiol 1997170209–215. [DOI] [PubMed] [Google Scholar]
- 31.Bono A V, Celato N, Cova V.et al Microvessel density in prostate carcinoma. Prostate Cancer Prostatic Dis 20025123–127. [DOI] [PubMed] [Google Scholar]
- 32.Bakre M M, Zhu Y, Yin H.et al Parathyroid hormone‐related peptide is a naturally occurring, protein kinase A‐dependent angiogenesis inhibitor. Nature Med 20028995–1003. [DOI] [PubMed] [Google Scholar]
- 33.Kondo H, Guo J, Bringhurst F R. Cyclic adenosine monophosphate/protein kinase A mediates parathyroid hormone/parathyroid hormone‐related protein receptor regulation of osteoclastogenesis and expression of RANKL and osteoprotegerin mRNAs by marrow stromal cells. J Bone Miner Res 2002171667–1679. [DOI] [PubMed] [Google Scholar]