Abstract
Objective
To assess the prognostic value of various conventional and novel echocardiographic indices in patients with chronic heart failure (CHF) caused by left ventricular (LV) systolic dysfunction.
Methods
185 patients with a mean (SD) age of 67 (11) years with CHF and LV ejection fraction < 45% despite optimal pharmacological treatment were prospectively enrolled. The patients underwent two dimensional echocardiography with tissue harmonic imaging to assess global LV systolic function and obtain volumetric data. Transmitral flow was assessed with conventional pulse wave Doppler. Systolic (Sm), early, and late diastolic mitral annular velocities were measured with the use of colour coded Doppler tissue imaging.
Results
During a median follow up of 32 months (range 24–38 months in survivors), 34 patients died and one underwent heart transplantation. Sm velocity (hazard ratio (HR) 0.648, 95% confidence interval (CI) 0.463 to 0.907, p = 0.011), diastolic arterial pressure (HR 0.965, 95% CI 0.938 to 0.993, p = 0.015), serum creatinine (HR 1.006, 95% CI 1.001 to 1.011, p = 0.023), LV ejection fraction (HR 0.945, 95% CI 0.899 to 0.992, p = 0.024), age (HR 1.035, 95% CI 1.000 to 1.071, p = 0.052), LV end systolic volume index (HR 1.009, 95% CI 0.999 to 1.019, p = 0.067), and restrictive pattern of transmitral flow (HR 0.543, 95% CI 0.278 to 1.061, p = 0.074) predicted the outcome of death or transplantation on univariate analysis. On multivariate analysis, only Sm velocity (HR 0.648, 95% CI 0.460 to 0.912, p = 0.013) and diastolic arterial pressure (HR 0.966, 95% CI 0.938 to 0.994, p = 0.016) emerged as independent predictors of outcome.
Conclusions
In patients with CHF and LV systolic dysfunction despite optimal pharmacological treatment, the strongest independent echocardiographic predictor of prognosis was Sm velocity measured with quantitative colour coded Doppler tissue imaging.
Keywords: congestive heart failure, left ventricular dysfunction, diastole, Doppler echocardiography, prognosis
Despite recent advances in management, chronic heart failure (CHF) is still associated with a high morbidity and mortality.1 Risk stratification can help gauge which patients are most in need of further treatment or who remain at high risk of future events, and who should therefore be considered for clinical trials of new interventions.
Both the European Society of Cardiology and American College of Cardiology/American Heart Association guidelines recommend the use of echocardiography as the preferred diagnostic imaging tool.2,3 Echocardiographic techniques provide the cardiologist with numerous indices reflecting left ventricular (LV) systolic and diastolic function and ventricular remodelling. Many of these indices have been shown to predict outcome in patients with CHF but, surprisingly, controversy exists around one of the most popular measures, LV ejection fraction (LVEF).4 Although LVEF measured by radionuclide ventriculography appears to be a consistent independent predictor of risk, this is less certain when LVEF is measured by echocardiography.5,6,7,8,9,10,11,12 The failure of echocardiographic LVEF to predict risk in some studies may reflect outmoded technology leading to poor quality data, the competing prognostic value of many other echocardiographic measurements that may eliminate LVEF on multivariate analysis, and differences in patient samples.
Recent advances in echocardiography, such as the introduction of contrast and of tissue harmonic imaging, have improved the accuracy and reproducibility of echocardiographic imaging and may enhance the value of LVEF measured by echocardiography for risk stratification in CHF.13 However, other echocardiographic techniques, such as Doppler tissue imaging (DTI), provide alternative, potentially more robust methods for risk stratification that are less dependent on the quality of images.
Few studies have addressed the prognostic importance of novel tissue Doppler derived indices of LV systolic and diastolic function.14,15,16 The objective of this study was to assess the prognostic value of a range of conventional and novel indices of LV systolic and diastolic function obtained with the use of two dimensional echocardiography with second harmonic imaging, conventional Doppler, and quantitative colour coded DTI in patients with CHF caused by LV systolic dysfunction. Our intention was to identify those echocardiographic variables that provide independent prognostic value in addition to basic clinical information such as age, sex, aetiology of CHF, New York Heart Association (NYHA) functional class, heart rate, blood pressure, serum sodium, and creatinine to generate a minimum prognostic dataset feasible for routine clinical use.
METHODS
Study participants
We prospectively enrolled 185 consecutive patients with a mean (SD) age of 67 (11) years (range 27–89 years) with clinical signs and symptoms of CHF. Exclusion criteria were preserved LV systolic function (LVEF ⩾ 45%), atrial fibrillation, recent myocardial infarction (during the previous six months), and significant primary valvar heart disease. The aetiology of LV dysfunction was ischaemic heart disease in 153 patients and non‐ischaemic cardiomyopathy in 32 patients. Informed consent was obtained from all study patients. The study complies with the Declaration of Helsinki and was approved by the local research ethics committee.
Echocardiography
The study participants underwent full echocardiographic examination with commercially available equipment (GE Vingmed Vivid Five, Horten, Norway) equipped with a 2.5 MHz phased array transducer. Images were recorded in the tissue harmonic imaging mode (coded octave harmonic imaging) with optimised gain settings.
LV end diastolic volume and end systolic volumes were calculated by the modified Simpson's rule,17 and the standard formula was applied to obtain LVEF. LV end diastolic volume and end systolic volume indices were obtained by correcting for body surface area.
Doppler echocardiography
Doppler studies were performed in the pulsed wave mode. Transmitral flow velocities were recorded from an apical four chamber view with the sample volume positioned at the tips of the mitral leaflets in diastole. Care was taken to obtain the smallest possible angle between the direction of transmitral flow and the ultrasound beam.
Peak velocity of the E wave, peak velocity of the A wave, deceleration time of early filling, and isovolumic relaxation time were measured from the transmitral Doppler spectrum. Deceleration time was calculated as the time between peak E wave and the upper deceleration slope extrapolated to the baseline and isovolumic relaxation time was measured as the interval between the aortic valve closure click and the beginning of the E wave by placing the sample volume between the anterior mitral leaflet and LV outflow tract. The E:A ratio was also calculated.
According to Doppler derived indices, patients were classified as having a restrictive (E:A ratio ⩾ 2 or 1 < E:A ratio < 2 with deceleration time ⩽ 140 ms) or non‐restrictive (E:A ratio ⩽ 1, or 1 < E:A ratio < 2 with deceleration time > 140 ms) pattern of LV diastolic filling.18
Doppler tissue imaging
Raw images were acquired with the use of real time two dimensional colour coded DTI in three apical views (four chamber, two chamber, and apical long axis views) and stored digitally on magnetic optical disks. A commercially available software package (Echopac 6.3, GE Vingmed) running on a Power Macintosh personal computer was used for offline analysis of the data.
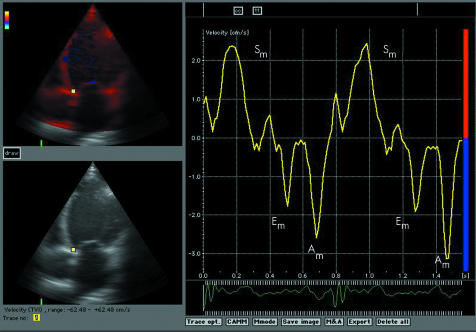
Longitudinal systolic mitral annular (Sm) velocity, as assessed during true ventricular systole ignoring peaks that are observed during isometric ventricular contraction or post‐systolic waves, and early (Em) and late diastolic mitral annular (Am) velocities were measured from six positions (at the lateral, septal, anterior, inferior, posterior, and anteroseptal sites of the mitral annulus) and averaged. The Em:Am ratio was then calculated. As an example, fig 1 illustrates a decoded trace from a study patient obtained with quantitative TDI at the septal site of the mitral annulus.
Figure 1 Example of the measurement of systolic (Sm), early diastolic (Em), and late diastolic mitral annular (Am) velocities at the septal site of the mitral annulus by colour coded tissue Doppler imaging. Note low mitral annular velocities suggestive of left ventricular dysfunction in a patient with chronic heart failure.
The echocardiographic study was performed by the same experienced investigator (NPN). All measurements were done as the mean of two or three consecutive cardiac cycles.
Clinical variables recorded
The following clinical variables were recorded and included in the prognostic model: age, sex, body mass index, systolic, diastolic, and pulse arterial pressures, heart rate, aetiology of CHF (ischaemic versus non‐ischaemic), NYHA functional class, serum sodium, and creatinine.
Statistical analysis
Results are presented as mean (SD) or as number (percentage) of patients.
Univariate Cox proportional hazards analysis was performed to assess the significance of various variables as predictors of cardiac death or transplantation. Variables predictive of the outcome (p < 0.1) were then entered into a multivariate Cox proportional hazards regression model (forward selection) to identify independent predictors of cardiac death or transplantation. The output from the Cox regression analysis is given as hazard ratios with 95% confidence intervals. Cumulative mortality curves were obtained by the Kaplan‐Meier method. SPSS software (version 12.0 for Windows; SPSS Inc, Chicago, Illinois, USA) was used for analysing data.
RESULTS
Table 1 shows baseline characteristics of the study patients. The majority of patients were men and had ischaemic heart disease. All the patients were in class II (n = 122) or III (n = 63) of the NYHA functional classification at the time of entry into the study. Before recruitment, patients were followed up for at least six months in a specialised heart failure clinic to ensure continued optimisation of pharmacological treatment. Most patients were taking β blockers (92%), of whom 72% were taking target doses. Every patient was taking either an angiotensin converting enzyme (ACE) inhibitor (84%) or an angiotensin receptor antagonist (16%), of whom 78% and 70%, respectively, were taking target doses. As for other heart failure medications, 84% of patients were taking diuretics, 35% were taking spironolactone, and 12% were taking digoxin.
Table 1 Clinical and echocardiographic characteristics of the study patients (n = 185).
| Age (years) | 67 (11) |
| Men | 146 (79%) |
| BMI (kg/m2) | 26.6 (4.1) |
| Systolic AP (mm Hg) | 133 (22) |
| Diastolic AP (mm Hg) | 81 (13) |
| Pulse AP (mm Hg) | 52 (17) |
| Heart rate (beats/min) | 71 (14) |
| Serum sodium (mmol/l) | 139 (3) |
| Serum creatinine (μmol/l) | 120 (44) |
| Ischaemic aetiology | 153 (83%) |
| EDV index (ml/m2) | 116 (37) |
| ESV index (ml/m2) | 76 (29) |
| Ejection fraction (%) | 35 (6) |
| Peak E (cm/s) | 81 (30) |
| Peak A (cm/s) | 71 (32) |
| E:A ratio | 1.62 (1.39) |
| IVRT (ms) | 93 (33) |
| DT (ms) | 183 (69) |
| Restrictive TMF pattern | 56 (30%) |
| Sm velocity (cm/s) | 2.9 (1.2) |
| Em velocity (cm/s) | 3.1 (1.5) |
| Am velocity (cm/s) | 4.0 (1.8) |
| Em:Am ratio | 1.0 (1.1) |
| E:Em ratio | 31 (18) |
Data are expressed as mean (SD) or as number (%) of patients.
A, velocity of atrial transmitral flow; Am, late diastolic mitral annular; AP, arterial pressure; BMI, body mass index; DT, deceleration time of early transmitral flow; E, velocity of early transmitral flow; EDV, end diastolic volume; Em, early diastolic mitral annular; ESV, end systolic volume; IVRT, isovolumic relaxation time; NYHA, New York Heart Association; Sm, systolic mitral annular; TMF, transmitral flow.
Thirty four patients died and one patient underwent cardiac transplantation during a median follow up of 32 months (range 3–38 months). All surviving patients were followed up for a minimum of 24 months (range 24–38 months). Table 2 shows the variables that predicted the combined outcome of death or cardiac transplantation on univariate Cox regression analysis (p < 0.1). Sm velocity, diastolic arterial pressure, serum creatinine, LVEF, age, LV end systolic volume index (corrected for body size), and a restrictive pattern of transmitral flow emerged as predictors of outcome in the study patients.
Table 2 Univariate and multivariate predictors of death and cardiac transplantation among patients with chronic heart failure.
| Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|
| HR (95% CI) | p Value | HR (95% CI) | p Value | |
| Sm velocity | 0.648 (0.463 to 0.907) | 0.011 | 0.648 (0.460 to 0.912) | 0.013 |
| Diastolic AP | 0.965 (0.938 to 0.993) | 0.015 | 0.966 (0.938 to 0.994) | 0.016 |
| Serum creatinine | 1.006 (1.001 to 1.011) | 0.023 | NA | NA |
| Ejection fraction | 0.945 (0.899 to 0.992) | 0.024 | NA | NA |
| Age | 1.035 (1.000 to 1.071) | 0.052 | NA | NA |
| ESV index | 1.009 (0.999 to 1.019) | 0.067 | NA | NA |
| Restrictive TMF pattern | 0.543 (0.278 to 1.061) | 0.074 | NA | NA |
CI, confidence interval; HR, hazard ratio; NA, not applicable.
Sex, body mass index, systolic and pulse arterial pressures, heart rate, NYHA functional class, aetiology of CHF, serum sodium, LV end diastolic volume index (corrected for body size), individual Doppler indices of transmitral flow (E, A, E:A ratio, isovolumic relaxation time, and deceleration time), diastolic mitral annular velocities (Em and Am velocities and their ratio Em:Am), and the E:Em ratio were not significantly associated with death and cardiac transplantation on univariate analysis in this study.
After all the variables that predicted the combined outcome of death or cardiac transplantation on univariate Cox regression analysis (p < 0.1) were entered into a forward multivariate Cox regression analysis, only Sm velocity and diastolic arterial pressure emerged as independent predictors of outcome in patients with CHF. Table 2 shows the final multivariate Cox model.
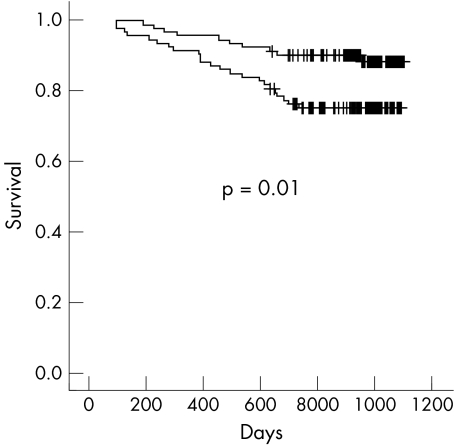
Two year mortality (including one case of cardiac transplantation) in the study patients was 18%. Figure 2 shows Kaplan‐Meier curves showing survival of the patients categorised according to Sm velocity of greater or less than 2.8 cm/s (median value).
Figure 2 Survival curves categorised according to Sm velocity greater (upper curve) or less (lower curve) than 2.8 cm/s (median value; p = 0.01). Vertical bars represent censored observations.
DISCUSSION
This analysis suggests that a great array of echocardiographic measures adds little to a single, relatively simple marker of cardiac function in patients with CHF caused by LV systolic dysfunction already receiving optimal medical treatment. To our knowledge, this is the first study showing that Sm velocity is a powerful predictor of outcome in patients with CHF caused by LV systolic dysfunction and is more strongly related to outcome than other echocardiography derived variables. It retains its prognostic value after adjustment for clinical data and other echocardiographic, conventional Doppler, and tissue Doppler indices. The interobserver and intraobserver variability of measurements of Sm velocity with the use of quantitative colour two dimensional DTI is within 4–8%, which compares favourably with assessment of LVEF.19,20 The technique is now widely available on echocardiographic equipment of various manufacturers. The prognostic value of Sm velocity now requires replication in other cohorts and by other investigators.
Several previous studies with echocardiographic imaging have suggested that LVEF and LV volumes indices, which were probably measured less accurately in some studies before the era of harmonic imaging, were strong predictors of outcome in the setting of CHF and after myocardial infarction.7,8,9,21 However, other studies failed to show that these measures had independent predictive value even in relatively large cohorts of patients.10,11,12 Univariate analysis of our data supports the observation that echocardiographic LVEF and volumetric data have prognostic value but are inferior to a tissue Doppler derived index of LV systolic function (Sm velocity), which eliminated these conventional indices from a multivariate model.
Differences in predictive variables between studies may reflect differences in study samples, which variables were entered into the prognostic model, and the accuracy of measurements, such as LV volumes, and their derivatives, such as LVEF. Importantly, changes in echocardiographic technology will have improved the accuracy of some measurements and added new variables. New technology is often rapidly adopted into clinical practice but this often leads to new measurements being added to rather than replacing traditional ones. While this may often be appropriate, it is not always so. Research should seek to rationalise clinical practice to identify the smallest amount of useful information and not just increase the number of things that can be measured.
Measures of LV diastolic filling obtained with the use of conventional Doppler have also been shown to be of prognostic significance. The restrictive pattern of transmitral flow was associated with an adverse prognosis in patients with dilated cardiomyopathy and CHF caused by LV systolic dysfunction.18,22 However, the use of conventional Doppler indices of transmitral flow is associated with well recognised limitations. The pattern of transmitral flow is dependent on loading conditions, interpretation of the Doppler spectrum in the presence of severe mitral regurgitation is difficult, and measurements of the Doppler spectrum of pulmonary venous flow to improve interpretation are often difficult to obtain by using the transthoracic approach. The restrictive pattern of transmitral flow, a predictor of outcome on univariate analysis in this study, was eliminated on multivariate analysis.
DTI is a relatively new echocardiographic technique, which enables measurement of atrioventricular annular and segmental myocardial velocities. Several DTI modes including pulsed wave DTI, colour M mode DTI, and colour two dimensional DTI are available. DTI is less dependent on the quality of echocardiographic images and does not require tracing of endocardial contours, unlike LV volumes and LVEF. The technique can also overcome some limitations of conventional Doppler studies (dependence on loading conditions).23 The assessment of mitral annular motion has been recognised as an accurate method to quantify both systolic and diastolic longitudinal LV function.23,24,25,26 Normal values obtained with the use of pulsed wave DTI and colour coded two dimensional DTI have been reported.19,27
Although not directly comparable, this study lends support to a few previous reports on prognostic significance of quantitative tissue Doppler indices reported in other cohorts of cardiac patients. Wang et al16 showed, in a group of patients with a variety of cardiac diseases, that both Sm and Em velocities were predictors of cardiac mortality on univariate analysis but that Em velocity was marginally superior on multivariate analysis. In patients with LV dysfunction resulting from various causes, Yamamoto et al15 found that Am velocity (assessed as a single measurement at the posterior wall site of the mitral annulus) and Em velocity in combination with mitral peak E wave velocity (E:Em ratio) were the strongest predictors of cardiac mortality. However, Sm velocity was not included in the analysis. Møller et al14 studied a group of patients after first myocardial infarction and reported that the E:Em ratio was an independent predictor of death or readmission to the hospital as the result of worsening of CHF. However, mitral annular velocities were measured at only one site (at the lateral site of the mitral annulus with the use of pulsed wave DTI) and no measurements of Sm velocity were reported.
Although most of the above studies focused on diastolic measurements, it should be noted that there is a significant correlation between Sm and diastolic mitral annular velocities (both Em and Am) due to the close physiological interaction between systolic shortening and diastolic lengthening. The descent of the mitral annulus from its equilibrium position leads to storage and subsequent release of potential energy in a reciprocal fashion between atrium and ventricle.28
Low diastolic arterial pressure was another important predictor of outcome in this study. The prognostic significance of arterial pressure in patients with CHF has been previously reported.29,30 Arterial pulse pressure, which was found to be of additional value in one study on post‐infarction patients, did not emerge as a predictor of outcome in this study.29
Limitations
These data should be extrapolated to other groups of patients with care. It is not clear what effect chronic treatment with ACE inhibitors and β blockers has on the predictive accuracy of most variables and so our data should not be extrapolated to ACE inhibitor or β blocker naive patients. We did not adjust for the known age related decrease in Sm velocity, although we included age in the multivariate model, which can affect its predictive capacity.19
Despite optimal pharmacological treatment, two year mortality in this study was 18%. It is higher than rates suggested by large clinical trials. Several potential explanations exist for this discrepancy. Our patients were older and had more co‐morbidity that would have excluded many from clinical trials. Our group of patients also had a higher prevalence of ischaemic heart disease, which is associated with a worse outcome.4
Mitral annular velocities in this study were measured by two dimensional colour coded tissue DTI and are lower than velocities measured with pulsed wave DTI. Further studies are required to elucidate whether the two techniques provide data of similar prognostic importance. However, we believe that colour coded DTI is a more advanced method and has emerged as the leading method of investigating mitral annular motion.
Conclusion
In patients with CHF and LV systolic dysfunction despite optimal pharmacological treatment, the strongest independent echocardiographic predictor of prognosis was Sm velocity measured with quantitative colour coded DTI, a simple measure of LV systolic function.
ACKNOWLEDGEMENTS
We thank the team of physicians and nurses in the Academic Unit of Cardiology in Hull for assistance with conducting the study, Elena Lukaschuk for research assistance, and Elaine Allison and Hanka Remblence for secretarial support.
Abbreviations
ACE - angiotensin converting enzyme
Am - late diastolic mitral annular
CHF - chronic heart failure
DTI - Doppler tissue imaging
Em - early diastolic mitral annular
LV - left ventricular
LVEF - left ventricular ejection fraction
NYHA - New York Heart Association
Sm - systolic mitral annular
Footnotes
Competing interest statement: There are no competing interests to report
Ethics approval: Informed consent was obtained from all study patients. The study complies with the Declaration of Helsinki and was approved by the local (Hull and East Riding) research ethics committee.
References
- 1.Cleland J G F, Clark A. Has the survival of the heart failure population changed? Lessons from trials. Am J Cardiol 199983112–119. [DOI] [PubMed] [Google Scholar]
- 2.Remme W J, Swedberg K, Cleland J G F.et al Guidelines for the diagnosis and treatment of chronic heart failure (task force report). Eur Heart J 2001221527–1560. [DOI] [PubMed] [Google Scholar]
- 3.Hunt S A, Baker D W, Chin M H.et al ACC/AHA guidelines for the evaluation and management of chronic heart failure in the adult: executive summary. A report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation 20011042996–3007. [DOI] [PubMed] [Google Scholar]
- 4.Cowburn P J, Cleland J G, Coats A J.et al Risk stratification in chronic heart failure. Eur Heart J 199819696–710. [DOI] [PubMed] [Google Scholar]
- 5.Parameshwar J, Keegan J, Sparrow J. Predictors of prognosis in severe chronic heart failure. Am Heart J 1992123421–426. [DOI] [PubMed] [Google Scholar]
- 6.Madsen B K, Hansen J F, Stokholm K H.et al Chronic congestive heart failure: description and survival of 190 consecutive patients with a diagnosis of chronic congestive heart failure based on clinical signs and symptoms. Eur Heart J 199415303–310. [DOI] [PubMed] [Google Scholar]
- 7.Cintron G, Johnson G, Francis G.et al Prognostic significance of serial changes in left ventricular ejection fraction in patients with congestive heart failure. The V‐HeFT VA Cooperative Studies Group. Circulation 199387(suppl 6)VI17–VI23. [PubMed] [Google Scholar]
- 8.Gustafsson F, Torp‐Pedersen C, Brendorp B, for the DIAMOND study group et al Long‐term survival in patients hospitalized with congestive heart failure: relation to preserved and reduced left ventricular systolic function. Eur Heart J 200324863–870. [DOI] [PubMed] [Google Scholar]
- 9.Juilliere Y, Barbier G, Feldman A.et al Additional predictive value of both left and right ventricular ejection fractions on long‐term survival in idiopathic dilated cardiomyopathy. Eur Heart J 199718276–280. [DOI] [PubMed] [Google Scholar]
- 10.McDermott M M, Feinglass J, Lee P I.et al Systolic function, readmission rates, and survival among consecutively hospitalized patients with congestive heart failure. Am Heart J 1997134728–736. [DOI] [PubMed] [Google Scholar]
- 11.Pernenkil R, Vinson J M, Shah A S.et al Course and prognosis in patients > or = 70 years of age with congestive heart failure and normal versus abnormal left ventricular ejection fraction. Am J Cardiol 199779216–219. [DOI] [PubMed] [Google Scholar]
- 12.Saxon L A, Stevenson W G, Middlekauff H R.et al Predicting death from progressive heart failure secondary to ischemic or idiopathic dilated cardiomyopathy. Am J Cardiol 19937262–65. [DOI] [PubMed] [Google Scholar]
- 13.Senior R, Soman P, Khattar R S.et al Improved endocardial visualization with second harmonic imaging compared with fundamental two‐dimensional echocardiographic imaging. Am Heart J 1999138163–168. [DOI] [PubMed] [Google Scholar]
- 14.Møller J E, Sondergaard E, Poulsen S H.et al Color M‐mode and pulsed wave tissue Doppler echocardiography: powerful predictors of cardiac events after first myocardial infarction. J Am Soc Echocardiogr 200114757–763. [DOI] [PubMed] [Google Scholar]
- 15.Yamamoto T, Oki T, Yamada H.et al Prognostic value of the atrial systolic mitral annular motion velocity in patients with left ventricular systolic dysfunction. J Am Soc Echocardiogr 200316333–339. [DOI] [PubMed] [Google Scholar]
- 16.Wang M, Yip G W, Wang A Y.et al Peak early diastolic mitral annulus velocity by tissue Doppler imaging adds independent and incremental prognostic value. J Am Coll Cardiol 200341820–826. [DOI] [PubMed] [Google Scholar]
- 17.Schiller N B, Shah P M, Crawford M.et al Recommendations for quantitation of the left ventricle by two‐dimensional echocardiography. J Am Soc Echocardiogr 19892358–367. [DOI] [PubMed] [Google Scholar]
- 18.Xie G Y, Berk M R, Smith M D.et al Prognostic value of Doppler transmitral flow patterns in patients with congestive heart failure. J Am Coll Cardiol 199424132–139. [DOI] [PubMed] [Google Scholar]
- 19.Nikitin N P, Witte K K, Thackray S D.et al Longitudinal ventricular function: normal values of atrioventricular annular and myocardial velocities measured with quantitative two‐dimensional color Doppler tissue imaging. J Am Soc Echocardiogr 200316906–921. [DOI] [PubMed] [Google Scholar]
- 20.McGowan J H, Cleland J G F. Reliability of reporting left ventricular systolic function by echocardiography: a systematic review of 3 methods. Am Heart J 2003146388–397. [DOI] [PubMed] [Google Scholar]
- 21.White H D, Norris R M, Brown M A.et al Left ventricular end‐systolic volume as the major determinant of survival after recovery from myocardial infarction. Circulation 19877644–51. [DOI] [PubMed] [Google Scholar]
- 22.Pinamonti B, Di Lenarda A, Sinagra G.et al Restrictive left ventricular filling pattern in dilated cardiomyopathy assessed by Doppler echocardiography: clinical, echocardiographic and hemodynamic correlations and prognostic implications. J Am Coll Cardiol 199322808–815. [DOI] [PubMed] [Google Scholar]
- 23.Sohn D W, Chai I H, Lee D J.et al Assessment of mitral annulus velocity by Doppler tissue imaging in the evaluation of left ventricular diastolic function. J Am Coll Cardiol 199730474–480. [DOI] [PubMed] [Google Scholar]
- 24.Gulati V K, Katz W E, Follansbee W P.et al Mitral annular descent velocity by tissue Doppler echocardiography as an index of global left ventricular function. Am J Cardiol 199677979–984. [DOI] [PubMed] [Google Scholar]
- 25.Alam M, Wardell J, Andersson E.et al Assessment of left ventricular function using mitral annular velocities in patients with congestive heart failure with or without the presence of significant mitral regurgitation. J Am Soc Echocardiogr 200316240–245. [DOI] [PubMed] [Google Scholar]
- 26.Farias C A, Rodriguez L, Garcia M J.et al Assessment of diastolic function by tissue Doppler echocardiography: comparison with standard transmitral and pulmonary venous flow. J Am Soc Echocardiogr 199912609–617. [DOI] [PubMed] [Google Scholar]
- 27.Pai R G, Gill K S. Amplitudes, durations, and timings of apically directed left ventricular myocardial velocities. I. Their normal pattern and coupling to ventricular filling and ejection. J Am Soc Echocardiogr 199811105–111. [DOI] [PubMed] [Google Scholar]
- 28.Carr‐White G S, Koh T W, Haxby E.et al Mitral annular energetics as determinants of left ventricular filling: quantification of atrioventricular interactions. Eur Heart J Suppl 20002(suppl K)K61–K68. [Google Scholar]
- 29.Mitchell G F, Moyé L A, Braunwald E.et al Sphygmomanometrically determined pulse pressure is a powerful independent predictor of recurrent events after myocardial infarction in patients with impaired left ventricular function. Circulation 1997964254–4260. [DOI] [PubMed] [Google Scholar]
- 30.Campana C, Gavazzi A, Berzuini C.et al Predictors of prognosis in patients awaiting heart transplantation. J Heart Lung Transpl 199312756–765. [PubMed] [Google Scholar]