In recent years biomarkers have emerged as important tools for diagnosis, risk stratification and therapeutic decision making in cardiovascular diseases. Cardiac troponins in particular have become the cornerstone for diagnostic work up of patients with acute coronary syndromes. Currently, several promising new biomarkers are under scientific investigation. Most of these new biomarkers, however, are not yet suitable for clinical application, with the exception of B‐type natriuretic peptide (BNP) and its N‐terminal fragment (NT‐proBNP). Both markers have proven their diagnostic usefulness in a great number of studies and thus have progressed from bench to clinical application. This article aims to summarise existing data concerning BNP and NT‐proBNP measurement in cardiovascular disorders and to outline how these markers can be integrated into clinical routine. Furthermore, future perspectives of these markers will be discussed.
PHYSIOLOGY
B‐type natriuretic peptide, which is also called brain‐type natriuretic peptide (BNP), was first described in 1988 after isolation from porcine brain. However, it was soon found to originate mainly from the heart, representing a cardiac hormone.
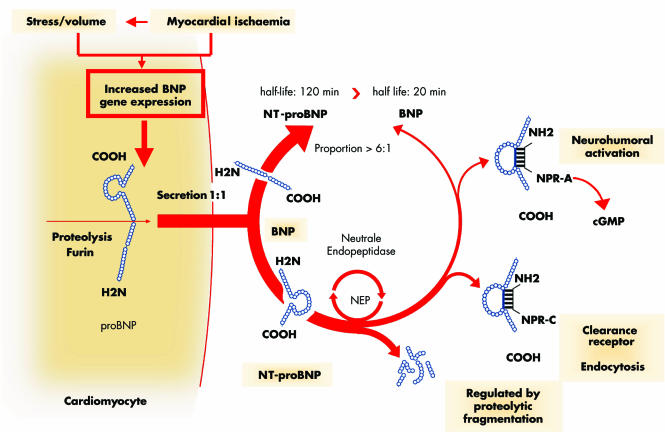
BNP belongs to the natriuretic peptide family together with other structurally similar peptides, namely atrial natriuretic peptide (ANP), C‐type natriuretic peptide (CNP), and urodilatin. The natriuretic peptides have in common a characteristic biochemical structure which consists of a 17 amino‐acid ring and a disulfide bridge between two cysteine molecules. The major source of BNP synthesis and secretion is the ventricular myocardium. Whereas ANP is stored in granules and can be released immediately after stimulation, only small amounts of BNP are stored in granules and rapid gene expression with de novo synthesis of the peptide is the underlying mechanism for the regulation of BNP secretion. BNP is synthesised as a prehormone (proBNP) comprising 108 amino acids. Upon release into the circulation it is cleaved in equal proportions into the biologically active 32 amino acid BNP, which represents the C‐terminal fragment, and the biologically inactive 76 amino acid N‐terminal fragment (NT‐proBNP).
Both molecules are constantly released and can be detected in the blood. The main stimulus for increased BNP and NT‐proBNP synthesis and secretion is myocardial wall stress. Furthermore, factors such as myocardial ischaemia and endocrine (paracrine) modulation by other neurohormones and cytokines are also of importance.
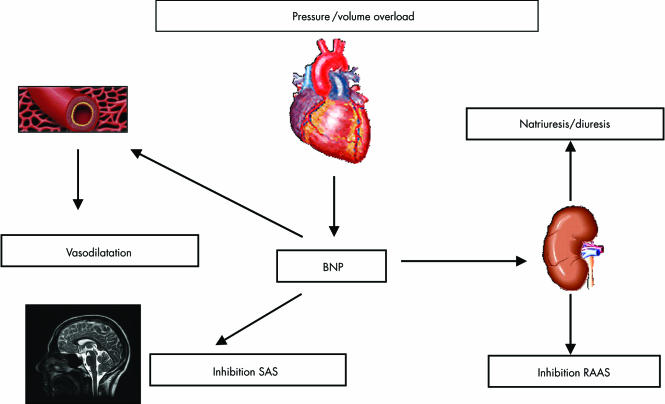
In the systemic circulation BNP mediates a variety of biological effects by interaction with the natriuretic peptide receptor type A (NPR‐A) causing intracellular cGMP production. The physiological effects of BNP are manifold and comprise natriuresis/diuresis, peripheral vasodilatation, and inhibition of the renin–angiotensin–aldosterone system (RAAS) and the sympathetic nervous system (SNS). BNP is cleared from plasma by binding to the natriuretic peptide receptor type C (NPR‐C) and through proteolysis by neutral endopeptidases. In contrast, NT‐proBNP is mainly cleared by renal excretion. However, recent studies suggest that there might also be other important clearing mechanisms for NT‐proBNP. The half‐life of BNP is 20 mins whereas NT‐proBNP has a half‐life of 120 mins, which explains why NT‐proBNP serum values are approximately six times higher than BNP values, even though both molecules are released in equimolar proportions (figs 1 and 2).1
Figure 1 Schematic illustration of B‐type natriuretic peptide (BNP) and NT‐proBNP synthesis, release and receptor interaction. BNP is synthesised as prohormone in the cardiomyocytes. Upon release into the circulation proBNP is cleaved into BNP and the N‐terminal fragment (NT‐proBNP) in equimolar proportions. Interaction of BNP and the natriuretic peptide receptor type A (NPR‐A) mediates the biological effects via intracellular cGMP increase. Reproduced with permission from E Spannuth.
Figure 2 Physiological effects of B‐type natriuretic peptide (BNP). Volume or pressure overload leads to ventricular wall stress and BNP release. The systemic biological effects of BNP are peripheral vasodilatation, increase in natriuresis and diuresis, and inhibition of the sympathetic nervous system (SNS) and the renin–angiotensin–aldosterone system (RAAS).
ANALYTIC CONSIDERATIONS
Both BNP and NT‐proBNP can be measured by fully automated and commercially available assays (AxSYM BNP, Abbot; ADVIA centaur BNP, Bayer; Elecsys NT‐proBNP, Roche Diagnostics), which have proven excellent test precision. Reliable point of care tests are also available for both markers (Triage BNP, Biosite; Cardiac Reader NT‐proBNP, Roche Diagnostics). BNP and NT‐proBNP plasma concentrations are expressed in pg/ml or pmol/l. The conversion factor for BNP is 1 pg/ml = 0.289 pmol/l, and for NT‐proBNP it is 1 pg/ml = 0.118 pmol/l. BNP values obtained with various assays are not comparable and there is no conversion factor for the comparison of BNP and NT‐proBNP values.
BNP is stable in whole blood at room temperature with the addition of EDTA for at least 24 h, whereas NT‐proBNP is stable for at least 72 h in whole blood at room temperature and requires no additives. Both BNP and NT‐proBNP are stable during freeze and thaw processes.
There are several determinants for BNP and NT‐proBNP concentrations. It has been shown consistently in several studies that BNP and NT‐proBNP are related to sex, with higher values in females, and to age, with higher values in older individuals. The sex relation is thought to be caused by differences in metabolism, whereas the association with age might reflect preclinical structural and functional myocardial alterations not detectable by current techniques.2
In patients with reduced renal function, BNP and NT‐proBNP values are increased with a negative correlation to creatinine clearance. NT‐proBNP seems to be affected more by worsening renal function than BNP. Besides diminished renal clearance, higher prevalence of concomitant left ventricular alterations such as left ventricular hypertrophy, diastolic and systolic dysfunction as well as fluid overload might contribute to elevated BNP and NT‐proBNP concentrations. However, recent results of a head to head comparison of both markers in patients with renal disease indicate similar diagnostic performance of both markers.3
CLINICAL APPLICATIONS
Heart failure
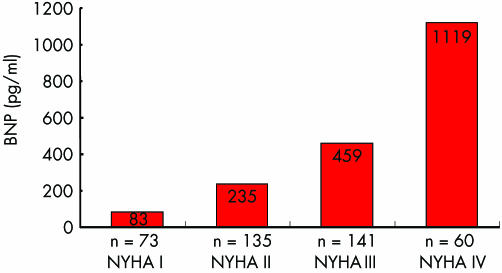
The diagnostic value of BNP and NT‐proBNP is best investigated in patients with heart failure. In a large number of studies it has been consistently found that BNP and NT‐proBNP are elevated in patients with heart failure, and values were found to be related to disease severity as assessed by New York Heart Association (NYHA) functional class (fig 3), left ventricular systolic ejection fraction, and left ventricular diastolic function.1
Figure 3 Median B‐type natriuretic peptide (BNP) in patients with heart failure according to New York Heart Association (NYHA) functional status. Adapted from Wieczorek et al.6
Emergency room setting
In the Breath Not Properly (BNP) trial 1586 patients presenting to the emergency department with shortness of breath were investigated. The main finding of this study was that BNP testing provided high test accuracy for the detection of heart failure, being superior to clinical judgement. At a cut‐off value of 100 pg/ml BNP had a very high negative predictive value, thus making it especially applicable as a rule‐out test for heart failure in this setting.4 Similar results were obtained in the N‐terminal proBNP Investigation of Dyspnoea in the Emergency department (PRIDE)5 study and in the International Collaboration of NT‐proBNP (ICON), in which the diagnostic role of NT‐proBNP in patients presenting with the cardinal symptom of shortness of breath has been established. In these studies, a cut‐off value for NT‐proBNP of 300 pg/ml to exclude heart failure has been determined. Several further studies which evaluated the diagnostic performance of BNP and NT‐proBNP demonstrated similar results of a high negative predictive value at the respective thresholds (table 1).6 Thus, the particular strength of these markers is their ability to rule out the diagnosis of heart failure. In general, heart failure is unlikely at BNP values < 100 pg/ml and is very likely at BNP values > 500 pg/ml and, similarly, unlikely at NT‐proBNP values < 300 pg/ml and very likely at NT‐proBNP values > 450 pg/ml (> 900 pg/ml in patients above 50 years of age) (table 2).
Table 1 Trials evaluating the diagnostic performance of B‐type natriuretic peptide (BNP) and NT‐proBNP.
| Studies | n | Diagnosis of HF | Analyse | Cut‐off | Sens (%) | Spec (%) | PPV (%) | NPV (%) | AUC |
|---|---|---|---|---|---|---|---|---|---|
| McCullough 2002 BNP | 1538 | Clinical | BNP | 100 pg/ml | 90 | 73 | 75 | 90 | 0.90 |
| Wieczorek 2002 | 1050 | Clinical | BNP | 100 pg/ml | 82 | 97 | 0.93 | ||
| Januzzi 2005 PRIDE | 599 | Clinical | NT‐proBNP | 300 pg/ml | 99 | 68 | 62 | 99 | 0.94 |
| Januzzi 2005 ICON | 1256 | Clinical | NT‐proBNP | 300 pg/ml | 99 | 60 | 77 | 98 | 0.83–0.99 |
| Bay 2003 | 2193 | EF <40% | NT‐BNP | 357 pmol/l | 73 | 82 | 24 | 98 | 0.85 |
EF, ejection fraction; HF, heart failure; NPV, negative predictive value; PPV, positive predictive value; Sens, sensitivity; Spec, specificity.
Table 2 Cut‐off values for BNP (derived from the BNP study4) and for NT‐proBNP (derived from the PRIDE and ICON study5) for the diagnosis of heart failure of patients presenting with dyspnoea.
| Rule‐out | Rule‐in | |
|---|---|---|
| HF unlikely | HF likely | |
| BNP (pg/ml) | 100 | 500 |
| NT‐proBNP (pg/ml), age <50 years | 300 | 450 |
| NT‐proBNP (pg/ml), age >50 years | 300 | 900 |
In the B‐Type Natriuretic Peptide for Acute Shortness of Breath Evaluation (BASEL) study 452 patients presenting to the emergency department with acute dyspnoea were included. They were randomised for a clinically guided diagnostic strategy or for a strategy which integrated rapid BNP measurement. If BNP was below 100 mg/ml, clinicians were advised that heart failure was unlikely, and if BNP was above 500 mg/ml they were advised that heart failure was likely to be the origin of the dyspnoea. As demonstrated in this trial, measurement of BNP applying the above mentioned threshold in conjunction with other clinical information reduced hospitalisation rate, the need for intensive care, and total treatment time, and significantly reduced total treatment cost. However, clinical outcome over 30 days was equal in both study arms (table 3).7
Table 3 Results of the BASEL (B‐Type Natriuretic Peptide for Acute Shortness of Breath Evaluation) study.
| BNP group n = 225 | Control group n = 227 | p Value | |
|---|---|---|---|
| Time to treatment (mins) | 63 (16–153) | 90 (20–205) | 0.03 |
| Time to discharge (days) | 8 (1–16) | 11 (5–18) | 0.001 |
| Hospitalisation rate (%) | 75 | 85 | 0.008 |
| Admission to intensive care (%) | 15 | 24 | 0.01 |
| Total treatment costs (US$) | 5410 | 7264 | 0.006 |
| In‐hospital mortality (%) | 6 | 9 | 0.21 |
| 30‐day mortality (%) | 10 | 12 | 0.45 |
| 30‐day readmission rate (%) | 12 | 10 | 0.63 |
Values are expressed as median and interquartile range in parenthesis, or as percentage.
Prognostic value of BNP and NT‐proBNP
Independent of their diagnostic value, several large scale studies have convincingly shown that BNP and NT‐proBNP provide strong prognostic information for an unfavourable outcome (death, cardiovascular death, readmission or cardiac events) in patients with heart failure or asymptomatic left ventricular dysfunction.8 In multivariable models BNP and NT‐proBNP proved to be superior to other prognostic parameters and in some studies even to be the only independent prognostic factor. Head to head studies comparing the diagnostic performance of BNP and NT‐proBNP testing have been performed in patients with heart failure and in patients with asymptomatic left ventricular dysfunction. They revealed that both markers performed equally well with almost identical areas under the curve (AUC) of the receiver operating characteristic (ROC) curves.9 Thus, it can be concluded from those studies that there is no meaningful difference for risk stratification in clinical routine between the two markers.
Guiding and monitoring heart failure treatment
Even though there is a large body of evidence demonstrating the association of elevated BNP or NT‐proBNP values with disease severity and prognosis in heart failure patients, there are limited data available which focus on the therapeutic implications derived from BNP and NT‐proBNP assessment.
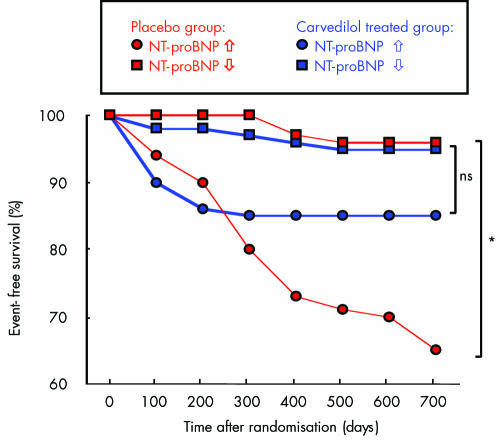
It has been reported that BNP and NT‐proBNP can be attenuated by treatment with drugs such as angiotensin receptor blockers or β blockers. Furthermore, several studies have been able to demonstrate changes of BNP and NT‐proBNP values during recompensation therapy in acute heart failure related to an improvement in invasively measured haemodynamic parameters.10 Subsequently, it was also shown that a decrease in BNP during the initial hospital stay was associated with a favourable clinical outcome, whereas no change or an increase in BNP values was associated with an unfavourable outcome.11 In a small pilot study by Troughton et al involving 79 patients with clinically overt heart failure and an ejection fraction below 40%, patients were randomly assigned either to clinically guided therapy or a combination of clinical parameters and BNP measurement to guide therapy. The event‐free survival rate over 180 days was significantly lower in the BNP guided group.12 In another study, a substudy of the Australia‐New Zealand heart failure trial, 297 patients with ischaemic heart disease and an ejection fraction below 45% were randomised to placebo or carvedilol treatment. Patients with NT‐proBNP values on admission above the median had a significant risk reduction if they were treated with carvedilol, whereas in the group of patients with BNP values below the median, the clinical outcome was identical for both the carvedilol and placebo treatment groups. This suggests that NT‐proBNP might help to identify those heart failure patients who derive benefit from active treatment with carvedilol (fig 4).13 These results are in contrast to the COPERNICUS trial, which enrolled 2289 patients with severe chronic heart failure (NYHA class III or IV) and an ejection fraction below 25%. The overall one year mortality of 14.9% in this study was extremely high and it was found that patients receiving active treatment with carvedilol had a better outcome than placebo treated patients. In a substudy of this trial including 1011 European patients, NT‐proBNP values were obtained at study entry. Even though NT‐proBNP was highly predictive for an unfavourable outcome in those patients, the treatment effect of carvedilol did not differ between patients with high NT‐proBNP values (above the median) and those with low NT‐proBNP values.14 Therefore, the data from these studies are promising and suggest that BNP and NT‐proBNP might be clinically useful for determining the optimal treatment for patients with heart failure and for monitoring treatment effects. The results of ongoing larger prospective trials, however, are awaited before definite conclusions can be reached.
Figure 4 Kaplan–Meier curves for event‐free survival of patients with ischaemic left ventricular dysfunction treated with carvedilol (blue line) or placebo (red line), with NT‐proBNP below the median (circles) and NT‐proBNP above the median (squares). ns, not significant; *p < 0.001. Modified from Richards et al.13
Coronary artery disease
Originally BNP and NT‐proBNP were considered biomarkers for heart failure only. More recently, however, there has been a growing body of data on the relevance of both markers in coronary artery disease. It is widely believed that the underlying pathophysiological process for an increase in BNP and NT‐proBNP values is left ventricular systolic or diastolic dysfunction caused by myocardial ischaemia leading to an increased wall stress. Nevertheless, data derived from experimental studies suggest a direct release of BNP and NT‐proBNP from cardiomyocytes in response to myocardial ischaemia independent of ventricular wall stress. It has also been demonstrated that BNP even rises after temporary myocardial ischaemia induced by balloon inflation during coronary intervention.
Acute coronary syndromes (ACS)
Substudies of large scaled clinical trials (OPUS‐TIMI 16, TACTICS‐TIMI 18, FRISC II, GUSTO IV, PRISM)15,16 have evaluated the prognostic value of BNP and NT‐proBNP in patients presenting with non‐ST elevation acute coronary syndromes (NSTE‐ACS). In all studies elevated values of BNP and NT‐proBNP have consistently been found. Furthermore, both markers were highly predictive for an adverse outcome independently of other biomarkers, especially troponins and C reactive protein (CRP). However, it must be emphasised that BNP and NT‐proBNP were predictive for mortality and heart failure after an ACS but not for recurrent ischaemic events. Similar results were reported for the predictive value of BNP and NT‐proBNP after ST elevation myocardial infarction (STEMI).17 Different studies evaluated whether serial assessment of NT‐proBNP is superior to a one time point assessment at admission. Jernberg et al studied 755 patients with an ACS and observed no difference in the predictive value as indicated by the AUC of the ROC curve for NT‐proBNP on admission and after 6 h.15 In a substudy of the PRISM trial Heeschen et al demonstrated an incremental prognostic value of serial NT‐proBNP assessment on admission and a second measurement 72 h later. In the FRISC‐II trial serial NT‐proBNP analyses were evaluated during the acute and the chronic phase of ACS and disclosed that the predictive value of NT‐proBNP value measured three and six months after the index event is a better predictor for two year mortality than early NT‐proBNP determination at admission or at 48 h after the acute event. However, the best time to take a sample for BNP or NT‐proBNP assessment still remains to be fully established.
In addition, the therapeutic benefits that can be derived from BNP and NT‐proBNP assessment in ACS are not clear. The only published study to date which investigated the usefulness of NT‐proBNP for identifying patients who might benefit from an early invasive strategy is a substudy of the FRISC‐II trial. In this study a trend towards a better outcome of patients with NT‐proBNP values in the highest tertile was observed. However, in combination with elevated interleukin (IL)‐6 concentrations, NT‐proBNP values in the third tertile indicated a significant treatment benefit from early invasive therapy.18 In the substudy of the PRISM trial, Heeschen et al analysed the effect of glycoprotein IIb/IIIa inhibition with tirofiban with respect to NT‐proBNP values.16 Even though they found that patients with high NT‐proBNP values had a lower event rate with tirofiban treatment compared to placebo at 48 h, they found no significant interaction between NT‐proBNP values and the clinical benefit of tirofiban treatment at 30 days.
Several matters need to be addressed before BNP and NT‐proBNP can be recommended for application in clinical routine in patients with ACS. Different cut‐off values have been applied in the various studies, but to date no clearly defined cut‐off value has been established. Moreover, further studies are needed to assess the therapeutic benefits that can be derived from BNP and NT‐proBNP assessment.
Stable coronary artery disease
Recent studies have evaluated the relevance of BNP and NT‐proBNP in patients with stable angina pectoris. It could be demonstrated that NT‐proBNP serum concentrations show a close relation to the extent of coronary artery disease and inducible myocardial ischaemia.19,20 Furthermore, three independent studies have indicated that BNP and NT‐proBNP provide prognostic information on long term mortality and adverse cardiovascular events superior to that provided by traditional risk factors.21 However, no cut‐off values are clearly defined and therapeutic consequences remain open.
Valvular heart disease
Valvular heart diseases lead to either volume or pressure overload of the left ventricle. Thus it is reasonable to expect that BNP and NT‐proBNP could be useful in evaluating the severity and prognosis of valve diseases. However, data are sparse. For patients with valvular aortic stenosis it has been shown in several small studies that both BNP and NT‐proBNP are related to disease severity, functional status and disease progression, with a decline of elevated values after successful valve replacement. Furthermore, the values provide prognostic information for an unfavourable postoperative outcome.22,23,24 The therapeutic implications of these findings are uncertain, but it can be speculated that BNP or NT‐proBNP assessment might help to decide upon the optimal timing for valve surgery. Data on the diagnostic utility of BNP and NT‐proBNP in patients with aortic regurgitation and mitral regurgitation are very limited, demonstrating that both markers are elevated in relation to disease severity. However, there are no data available concerning the prognostic value. Generally, there is good evidence that BNP and NT‐proBNP assessment might play a role in the future diagnostic work up of patients with valvular heart diseases, but the clinical benefits that can be derived have not yet been established. Thus, further studies are warranted.
Future perspectives
Several large studies which aimed to evaluate the usefulness of BNP or NT‐proBNP for population screening demonstrated a predictive value of both markers for death or the existence of cardiovascular diseases. However, BNP and NT‐proBNP population screening is generally not advised. Nevertheless, it seems reasonable to use BNP and NT‐proBNP for screening and risk assessment of well defined risk groups—for example, cardiovascular patients scheduled to undergo non‐cardiac surgery, patients to be treated with COX‐2 inhibitors, or patients with malignant disease being treated with cardiotoxic chemotherapeutic agents. Studies are in progress for these indications.
In a variety of small studies it has been found that BNP and NT‐proBNP values are elevated in patients with atrial fibrillation, even in the absence of structural heart disease, and that they are predictive of successful cardioversion. To date no threshold values are defined and further studies are necessary. In the future, however, BNP and NT‐proBNP assessment could prove useful for deciding on the best treatment of patients with atrial fibrillation and to monitor patients after successful cardioversion.
Resynchronisation therapy has become an accepted therapeutic option for patients with severe heart failure. The optimal stimulation mode needs to be adapted using different diagnostic tools such as echocardiography, ergospirometry or the six minute walk test. Recently, some smaller studies have suggested that BNP or NT‐proBNP assessment can be used to optimise biventricular stimulation.
Implementation of BNP and NT‐proBNP assessment into current ESC guidelines
The role of BNP and NT‐proBNP testing is included in the guidelines for the diagnosis and treatment of chronic heart failure of the task force of the European Society of Cardiology, first published in 2000 and most recently updated in 2005. Assessment of both markers is considered to be a reliable rule‐out test of heart failure in primary care and in the emergency room. However, it is clearly stated that the role for treatment monitoring needs to be determined. Assessment of BNP for risk stratification is also mentioned in the current task force report on the management of acute coronary syndromes in patients presenting without persistent ST segment elevation, but without any recommendations for the application of BNP and NT‐proBNP in clinical routine.
CONCLUSIONS
BNP and NT‐proBNP have emerged as powerful biomarkers in various cardiovascular diseases. Both markers can be detected in serum plasma using commercially available assays. The diagnostic performance of BNP and NT‐proBNP is comparable and there is no meaningful difference between them. They reflect haemodynamic myocardial stress independent of the underlying pathology, thus they are not specific for a distinct pathology such as heart failure but for cardiovascular diseases in general. Their particular strength is to rule out heart failure in patients presenting to the emergency department with shortness of breath. They provide strong and independent prognostic information in patients with heart failure, stable coronary artery disease, acute coronary syndromes, and valvular aortic stenosis. There are some data available to suggest that BNP and NT‐proBNP values might assist in deciding upon the optimal treatment of patients with heart failure, but to date there are no data to support the use of these markers for reaching therapeutic decisions in patients with coronary artery disease or valvular heart disease (table 4).
Table 4 Clinical information that can be obtained from BNP or NT‐proBNP assessment.
| Diagnosis | Severity | Prognosis | Decision | |
|---|---|---|---|---|
| Heart failure | ++ | ++ | ++ | + |
| Stable CAD | 0 | + | ++ | 0 |
| ACS | 0 | 0 | ++ | 0 |
| Aortic stenosis | 0 | + | + | 0 |
++, strong evidence; +, evidence derived from smaller studies; 0, no data available.
ACS, acute coronary syndrome; CAD, coronary artery disease.
Role of BNP and NT‐proBNP in clinical routine: key points
B‐type natriuretic peptide (BNP) and NT‐proBNP are reliable biomarkers, reflecting myocardial stress caused by various cardiovascular diseases
Both markers are stable in whole blood and can be measured in clinical routine using fully automated commercially available assays
The diagnostic performance of BNP and NT‐proBNP is comparable and there is no meaningful difference between the two
The particular strength of BNP and NT‐proBNP is to rule out heart failure in patients with shortness of breath in the emergency department
Both markers provide prognostic information in patients with heart failure, coronary artery disease, and valvular heart disease
Additional references appear on the Heart website—http://www.heartjnl.com/supplemental
Additional references appear on the Heart website—http://www.heartjnl.com/supplemental
Supplementary Material
Footnotes
In compliance with EBAC/EACCME guidelines, all authors participating in Education in Heart have disclosed potential conflicts of interest that might cause a bias in the article
Additional references appear on the Heart website—http://www.heartjnl.com/supplemental
References
- 1.de Lemos J A, McGuire D K, Drazner M H. B‐type natriuretic peptide in cardiovascular disease. Lancet 2003362316–322.This review summarises present knowledge on the physiology of BNP and provides comprehensive data on the diagnostic and therapeutic potential of BNP in patients with heart failure. [DOI] [PubMed] [Google Scholar]
- 2.Redfield M M, Rodeheffer R J, Jacobsen S J.et al Plasma brain natriuretic peptide concentration: impact of age and gender. J Am Coll Cardiol 200240976–982. [DOI] [PubMed] [Google Scholar]
- 3.Luchner A, Hengstenberg C, Lowel H.et al Effect of compensated renal dysfunction on approved heart failure markers: direct comparison of brain natriuretic peptide (BNP) and N‐terminal pro‐BNP. Hypertension 200546118–123. [DOI] [PubMed] [Google Scholar]
- 4.Maisel A S, Krishnaswamy P, Nowak R M.et al Rapid measurement of B‐type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med 2002347161–167.The Breath Not Properly (BNP) study provided important data on the diagnostic performance of BNP to detect heart failure in patients presenting to the emergency department with the cardinal symptom of shortness of breath. [DOI] [PubMed] [Google Scholar]
- 5.Januzzi J L, Jr, Camargo C A, Anwaruddin S.et al The N‐terminal pro‐BNP investigation of dyspnea in the emergency department (PRIDE) study. Am J Cardiol 200595948–954. [DOI] [PubMed] [Google Scholar]
- 6.Wieczorek S J, Wu A H, Christenson R.et al A rapid B‐type natriuretic peptide assay accurately diagnoses left ventricular dysfunction and heart failure: a multicenter evaluation. Am Heart J 2002144834–839. [DOI] [PubMed] [Google Scholar]
- 7.Mueller C, Scholer A, Laule‐Kilian K.et al Use of B‐type natriuretic peptide in the evaluation and management of acute dyspnea. N Engl J Med 2004350647–654.The BASEL study demonstrated that BNP measurement in the emergency department reduces hospitalisation rate and total treatment costs with comparable clinical outcome. [DOI] [PubMed] [Google Scholar]
- 8.Anand I S, Fisher L D, Chiang Y T.et al Changes in brain natriuretic peptide and norepinephrine over time and mortality and morbidity in the valsartan heart failure trial (Val‐HeFT). Circulation 20031071278–1283.To our knowledge this articles provides the largest database including BNP measurement and follow‐up data of 4305 patients with heart failure. [DOI] [PubMed] [Google Scholar]
- 9.Mueller T, Gegenhuber A, Poelz W.et al Diagnostic accuracy of B type natriuretic peptide and amino terminal proBNP in the emergency diagnosis of heart failure. Heart 200591606–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Knebel F, Schimke I, Pliet K.et al NT‐ProBNP in acute heart failure: correlation with invasively measured hemodynamic parameters during recompensation. J Card Fail 200511(5 suppl)S38–S41. [DOI] [PubMed] [Google Scholar]
- 11.Cheng V, Kazanagra R, Garcia A.et al A rapid bedside test for B‐type peptide predicts treatment outcomes in patients admitted for decompensated heart failure: a pilot study. J Am Coll Cardiol 200137386–391. [DOI] [PubMed] [Google Scholar]
- 12.Troughton R W, Frampton C M, Yandle T G.et al Treatment of heart failure guided by plasma aminoterminal brain natriuretic peptide (N‐BNP) concentrations. Lancet 20003551126–1130.This small study demonstrated for the first time that NT‐proBNP guided treatment results in better clinical outcome compared to clinically guided therapy without NT‐proBNP assessment. [DOI] [PubMed] [Google Scholar]
- 13.Richards A M, Doughty R, Nicholls M G.et al Plasma N‐terminal pro‐brain natriuretic peptide and adrenomedullin: prognostic utility and prediction of benefit from carvedilol in chronic ischemic left ventricular dysfunction. Australia‐New Zealand heart failure group. J Am Coll Cardiol 2001371781–1787.This study showed that NT‐proBNP is able to discern heart failure patients who derive a benefit from carvedilol treatment. Thus this study demonstrates that therapeutic implications can be derived from BNP and NT‐proBNP assessment. [DOI] [PubMed] [Google Scholar]
- 14.Hartmann F, Packer M, Coats A J.et al Prognostic impact of plasma N‐terminal pro‐brain natriuretic peptide in severe chronic congestive heart failure: a substudy of the carvedilol prospective randomized cumulative survival (COPERNICUS) trial. Circulation 20041101780–1786. [DOI] [PubMed] [Google Scholar]
- 15.Jernberg T, Stridsberg M, Venge P.et al N‐terminal pro brain natriuretic peptide on admission for early risk stratification of patients with chest pain and no ST‐segment elevation. J Am Coll Cardiol 200240437–445. [DOI] [PubMed] [Google Scholar]
- 16.Heeschen C, Hamm C W, Mitrovic V.et al N‐terminal pro‐B‐type natriuretic peptide levels for dynamic risk stratification of patients with acute coronary syndromes. Circulation 20041103206–3212.Among the large multicentre studies, the data from the PRISM trial emphasises the importance of serial NT‐proBNP measurement for assessing dynamic risk stratification. [DOI] [PubMed] [Google Scholar]
- 17.Richards A M, Nicholls M G, Espiner E A.et al B‐type natriuretic peptides and ejection fraction for prognosis after myocardial infarction. Circulation 20031072786–2792. [DOI] [PubMed] [Google Scholar]
- 18.Jernberg T, Lindahl B, Siegbahn A.et al N‐terminal pro‐brain natriuretic peptide in relation to inflammation, myocardial necrosis, and the effect of an invasive strategy in unstable coronary artery disease. J Am Coll Cardiol 2003421909–1916. [DOI] [PubMed] [Google Scholar]
- 19.Weber M, Dill T, Arnold R.et al N‐terminal B‐type natriuretic peptide predicts extent of coronary artery disease and ischemia in patients with stable angina pectoris. Am Heart J 2004148612–620. [DOI] [PubMed] [Google Scholar]
- 20.Bibbins‐Domingo K, Ansari M, Schiller N B.et al B‐type natriuretic peptide and ischemia in patients with stable coronary disease: data from the Heart and Soul study. Circulation 20031082987–2992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kragelund C, Gronning B, Kober L.et al N‐terminal pro‐B‐type natriuretic peptide and long‐term mortality in stable coronary heart disease. N Engl J Med 2005352666–675.This study examines the prognostic information which can be derived from measurement of NT‐proBNP in patients with stable coronary artery disease. [DOI] [PubMed] [Google Scholar]
- 22.Gerber I L, Stewart R A, Legget M E.et al Increased plasma natriuretic peptide levels reflect symptom onset in aortic stenosis. Circulation 20031071884–1890. [DOI] [PubMed] [Google Scholar]
- 23.Weber M, Arnold R, Rau M.et al Relation of N‐terminal pro B‐type natriuretic peptide to progression of aortic valve disease. Eur Heart J 2005261023–1030. [DOI] [PubMed] [Google Scholar]
- 24.Bergler‐Klein J, Klaar U, Heger M.et al Natriuretic peptides predict symptom‐free survival and postoperative outcome in severe aortic stenosis. Circulation 20041092302–2308.The presented data demonstrate that elevated BNP values in patients with aortic stenosis provide prognostic information for an unfavourable clinical course. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.