Abstract
Objective
To assess the long term prognostic value of N‐terminal pro‐brain natriuretic peptide (NT‐proBNP) on admission and its prognostic interaction with both admission troponin T (TnT) concentrations and resolution of ST segment elevation in fibrinolytic treated ST elevation myocardial infarction (STEMI).
Design and setting
Substudy of the ASSENT (assessment of the safety and efficacy of a new thrombolytic) ‐2 and ASSENT‐PLUS trials.
Patients
NT‐proBNP and TnT concentrations were determined on admission in 782 patients. According to NT‐proBNP concentrations, patients were divided into three groups: normal concentration (for patients ⩽ 65 years, ⩽ 184 ng/l and ⩽ 268 ng/l and for those > 65 years, ⩽ 269 ng/l and ⩽ 391 ng/l in men and women, respectively); higher than normal but less than the median concentration (742 ng/l); and above the median concentration. For TnT, a cut off of 0.1 μg/l was used. Of the 782 patients, 456 had ST segment resolution (< 50% or ⩾ 50%) at 60 minutes calculated from ST monitoring.
Main outcome measures
All cause one year mortality.
Results
One year mortality increased stepwise according to increasing concentrations of NT‐proBNP (3.4%, 6.5%, and 23.5%, respectively, p < 0.001). In receiver operating characteristic analysis, NT‐proBNP strongly trended to be associated more with mortality than TnT and time to 50% ST resolution (area under the curve 0.81, 95% confidence interval (CI) 0.72 to 0.9, 0.67, 95% CI 0.56 to 0.79, and 0.66, 95% CI 0.56 to 0.77, respectively). In a multivariable analysis adjusted for baseline risk factors and TnT, both raised NT‐proBNP and ST resolution < 50% were independently associated with higher one year mortality, whereas raised TnT contributed independently only before information on ST resolution was added to the model.
Conclusion
Admission NT‐proBNP is a strong independent predictor of mortality and gives, together with 50% ST resolution at 60 minutes, important prognostic information even after adjustment for TnT and baseline characteristics in STEMI.
Keywords: acute myocardial infarction, brain natriuretic peptide, prognosis, electrocardiography
Mortality risk is quite variable among patients with fibrinolytic treated ST elevation myocardial infarction (STEMI).1 Careful and early risk evaluation of each patient is therefore important. Several clinical baseline variables have been identified as important predictors of outcome, especially age, heart rate, and blood pressure.2 In recent years, interest has been focused on cardiac biomarkers and early resolution of ST segment elevation for risk stratification in STEMI.3,4 Until now, the most evaluated biomarker has been troponin T (TnT) (or troponin I) on admission, which gives strong prognostic information, also in combination with ST resolution.5,6
Brain natriuretic peptide (BNP) and the N‐terminal part of its prohormone, NT‐proBNP, are released from the cardiac ventricles in response to increased wall stress and to ischaemia per se.7,8 A few previous smaller studies have shown that NT‐proBNP and BNP concentrations are independent predictors of mortality on days 2 to 5 after STEMI.9,10 Also, raised concentrations of NT‐proBNP and BNP on admission in STEMI have been related to adverse outcome in two recent studies.11,12 These studies, however, evaluated only short term mortality. Furthermore, the prognostic interaction of NT‐proBNP and early resolution of ST segment elevation have not been investigated. We therefore evaluated admission NT‐proBNP concentration and its prognostic interaction with admission TnT and ST segment resolution for early risk stratification of patients with STEMI with long term follow up.
METHODS
Patients and study design
This study was a substudy of the ASSENT (assessment of the safety and efficacy of a new thrombolytic) ‐2 and the ASSENT‐PLUS trials.13,14 In brief, the ASSENT‐2 trial was a multicentre study comparing tenecteplase with front loaded alteplase. In the ASSENT‐PLUS trial 434 patients were recruited in Scandinavia and the USA during 1999 and 2000 and evaluated the efficacy and safety of the low molecular weight heparin dalteparin compared with unfractionated heparin as an adjunct to alteplase.
In both studies inclusion criteria were symptoms of acute myocardial infarction (MI) within six hours of onset, ST elevation ⩾ 0.1 mV in two or more limb leads or ⩾ 0.2 mV in two or more contiguous precordial leads or left bundle branch block, and age ⩾ 18 years. Exclusion criteria in both trials were the regular ones for thrombolytic treatment and have been described in detail previously.13,14 In addition, known renal dysfunction (serum creatinine > 150 μmol/l) was an exclusion criterion in the ASSENT‐PLUS trial. Of 1456 patients enrolled in the ASSENT‐2 and ASSENT‐PLUS trials at Swedish hospitals, 782 (with 8.4% one year mortality) had an admission NT‐proBNP sample available and constituted the study population for the present substudy (568 from the ASSENT‐2 and 214 from the ASSENT‐PLUS trial).
Blood samples for biochemical markers
Venous blood samples were collected immediately before the start of thrombolytic and anticoagulation treatment at selected Swedish sites. After centrifugation the EDTA plasma samples were stored frozen at −70°C for central analysis. NT‐proBNP was determined with a sandwich immunoassay on an Elecsys 2010 (Roche Diagnostics). The analytical range extends from 20 000 to 35 000 ng/l. At our laboratory, the total coefficient of variation was 3.3% at a concentration of 209 ng/l and 3% at a concentration of 7431 ng/l. A normal concentration of NT‐proBNP (⩽ 97.5th centile in a healthy population) according to age and sex has been shown to be, for patients ⩽ 65 years, ⩽ 184 ng/l and ⩽ 268 ng/l and, for those > 65 years, ⩽ 269 ng/l and ⩽ 391 ng/l in men and women, respectively.15 TnT was analysed with the third generation TnT assay on an Elecsys 2010 with a detection limit of 0.01 μg/l. A prospectively defined cut off concentration of < 0.1 or ⩾ 0.1 μg/l was used based on previous evaluations of admission TnT in STEMI for risk stratification, which should not be confused with the cut off concentration used for diagnosis of MI.6,11,16,17
ST segment resolution
A subgroup of 456 patients were monitored for 24 hours after admission by continuous vectorcardiography (n = 334) or continuous 12 lead ECG (n = 122). One year mortality was 6.3% in this subgroup and thus similar to the whole ST monitoring substudy population.4,6
These two ST monitoring methods have previously been shown to identify the same risk groups among patients with STEMI.4,6 Inclusion and exclusion criteria for ST monitoring and methods for acquirement of continuous vectorcardiography and ECG recordings and for assessment of ST segment measurements have previously been described.4,6 A cut off level of < 50 and ⩾ 50% ST segment resolution from the maximum ST elevation measured at 60 minutes after the start of recording was used.4,6 We also assessed time to 50% ST segment resolution to evaluate its relation to admission NT‐proBNP concentrations.
Coronary angiography
A predischarge coronary angiogram was scheduled at days 4 to 7 and performed in 179 of the 214 patients from the ASSENT‐PLUS cohort.14 The coronary vessels were divided into 15 segments and the degree of stenosis was analysed.18 A CASS (coronary artery surgery study) score was computed to determine the severity of coronary artery disease.19,20 By adding the regional scores, a CASS score with a possible range of 0–3 was obtained. When calculating the CASS score, the culprit lesion was considered occluded in order to imitate the situation on admission.
Clinical end points
The outcome event in this substudy was all cause one year mortality. One year mortality was evaluated by patient records and telephone contacts.
Statistical analysis
Baseline characteristics were expressed as medians (with 25th to 75th centile) or percentages. Differences in categorical baseline variables between groups according to NT‐proBNP concentration were evaluated with χ2 tests for trend. Differences between median values for continuous variables were evaluated with Kruskal‐Wallis tests or Mann‐Whitney U tests. Correlations were assessed by Spearman's rank statistics. To compare the predictive capacity of NT‐proBNP, TnT, and time to 50% ST resolution, receiver operating characteristic (ROC) curves were used. Kaplan‐Meier curves were constructed to illustrate the risk for death during the one year of follow up and log rank tests were done to compare the risk between strata.
Independent predictors of one year mortality were identified with stepwise multiple logistic regression analyses including age, sex, heart rate, systolic blood pressure, Killip class, previous MI, time to treatment, anterior infarction, TnT, and NT‐proBNP (log transformed (base 10) due to its skewed distribution) in the whole study population. The independent predictors of mortality as well as Killip class, which tended to be independent, were then evaluated in two models: model 1 included TnT and NT‐proBNP and in model 2 information on ST resolution at 60 minutes was added. Additional logistic regression analyses were performed to adjust for study (ASSENT‐2 or ASSENT‐PLUS) and to test for the interaction between NT‐proBNP and ST resolution. In all statistical analyses, p < 0.05 was considered significant. All statistics were calculated with SPSS software (version 12.0; SPSS Inc, Chicago, Illinois, ISA).
RESULTS
General findings
During one year of follow up 66 (8.4%) patients died in the whole study population. More than half of the study population (n = 443) had a normal NT‐proBNP concentration on admission according to age and sex. The remaining patients had a median concentration of 742 ng/l (25th–75th centile 395–1894 ng/l). Table 1 lists clinical characteristics in relation to normal, above normal but below median (intermediate), and above the median (high) NT‐proBNP concentrations. Age, heart rate, Killip class, the rate of previous MI, and time from symptom onset to treatment increased stepwise in relation to higher concentrations of NT‐proBNP. However, the correlation between NT‐proBNP and symptom duration was weak (r = 0.17, p < 0.001). The distribution of NT‐proBNP concentrations and baseline characteristics according to NT‐proBNP were similar in the subgroup of patients with ST monitoring.
Table 1 Clinical characteristics according to N‐terminal pro‐brain natriuretic peptide (NT‐proBNP) concentration on admission.
| Variable | NT‐proBNP concentration | p Value | ||
|---|---|---|---|---|
| Normal* (n = 443) | >Normal but <median (<742 ng/l) (n = 169) | ⩾Median (⩾742 ng/l) (n = 170) | ||
| Age (years) | 63 (55–71) | 68 (59–75) | 74 (67–79) | NA |
| Men | 71.6% | 77.5% | 62.9% | NA |
| Time to treatment (min) | 135 (95–200) | 160 (110–225) | 172 (110–239) | <0.001 |
| Current smoker | 37.6% | 23.1% | 22.5% | <0.001 |
| Diabetes mellitus | 9.7% | 10.7% | 12.4% | 0.34 |
| Hypertension | 25.1% | 29.6% | 32.4% | 0.06 |
| Previous MI | 8.8% | 18.9% | 27.1% | <0.001 |
| Anterior MI | 40.9% | 50.9% | 50.9% | 0.01 |
| SBP (mm Hg) | 140 (125–156) | 145 (130–160) | 140 (125–160) | 0.26 |
| Heart rate (beats/min) | 68 (59–78) | 68 (59–78) | 78 (66–90) | <0.001 |
| Killip class >1 | 9.5% | 15.9% | 25.0% | <0.001 |
| Troponin T ⩾0.1 μg/l | 11.7% | 23.7% | 50.0% | <0.001 |
| ⩾50% ST resolution† | 47.4% | 37.7% | 35.6% | 0.03 |
| Coronary angiography: CASS score‡ | 0.03 | |||
| 0 | 8.0 | 0 | 0 | |
| 1 | 56.3 | 73.3 | 72.7 | |
| 2 | 33.0 | 20.0 | 13.6 | |
| 3 | 2.7 | 6.7 | 13.6 | |
Data are median (25th to 75th centile) or percentage.
*⩽65 or >65 years, ⩽184 or ⩽269 ng/l in men, ⩽65 or >65 years, ⩽268 or ⩽391 ng/l in women; †assessed in 249, 106, and 101 patients in each group, respectively; ‡assessed in 112, 30, and 22, respectively.
CASS, coronary artery surgery study; MI, myocardial infarction; NA, not applicable; SBP, systolic blood pressure.
The prevalence of more severe coronary artery disease tended to increase with increasing NT‐proBNP concentrations.
NT‐proBNP in relation to TnT and ST resolution
Patients with TnT ⩾0.1 μg/l (n = 177, 23%) had much higher concentrations of NT‐proBNP than those with TnT < 0.1 μg/l (678 ng/l (215–2230) v 167 ng/l (69–382), respectively, p < 0.001). There was a moderate positive correlation between concentrations of TnT and NT‐proBNP (r = 0.43, p < 0.001). In the subgroup (n = 456) of patients with ST monitoring, those without 50% ST resolution at 60 minutes (n = 262, 57%) had slightly higher NT‐proBNP concentrations than did those with 50% ST resolution (249 ng/l (109–721) v 174 ng/l (70–504), respectively, p = 0.009), although there was only a weak positive correlation between time to 50% ST resolution and NT‐proBNP concentration (r = 0.13, p = 0.005).
Prognostic value of NT‐proBNP
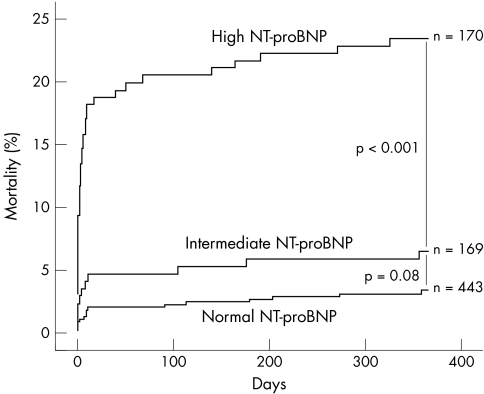
One year mortality increased stepwise according to increasing NT‐proBNP concentration (3.4%, 6.5%, and 23.5%, respectively) (fig 1). Accordingly, there was a striking mortality difference between patients with high and those with normal concentration of NT‐proBNP (odds ratio (OR) 8.8, 95% confidence interval (CI) 4.7 to 16.4, p < 0.001). Patients with high NT‐proBNP concentration had a significantly higher mortality than patients with intermediate concentration (OR 4.4, 95% CI 2.2 to 9.0, p < 0.001).
Figure 1 Cumulative mortality during one year according to the concentration of N‐terminal pro‐brain natriuretic peptide (NT‐proBNP) (n = 782).
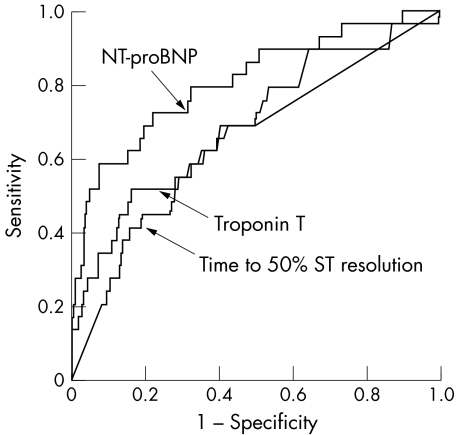
Figure 2 illustrates the univariable association of NT‐proBNP and TnT concentration and time to 50% ST resolution with one year mortality by ROC curves. Notably, the area under the curve (AUC) showed a strong trend for NT‐proBNP to be more strongly associated with mortality than the other variables (NT‐proBNP v TnT, p = 0.056 and NT‐proBNP v time to 50% ST resolution, p = 0.052). Moreover, when evaluated in the whole study population the AUCs for NT‐proBNP (0.79) and TnT (0.71) were unaltered and NT‐proBNP was significantly more strongly related to mortality than was TnT (p = 0.026). The AUC for NT‐proBNP (0.76, n = 574) was also similar for patients without previous MI and in Killip class I on admission.
Figure 2 Receiver operating characteristic curve for death at one year for NT‐proBNP, troponin T (TnT), and time to 50% ST segment resolution with an area under the curve of 0.81 (95% confidence interval (CI) 0.72 to 0.90), 0.67 (95% CI 0.56 to 0.79), and 0.66 (95% CI 0.56 to 0.77), respectively (n = 456).
A high NT‐proBNP concentration (> 742 ng/l) yielded a sensitivity and specificity in the whole study population of 61% and 82%, respectively. The corresponding positive and negative predictive values were 24% and 96%, respectively.
In a multivariable analysis of all patients in this study, and thus not including information on early ST resolution in the model, age, heart rate, systolic blood pressure, “raised” TnT, and log(NT‐proBNP) were independently associated with one year mortality (table 2, model 1). In a restricted version of model 1 that included only patients with data on ST resolution (n = 456), NT‐proBNP but not TnT (OR 1.52, 95% CI 0.60 to 3.85) contributed independently. When 50% ST resolution at 60 minutes was added to the model, both log(NT‐proBNP) and < 50% ST resolution were independently associated with mortality in contrast to TnT (table 2, model 2). The results were similar when NT‐proBNP was entered as a categorical variable in model 2 (OR for high NT‐proBNP v normal NT‐proBNP 3.34, 95% CI 1.06 to 10.54, p = 0.03). Also, the results were unchanged when TnT and ST resolution (log transformed) were entered in a continuous format and with adjustment for study (ASSENT‐2 or ASSENT‐PLUS).
Table 2 Univariable and multivariable logistic regression analysis for one year mortality (odds ratios and 95% confidence intervals).
| Variable | Univariable analysis | Multivariable analyses | ||
|---|---|---|---|---|
| Model 1 (n = 782) | Model 2 (n = 456) | Model 2 with interaction | ||
| Age (years) | 1.13 (1.10 to 1.17) | 1.11 (1.06 to 1.15) | 1.08 (1.02 to 1.14) | 1.09 (1.03 to 1.15) |
| Heart rate (beats/min) | 1.04 (1.03 to 1.05) | 1.02 (1.01 to 1.04) | 1.02 (1.0 to 1.05) | 1.03 (1.0 to 1.05) |
| SBP (mm Hg) | 0.98 (0.97 to 0.99) | 0.98 (0.96 to 0.99) | 0.98 (0.96 to 0.99) | 0.98 (0.96 to 0.99) |
| Killip class >1 | 3.28 (1.86 to 5.76) | 1.74 (0.89 to 3.40) | 1.11 (0.38 to 3.26) | 1.09 (0.37 to 3.20) |
| Log(NT‐proBNP)* | 3.04 (2.33 to 3.97) | 1.69 (1.20 to 2.37) | 2.27 (1.33 to 3.87) | NA |
| ST resolution <50%† | NA | NA | NA | 2.97 (1.58 to 5.59) |
| ST resolution ⩾50%† | NA | NA | NA | 1.15 (0.50 to 2.63) |
| ST resolution <50%† | 3.02 (1.20 to 7.56) | NA | 3.06 (1.07 to 8.76) | 1.42 (0.41 to 4.90)‡ |
| Troponin T ⩾0.1 (µg/l) | 4.56 (2.72 to 7.65) | 2.25 (1.21 to 4.19) | 1.35 (0.52 to 3.48) | 1.30 (0.49 to 3.50) |
*log(NT‐proBNP) standardised to have mean = 0 and SD = 1; †at 60 minutes; ‡odds ratio for patient with mean log(NT‐proBNP) for NT‐proBNP of 256 ng/l.
Combination of NT‐proBNP with TnT and ST resolution
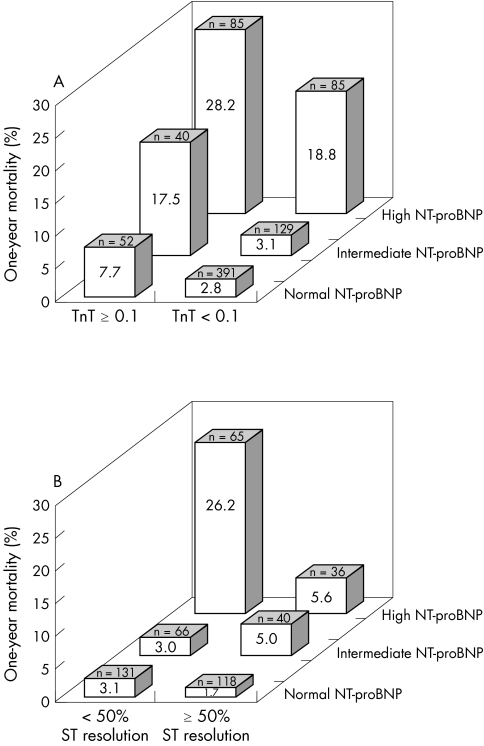
When stratification was based on the concentration of TnT, mortality increased gradually according to increasing NT‐proBNP concentration in both patients with and without a TnT rise (fig 3A).
Figure 3 (A) One year mortality according to the combination of NT‐proBNP (ng/l) and TnT (μg/l) (n = 782). (B) One year mortality according to the combination of NT‐proBNP (ng/l) and ST segment resolution (%) at 60 minutes (n = 456).
There was a profound difference in mortality between the group with high NT‐proBNP and without ST resolution and the group with normal NT‐proBNP and with ST resolution (OR 20.5, 95% CI 4.6 to 92.4, p < 0.001) (fig 3B). Notably, the difference in mortality between patients with and patients without ST resolution was mainly restricted to those with high concentrations of NT‐proBNP. The result was similar when other classifications of NT‐proBNP and ST resolution were used. Accordingly, there was a significant interaction between NT‐proBNP and 50% ST resolution at 60 minutes (p = 0.04) (table 2).
DISCUSSION
NT‐proBNP and prognosis
Our study shows that admission NT‐proBNP is a strong independent predictor of long term mortality in STEMI in accordance with previous evaluations of NT‐proBNP (and BNP) and short term mortality.11,12 For the first time, NT‐proBNP was evaluated together with ST resolution, TnT, and other well known risk factors, and still independently predicted mortality. As in a previous trial, NT‐proBNP were equally predictive in patients without previous MI and signs of heart failure on admission.11 Accordingly, Killip class provided no independent prognostic information when NT‐proBNP was added to the multivariable model (table 2).
Although more than half of the study population had normal concentrations of NT‐proBNP, in contrast to STEMI studies with later sample time points, the predictive capacity seen in these trials was also maintained with admission sample acquisition.9,10 This is in line with a previous small study in which there was no difference in predictive capacity according to NT‐proBNP concentrations on admission or after two days following STEMI.21
We found only a weak correlation between symptom duration and NT‐proBNP, which was somewhat unexpected considering the time dependent rise of BNP in the early phase after STEMI.22,23 One possible explanation for this is that a patient's recollection of the symptom duration is highly subjective. Thus, admission TnT, which is believed to be a more objective marker of ischaemic time, had a stronger correlation to NT‐proBNP.5,6
As shown in previous acute coronary syndromes studies, increased NT‐proBNP concentration was also associated with more severe coronary artery disease in patients with STEMI.24
Combination of NT‐proBNP with TnT and ST resolution
When NT‐proBNP was tested in multivariable analysis including well known predictors of outcome and TnT but not ST resolution (table 2, model 1), both NT‐proBNP and TnT contributed independently to mortality prediction in contrast to previous studies.11,12 However, when model 1 was restricted to patients with data on ST resolution, TnT no longer contributed independently, which probably is explained by the smaller sample size and fewer events in this subgroup of patients. Lastly, when information on ST resolution at 60 minutes was added, NT‐proBNP and ST resolution predicted mortality independently in contrast to TnT (table 2, model 2). Thus, these results suggest that NT‐proBNP and 50% ST resolution at 60 minutes are complementary concerning their pathophysiological mechanisms in relation to mortality. There was a significant interaction between NT‐proBNP and ST resolution and the benefit of early ST resolution was mainly restricted to patients with high NT‐proBNP concentrations (table 2, fig 3B). In contrast, NT‐proBNP and TnT seemed to reflect more similar mechanisms in relation to mortality as indicated by a moderate correlation. The finding that NT‐proBNP is an indicator of myocardial ischaemia per se8 and that TnT is an indicator of myocardial necrosis may to some extent explain why NT‐proBNP has greater prognostic accuracy on admission in STEMI than TnT, as discussed by Galvani et al,11 but also why they in part seem to be markers of similar pathophysiology in the early phase of STEMI.
However, the knowledge of TnT concentration in addition to NT‐proBNP provided further risk stratification on admission (fig 3A), especially before information was obtained on ST resolution at 60 minutes.
The combination of NT‐proBNP and early ST resolution improved risk prediction. Hence, one third of the high risk patients with high NT‐proBNP who achieved early ST resolution could be stratified into a moderate to low risk group, which may be explained by subsequent early tissue level reperfusion.25 We can hypothesise that the patients with high concentrations of NT‐proBNP on admission have either a large ongoing MI or previously established left ventricular dysfunction with a subsequent raised risk of adverse outcome unless there is early tissue level reperfusion. On the other hand, patients with normal admission NT‐proBNP (more than half of the population) were at low risk almost regardless of 50% ST resolution.
Identification of high risk patients with high NT‐proBNP on admission in STEMI may be helpful for selection of more intense interventional or pharmacological treatment strategies. Our study suggests that early tissue level reperfusion is especially important in patients with raised NT‐proBNP concentration and can alter the adverse outcome for this high risk group. Thus, one may speculate that primary angioplasty can be valuable for these high risk patients, since tissue level reperfusion is achieved more often with primary angioplasty than with thrombolysis.26 However, this and other new treatment strategies according to admission NT‐proBNP concentration need to be tested in prospective trials.
Limitations
One limitation is that the prognostic interaction of NT‐proBNP and ST resolution could be studied only in a subgroup of the study population with a lower one year mortality than that of the other patients, although baseline characteristics were similar. The mortality among the patients with a blood sample (NT‐proBNP) was similar to that of the entire ASSENT‐2 study population in contrast to the lower mortality in patients with ST monitoring as reported in a previous study.6 This lower mortality is in accordance with previous trials that evaluated ST resolution and is probably explained by the time criteria for ST monitoring, which excluded some of the patients with fatal early events.3,4 Also, patients with left bundle branch block, a high risk group, were prospectively excluded from ST monitoring.1
Another limitation is that we had no information on renal function, which has been shown to be independently associated with both NT‐proBNP concentration and mortality in a large population with unstable coronary artery disease.27 However, in a previous smaller study that evaluated admission NT‐proBNP in STEMI in which information on renal failure was available, renal dysfunction was not independently associated with mortality.11 Thus, information on renal dysfunction probably would not alter our results that much.
Conclusion
NT‐proBNP on admission is a strong independent predictor of long term mortality in patients with STEMI treated with fibrinolytics. When evaluated together with admission TnT and ST resolution at 60 minutes, both NT‐proBNP and early ST resolution remain independently associated with mortality in contrast to TnT. The combination of NT‐proBNP and ST resolution at 60 minutes gives complementary early information on prognosis and provides even better risk stratification in patients with STEMI.
ACKNOWLEDGEMENTS
This study was supported by grants from the Swedish Heart and Lung Foundation; Boehringer Ingelheim, Skärholmen, Sweden; Ortivus AB, Täby, Sweden; and GE Medical Systems, Information Technologies, Milwaukee, Wisconsin, USA. We thank Johan Lindbäck for statistical advice.
Abbreviations
ASSENT - assessment of the safety and efficacy of a new thrombolytic
AUC - area under the curve
BNP - brain natriuretic peptide
CASS - coronary artery surgery study
CI - confidence interval
MI - myocardial infarction
NT‐proBNP - N‐terminal pro‐brain natriuretic peptide
OR - odds ratio
ROC - receiver operating characteristic
STEMI - ST elevation myocardial infarction
TnT - troponin T
Footnotes
Competing interests: None declared.
References
- 1.FTT Collaborative Group Indications for fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1000 patients. Fibrinolytic therapy trialists' (FTT) collaborative group. Lancet 1994343311–322. [PubMed] [Google Scholar]
- 2.Lee K L, Woodlief L H, Topol E J.et al Predictors of 30‐day mortality in the era of reperfusion for acute myocardial infarction: results from an international trial of 41,021 patients. GUSTO‐I Investigators. Circulation 1995911659–1668. [DOI] [PubMed] [Google Scholar]
- 3.Schroder R, Wegscheider K, Schroder K.et al Extent of early ST segment elevation resolution: a strong predictor of outcome in patients with acute myocardial infarction and a sensitive measure to compare thrombolytic regimens. A substudy of the international joint efficacy comparison of thrombolytics (INJECT) trial. J Am Coll Cardiol 1995261657–1664. [DOI] [PubMed] [Google Scholar]
- 4.Johanson P, Jernberg T, Gunnarsson G.et al Prognostic value of ST‐segment resolution‐when and what to measure. Eur Heart J 200324337–345. [DOI] [PubMed] [Google Scholar]
- 5.Ohman E M, Armstrong P W, White H D.et al Risk stratification with a point‐of‐care cardiac troponin T test in acute myocardial infarction. GUSTO III Investigators. Global use of strategies to open occluded coronary arteries. Am J Cardiol 1999841281–1286. [DOI] [PubMed] [Google Scholar]
- 6.Bjorklund E, Lindahl B, Johanson P.et al Admission troponin T and measurement of ST‐segment resolution at 60 min improve early risk stratification in ST‐elevation myocardial infarction. Eur Heart J 200425113–120. [DOI] [PubMed] [Google Scholar]
- 7.Levin E R, Gardner D G, Samson W K. Natriuretic peptides. N Engl J Med 1998339321–328. [DOI] [PubMed] [Google Scholar]
- 8.Tateishi J, Masutani M, Ohyanagi M.et al Transient increase in plasma brain (B‐type) natriuretic peptide after percutaneous transluminal coronary angioplasty. Clin Cardiol 200023776–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Omland T, Aakvaag A, Bonarjee V V.et al Plasma brain natriuretic peptide as an indicator of left ventricular systolic function and long‐term survival after acute myocardial infarction: comparison with plasma atrial natriuretic peptide and N‐terminal proatrial natriuretic peptide. Circulation 1996931963–1969. [DOI] [PubMed] [Google Scholar]
- 10.Richards A M, Nicholls M G, Yandle T G.et al Plasma N‐terminal pro‐brain natriuretic peptide and adrenomedullin: new neurohormonal predictors of left ventricular function and prognosis after myocardial infarction. Circulation 1998971921–1929. [DOI] [PubMed] [Google Scholar]
- 11.Galvani M, Ottani F, Oltrona L.et al N‐terminal pro‐brain natriuretic peptide on admission has prognostic value across the whole spectrum of acute coronary syndromes. Circulation 2004110128–134. [DOI] [PubMed] [Google Scholar]
- 12.Mega J L, Morrow D A, De Lemos J A.et al B‐type natriuretic peptide at presentation and prognosis in patients with ST‐segment elevation myocardial infarction: an ENTIRE‐TIMI‐23 substudy. J Am Coll Cardiol 200444335–339. [DOI] [PubMed] [Google Scholar]
- 13. ASSENT‐2 Investigators. Single‐bolus tenecteplase compared with front‐loaded alteplase in acute myocardial infarction: the ASSENT‐2 double‐blind randomised trial, Assessment of the Safety and Efficacy of a New Thrombolytic Investigators. Lancet 1999354716–722. [DOI] [PubMed] [Google Scholar]
- 14.Wallentin L, Bergstrand L, Dellborg M.et al Low molecular weight heparin (dalteparin) compared to unfractionated heparin as an adjunct to rt‐PA (alteplase) for improvement of coronary artery patency in acute myocardial infarction: the ASSENT Plus study. Eur Heart J 200324897–908. [DOI] [PubMed] [Google Scholar]
- 15.Johnston N, Jernberg T, Lindahl B.et al Biochemical indicators of cardiac and renal function in a healthy elderly population. Clin Biochem 200437210–216. [DOI] [PubMed] [Google Scholar]
- 16.Giannitsis E, Lehrke S, Wiegand U K.et al Risk stratification in patients with inferior acute myocardial infarction treated by percutaneous coronary interventions: the role of admission troponin T. Circulation 20001022038–2044. [DOI] [PubMed] [Google Scholar]
- 17.European Society of Cardiology, American College of Cardiology Myocardial infarction redefined: a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. Eur Heart J 2000211502–1513. [DOI] [PubMed] [Google Scholar]
- 18.Austen W G, Edwards J E, Frye R L.et al A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation 197551(4 suppl)5–40. [DOI] [PubMed] [Google Scholar]
- 19.National Heart, Lung, and Blood Institute Coronary artery surgery study. A multicenter comparison of the effects of randomized medical and surgical treatment of mildly symptomatic patients with coronary artery disease, and a registry of consecutive patients undergoing coronary angiography. Circulation 198163I1–81. [PubMed] [Google Scholar]
- 20.Kesek M, Englund A, Jernberg T.et al The relation of QT dispersion and localized QT difference to coronary pathology in a population with unstable coronary artery disease. Ann Noninvasive Electrocardiol 2003822–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Arakawa N, Nakamura M, Aoki H.et al Plasma brain natriuretic peptide concentrations predict survival after acute myocardial infarction. J Am Coll Cardiol 1996271656–1661. [DOI] [PubMed] [Google Scholar]
- 22.Morita E, Yasue H, Yoshimura M.et al Increased plasma levels of brain natriuretic peptide in patients with acute myocardial infarction. Circulation 19938882–91. [DOI] [PubMed] [Google Scholar]
- 23.Inoue T, Sakuma M, Yaguchi I.et al Early recanalization and plasma brain natriuretic peptide as an indicator of left ventricular function after acute myocardial infarction. Am Heart J 2002143790–796. [DOI] [PubMed] [Google Scholar]
- 24.Jernberg T, Lindahl B, Siegbahn A.et al N‐terminal pro‐brain natriuretic peptide in relation to inflammation, myocardial necrosis, and the effect of an invasive strategy in unstable coronary artery disease. J Am Coll Cardiol 2003421909–1916. [DOI] [PubMed] [Google Scholar]
- 25.Van 't Hof A W, Liem A, de Boer M J.et al Clinical value of 12‐lead electrocardiogram after successful reperfusion therapy for acute myocardial infarction. Zwolle Myocardial Infarction Study Group. Lancet 1997350615–619. [DOI] [PubMed] [Google Scholar]
- 26.Martinez‐Rios M A, Rosas M, Gonzalez H.et al Comparison of reperfusion regimens with or without tirofiban in ST‐elevation acute myocardial infarction. Am J Cardiol 200493280–287. [DOI] [PubMed] [Google Scholar]
- 27.James S K, Lindahl B, Siegbahn A.et al N‐terminal pro‐brain natriuretic peptide and other risk markers for the separate prediction of mortality and subsequent myocardial infarction in patients with unstable coronary artery disease: a global utilization of strategies to open occluded arteries (GUSTO)‐IV substudy. Circulation 2003108275–281. [DOI] [PubMed] [Google Scholar]