Randomised clinical trials of drug treatment for chronic heart failure are the basis of many physicians' beliefs about heart failure. Due to the selection bias of such studies—which preferentially recruit relatively young white men with coronary artery disease—relatively little attention has focused on gender differences in heart failure. This article provides an overview of such gender differences, based on population‐based studies in North America and Europe.
PREVALENCE
It is difficult to make comparisons between prevalence studies (and across time) due to differences in the case definitions employed.1 There is no “gold standard” for heart failure, and most recent studies rely heavily on echocardiography to demonstrate underlying cardiac abnormalities in patients with symptoms that might be caused by heart failure. Most studies rely on administering questionnaires regarding symptoms, a few collect information on clinical signs, and very few combine robust clinical assessment with echocardiographic data. The prevalence of left ventricular systolic dysfunction is relatively straightforward, if time consuming, to establish within a population; however, this is not synonymous with heart failure.
The Framingham heart study, a large cohort study from Massachusetts in the United States, reported an estimated prevalence of heart failure of 0.8% in both genders within the age group of 50–59 years. The prevalence increases notably with advancing age, rising to 6.6% and 7.9% in men and women, respectively, aged 80–89 years.2 The US National Health And Nutrition Examination Survey (NHANES) study reported an overall prevalence of approximately 2% in both men and women aged 25–74 years, based on a clinical score system derived from the Framingham heart study.3
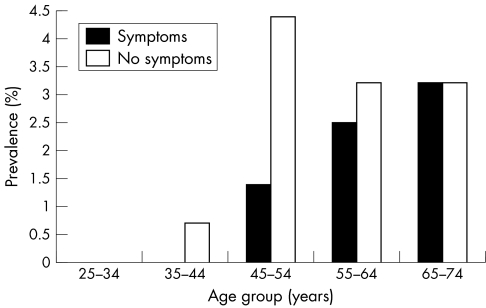
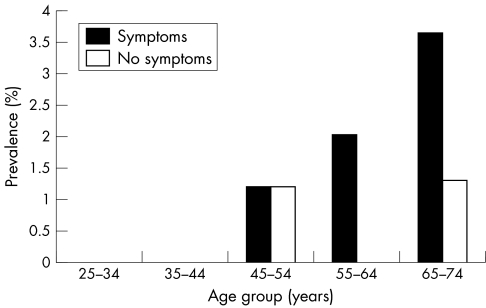
European data suggest a similar prevalence of heart failure of between 1–2%.4,5 In the UK, there have been two major population based echocardiographic studies of heart failure prevalence. The 1992 MONICA (monitoring trends and determinants in cardiovascular disease) Glasgow population was screened using questionnaire and echocardiography. The response rate in this cross‐sectional survey was 83%. The reported prevalence of definite left ventricular (LV) systolic dysfunction, defined as a LV ejection fraction (LVEF) of 30% or less, was 4% in men and 2% in women aged 25–74 years. The prevalence increased with age in both genders. Approximately half of these cases were symptomatic and labelled as having “heart failure”6 (figs 1 and 2). This study did not attempt to identify subjects with heart failure and “preserved” LV systolic function. The “Heart of England” screening study assessed the prevalence of LV systolic dysfunction, and heart failure, in the West Midlands, England between 1995 and 1999. The prevalence of “definite” heart failure, defined in accordance with the European Society of Cardiology (ESC) criteria,7 was 3% in men and 1.7% in women. “Probable” heart failure, defined as either patients with symptoms and borderline LVEF or patients with definitely impaired LVEF with previous symptoms but now symptom‐free due to appropriate treatment (angiotensin converting enzyme (ACE) inhibitor or diuretic), was reported in a further 0.8%. Gender subclassification was not reported in this “probable” heart failure group.8
Figure 1 Prevalence of definite left ventricular systolic dysfunction (left ventricular ejection fraction ⩽ 30%) by age group in men based on Glasgow MONICA study data.6
Figure 2 Prevalence of definite left ventricular systolic dysfunction (left ventricular ejection fraction ⩽ 30%) by age group in women based on Glasgow MONICA study data.6
A recent report from Olmsted County, Minnesota has evaluated the prevalence of “diastolic” heart failure. In this cross‐sectional survey of the population aged over 45 years, the overall prevalence of heart failure, as defined by Framingham criteria, was 2.2%, comparable to earlier studies; 44% of heart failure cases had preserved systolic function (LVEF > 50%) on echocardiography. The prevalence of diastolic dysfunction, as defined by detailed echocardiographic measurements of mitral inflow, pulmonary venous flow and Doppler tissue imaging of mitral annular motion, was higher in the older population, and in those with a history of hypertension, diabetes, coronary disease and previous myocardial infarction. The prevalence of diastolic dysfunction was similar in both genders.9 A small nested case–control study from the Framingham heart study suggested that an EF < 50% was less common in women with heart failure than in men (27%, 95% confidence interval (CI) 11% to 43%, compared with 68%, 95% CI 52% to 82%, respectively).10 Similar findings have been reported from a multinational survey of patients admitted to hospital with heart failure: 51% of men but only 28% of women had an LVEF less than 40%.11
INCIDENCE
There have been relatively few population‐based studies of the incidence of heart failure.1 Comparison between studies is again difficult due to differences in methodology.
In the USA, the Framingham heart study has reported the incidence of heart failure to be 0.3% per annum in men and 0.2% per annum in women aged 50–59 years, rising by a factor of 10 to 2.7% per annum in men and 2.2% per annum in women aged 80–89 years. The mean age at the time of diagnosis of heart failure was 70 years. The incidence of heart failure was significantly higher in men than women at all ages with an age‐standardised incidence ratio of 1.67.2
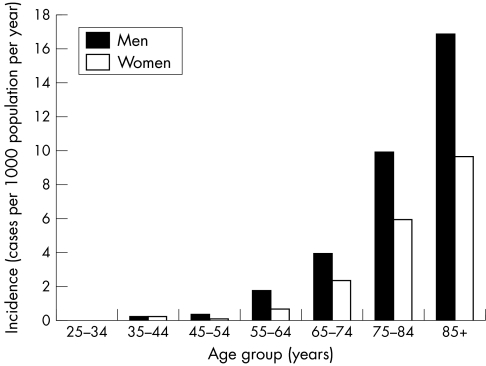
The Hillingdon heart failure study evaluated the incidence of heart failure in one district of West London, England, using clinical and echocardiographic data and a case definition based on three cardiologists applying the ESC definition of heart failure.7 This study reported an incidence rate of 0.2% per annum in men and 0.1% per annum in women aged 55–64 years. The incidence rose almost 10‐fold to 1.7% in men and 1% in women aged 85 years or over. The median age at the time of diagnosis of heart failure was 76 years. The incidence of heart failure was significantly higher in men than women at all ages with an age‐standardised ratio of 1.7512 (fig 3). On the basis of this study it is estimated that there are approximately 34 000 incident cases of heart failure per year in men and 29 000 cases per year in women in the UK.13
Figure 3 Incidence of heart failure by age group and gender based on Hillingdon heart failure study data.12
Data on the secular trend in the incidence of heart failure in Europe are currently unavailable. Reports from the United States are inconsistent. In the Framingham cohort between 1950 and 1999, there was a non‐significant 7% reduction in the age‐adjusted incidence of heart failure in men. In women, however, there was a significant 31% reduction in the age‐adjusted incidence during that period.14 A study from Olmsted County, Minnesota, USA compared the incidence of heart failure between 1981 and 1991 and reported no significant change.15
AETIOLOGY
Heart failure is a clinical syndrome, and not a complete diagnosis in itself. It is important to determine the underlying cardiac abnormality. Several pathologies frequently co‐exist: coronary artery disease, hypertension, and diabetes mellitus, to name but a few. Population based studies are less likely to use the whole range of cardiac investigations that would be used in the precise characterisation of heart failure in clinical practice; coronary angiography may not be performed systematically, and perfusion imaging is unlikely. This may lead to misclassification of the underlying aetiology of heart failure, with coronary artery disease not being implicated except in patients with obvious history, electrocardiographic changes or regional wall motion abnormalities on echocardiography. Such misclassification may be different by age and gender of the patient, biasing studies to find a difference in aetiology that is untrue.
In a UK population‐based study of incident (new) cases of heart failure in South East London (the Bromley heart failure study), 52% of cases aged under 75 were ascribed to coronary artery disease after systematic study with coronary angiography and myocardial perfusion imaging in the mid 1990s. This study demonstrated that using coronary angiography and perfusion imaging increases the proportion of cases in which coronary artery disease can be implicated: the diagnosis may be missed in 25% of cases if non‐invasive testing alone is used.16 The Framingham heart study has reported a significantly lower age‐adjusted prevalence of coronary artery disease in women with incident heart failure. Coronary artery disease was reported as the aetiological factor in 59% of men and 47% of women (age adjusted odds ratio (OR) 0.55, 95% CI 0.40 to 0.76) for the period 1948–88.2 Valvular disease, hypertension and diabetes were more common in women than in men.2 The incidence of coronary heart disease rises sharply in peri‐ and post‐menopausal women. This may be due to gender based differences at a molecular and cellular level, particularly with regard to sex steroid hormones and receptors and their downstream effects on vascular tone, blood pressure, lipid metabolism, thrombosis and atherosclerosis.17
The Framingham data have shown a change in aetiology over time in both men and women. The prevalence of coronary disease among new cases of heart failure has risen by 46% per decade (p < 0.05).2 The prevalence of diabetes has increased by 21% and 24% per decade in men and women, respectively. By contrast, hypertension (and electrocardiographic left ventricular hypertrophy) and valvular heart disease have decreased in prevalence for both genders.18 This shift in the relative importance of the different aetiological factors for heart failure presumably relates to improvements in the detection and management of hypertension, the virtual disappearance of rheumatic fever in the United States after the first world war, and improved survival from acute coronary disease. Less misclassification of coronary artery disease may also play a part, with the more widespread use of coronary angiography and perfusion imaging.
SURVIVAL
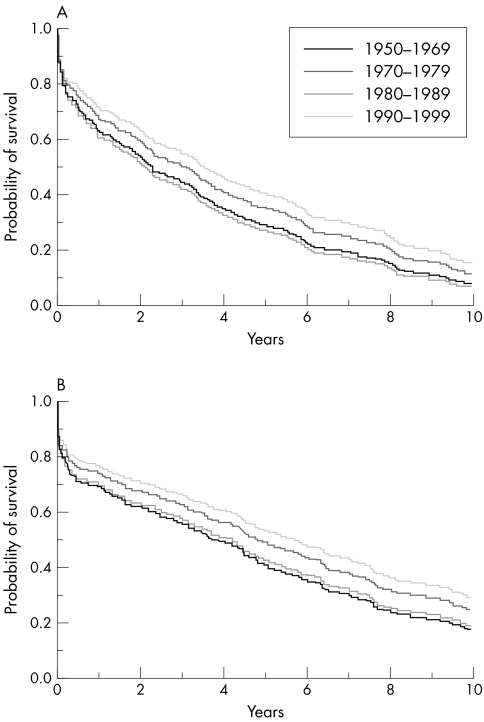
The prognosis of heart failure, although improved by modern treatments, remains poor with particularly high early mortality rates. The 90 day, one year, and five year mortality rates in the Framingham heart study, based on incident cases identified between 1948 and 1988, were 27%, 43%, and 75%, respectively, for men. The comparative figures for women were only slightly better at 28%, 36%, and 62% in women. Median survival was 1.7 years in men, and 3.2 years in women. The age‐adjusted survival was significantly better in women (hazard ratio 0.64, 95% CI 0.54 to 0.77).2 Survival appears to have improved between 1990 and 1999 in the Framingham population, perhaps related to the use of ACE inhibitors, with one year and five year age‐adjusted mortality rates improving to 28% and 59%, respectively, in men, and 24% and 45%, respectively, in women14 (fig 4). The NHANES study reported a considerably better long term survival in women with heart failure with a 15 year total mortality rate of 39.1% for women, compared with 71.8% for men.3 The case definition in NHANES was considerably less strict than that employed in Framingham and other population based studies, and may “overdiagnose” heart failure in women, biasing the study to overestimate the mortality differential between the sexes.
Figure 4 Temporal trends in age‐adjusted survival after the onset of heart failure among men (panel A) and women (panel B) from the Framingham heart study.14
Recent experience from the Hillingdon heart failure study in the UK, following up 220 incident cases of heart failure identified in 1995/96, confirmed a similar poor overall prognosis for incident heart failure patients. The overall mortality rates were 19%, 38% and 43% at one month, one year and 18 months, respectively, with no significant difference between the genders.19
Although generally considered to have a better prognosis than systolic heart failure, non‐systolic heart failure is not a benign condition. In one study, high risk (elderly and hospitalised) patients with diastolic heart failure (defined as a clinical history of heart failure but with an LVEF of 50% or higher) had an 18 month mortality of 33% in both genders.20 A recent report from Olmsted County, Minnesota, has evaluated the prognosis of diastolic dysfunction in a cross sectional survey of the local community aged 45 years and above. This study demonstrated that mild, moderate and severe diastolic dysfunction (evaluated by echocardiography) was significantly associated with an increase in all‐cause mortality (p < 0.001) when compared to normal diastolic function, and this finding was independent of age, gender and LVEF.9 A small nested case–control study from Framingham has reported increased mortality in patients with heart failure and normal EF (annual mortality 8.7% compared with 3.0% for age and gender matched controls), although not as high as in patients with heart failure and reduced EF (18.9% annual mortality compared with 4.1% for age and gender matched controls).10 The difference in mortality by EF disappears after adjustment for age, history of coronary artery disease, diabetes, atrial fibrillation, smoking status and blood pressure.10
Reports from clinical trials of drug treatment suggest that women have a better prognosis than men when they develop heart failure, particularly if the aetiology is non‐ischaemic. Selection bias and confounding cannot be excluded, as women are in the minority in such trials and may differ from the men in ways other than just gender.21,22
EVIDENCE BASE FOR THE MANAGEMENT OF HEART FAILURE
It is generally agreed that the evidence base for the management of heart failure is substantial. The evidence for benefit of ACE inhibitors, and β blockers, for the treatment of heart failure caused by LV systolic dysfunction is considered to be of the highest level.23,24 The majority of patients in these trials have been relatively young men of European origin either in North America or in Europe. Many assume that it is reasonable to extrapolate this benefit to women, and also to non‐white populations.
Although results from some ACE inhibitor randomised controlled trials have shown less impressive mortality reductions for women compared to men,25,26,27,28 a large meta‐analysis of 32 placebo controlled trials evaluating ACE inhibitor treatment for heart failure found no gender associated differences in mortality reduction.29 Also, the mortality reduction observed with β blockers does not appear to differ by gender.30,31,32 Randomised studies of cardiac resynchronisation therapy (CRT) in chronic heart failure tend to recruit men (approximate male to female ratio of 3:1), although there is no evidence of reduced benefit in women.33,34,35 This recruitment gender bias may be more related to the specific study entry criterion that requires patients to have a reduced LVEF, thereby excluding cases of non‐systolic heart failure, more common in women. In addition specialised centres tend to care for younger patients, who are more likely to be male than female.
Prevention of heart failure by treatment of hypertension and coronary artery disease is important. A meta‐analysis of over 40 000 patients with hypertension found no evidence of a gender difference in the odds ratios for benefit in any category of cardiovascular event.36 Most studies comparing outcomes after percutaneous or surgical coronary intervention in men and women have demonstrated worse outcomes in women. Clinical factors among women contributing to these gender differences include a delayed onset of disease, a tendency to present at an older age, a higher prevalence of co‐morbidities at the time of presentation, and possibly smaller coronary arteries.37
GENDER BIAS IN THE HEALTH CARE SYSTEM
A recent European multi‐centre survey of the quality of care in patients admitted to hospital with heart failure reported that there is less use of life‐prolonging treatment (ACE inhibitors, β blockers, spironolactone) in the 70 years and over age group, and that the odds of receiving ACE inhibitor and β blocker treatment was significantly higher in men than women (OR 1.34, 95% CI 1.22 to 1.48).38 A European multi‐centre survey of primary care heart failure management observed that the odds of receiving an ACE inhibitor was significantly reduced in women (OR 0.80, 95% CI 0.70 to 0.92).39 Primary care data from the UK demonstrate that at all ages, women are less likely to receive treatment with ACE inhibitors for heart failure (with a 9.5% lower age‐standardised prescription rate for women compared with men).40 Although the 1990s have seen a substantial (> 40%) increase in treatment with ACE inhibitors, this gender bias persists.40
SUMMARY AND CONCLUSIONS
The incidence and prevalence of heart failure is lower in women than in men at all ages. However, due to the steep increase in incidence with age, and the proportionally larger number of elderly women in the populations of the developed world, the total number of men and women living with heart failure is similar. Heart failure with preserved systolic function (or proven or presumed “diastolic” dysfunction) is more common in women, perhaps related to gender differences in the myocardial response to injury, and the lower prevalence of coronary heart disease in women at all ages compared with men. Patients with systolic heart failure have a poor prognosis, particularly in the early period after a new diagnosis, and irrespective of gender. The size of the evidence base for the treatment of heart failure in women is smaller than for men, mainly due to the selection bias demonstrated by centres recruiting to randomised clinical trials. At least part of this bias is age, rather than gender, related. Prospective clinical trials should ensure that gender based differences in response to therapeutic options are considered. Currently, despite a lack of evidence that ACE inhibitors or β blockers have any less effect in women, they are less likely to receive such therapies in clinical practice, even after correction for age bias. Although it is unarguably important that clinical trials should try harder to recruit older patients and women to increase the generalisability of the evidence base, from the public health viewpoint the implementation of the evidence in all patients, irrespective of gender, is the key factor in improving the outcome for patients with heart failure.
Abbreviations
ACE - angiotensin converting enzyme
EF - ejection fraction
CRT - cardiac resynchronisation therapy
ESC - European Society of Cardiology
LV - left ventricular
LVEF - left ventricular ejection fraction
MONICA - monitoring trends and determinants in cardiovascular disease
NHANES - US National Health And Nutrition Examination Survey
References
- 1.Cowie M R, Mosterd A, Wood D A.et al The epidemiology of heart failure. Eur Heart J 199718208–225. [DOI] [PubMed] [Google Scholar]
- 2.Ho K K, Pinsky J L, Kannel W B.et al The epidemiology of heart failure: the Framingham Study. J Am Coll Cardiol 199322(4 suppl A)6A–13A. [DOI] [PubMed] [Google Scholar]
- 3.Schocken D D, Arrieta M I, Leaverton P E.et al Prevalence and mortality rate of congestive heart failure in the United States. J Am Coll Cardiol 199220301–306. [DOI] [PubMed] [Google Scholar]
- 4.Eriksson H, Svardsudd K, Larsson B.et al Risk factors for heart failure in the general population: the study of men born in 1913. Eur Heart J 198910647–656. [DOI] [PubMed] [Google Scholar]
- 5.Landahl S, Svanborg A, Astrand K. Heart volume and the prevalence of certain common cardiovascular disorders at 70 and 75 years of age. Eur Heart J 19845326–331. [DOI] [PubMed] [Google Scholar]
- 6.McDonagh T A, Morrison C E, Lawrence A.et al Symptomatic and asymptomatic left‐ventricular systolic dysfunction in an urban population. Lancet 1997350829–833. [DOI] [PubMed] [Google Scholar]
- 7.European Society of Cardiology Guidelines for the diagnosis of heart failure. The task force on heart failure of the European Society of Cardiology. Eur Heart J 199516741–751. [PubMed] [Google Scholar]
- 8.Davies M K, Hobbs F D R, Davis R C.et al Prevalence of left‐ventricular systolic dysfunction and heart failure in the echocardiographic Heart of England screening study: a population based study. Lancet 2001358439–444. [DOI] [PubMed] [Google Scholar]
- 9.Redfield M M, Jacobsen S J, Burnett J C., Jret al Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. JAMA 2003289194–202. [DOI] [PubMed] [Google Scholar]
- 10.Vasan R S, Larson M G, Benjamin E J.et al Congestive heart failure in subjects with normal versus reduced left ventricular ejection fraction: prevalence and mortality in a population‐based cohort. J Am Coll Cardiol 1999331948–1955. [DOI] [PubMed] [Google Scholar]
- 11.Cleland J G, Swedberg K, Follath F.et al The EuroHeart Failure survey programme‐a survey on the quality of care among patients with heart failure in Europe. Part 1: patient characteristics and diagnosis. Eur Heart J 200324442–463. [DOI] [PubMed] [Google Scholar]
- 12.Cowie M R, Wood D A, Coats A J.et al Incidence and aetiology of heart failure: a population‐based study. Eur Heart J 199920421–428. [DOI] [PubMed] [Google Scholar]
- 13.British Heart Foundation Coronary heart disease statistics: heart failure supplement. London: BHF, 2002
- 14.Levy D, Kenchaiah S, Larson M G.et al Long‐term trends in the incidence of and survival with heart failure. N Engl J Med 20023471397–1402. [DOI] [PubMed] [Google Scholar]
- 15.Senni M, Tribouilloy C M, Rodeheffer R J.et al Congestive heart failure in the community: trends in incidence and survival in a 10‐year period. Arch Intern Med 199915929–34. [DOI] [PubMed] [Google Scholar]
- 16.Fox K F, Cowie M R, Wood D A.et al Coronary artery disease as the cause of incident heart failure in the population. Eur Heart J 200122228–236. [DOI] [PubMed] [Google Scholar]
- 17.Mendelsohn M E, Karas R H. Molecular and cellular basis of cardiovascular gender differences. Science 20053081583–1587. [DOI] [PubMed] [Google Scholar]
- 18.Kannel W B, Ho K K, Thom T. Changing epidemiological features of cardiac failure. Br Heart J 199472S3–S9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cowie M R, Wood D A, Coats A J.et al Survival of patients with a new diagnosis of heart failure: a population based study. Heart 200083505–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ibrahim S A, Burant C J, Kent K C. Elderly hospitalized patients with diastolic heart failure: lack of gender and ethnic differences in 18‐month mortality rates. J Gerontol A Biol Sci Med Sci 20035856–59. [DOI] [PubMed] [Google Scholar]
- 21.Adams K F., Jr Sueta CA, Gheorghiade M, et al. Gender differences in survival in advanced heart failure. Insights from the FIRST study. Circulation 1999991816–1821. [DOI] [PubMed] [Google Scholar]
- 22.Ghali J K, Krause‐Steinrauf H J, Adams K F.et al Gender differences in advanced heart failure: insights from the BEST study. J Am Coll Cardiol 2003422128–2134. [DOI] [PubMed] [Google Scholar]
- 23.Hunt S A, Baker D W, Chin M H.et al ACC/AHA guidelines for the evaluation and management of chronic heart failure in the adult: executive summary. A Report of the American College of Cardiology/American Heart Association task force on practice guidelines (committee to revise the 1995 guidelines for the evaluation and management of heart failure): developed in collaboration with the International Society for Heart and Lung Transplantation; endorsed by the Heart Failure Society of America, Circulation 20011042996–3007. [DOI] [PubMed] [Google Scholar]
- 24.Task Force for the Diagnosis and Treatment of Chronic Heart Failure Guidelines for the diagnosis and treatment of chronic heart failure. Eur Heart J 2001221527–1560. [DOI] [PubMed] [Google Scholar]
- 25.CONSENSUS Trial Study Group Effects of enalapril on mortality in severe congestive heart failure. Results of the cooperative North Scandinavian enalapril survival study (CONSENSUS). The CONSENSUS trial study group. N Engl J Med 19873161429–1435. [DOI] [PubMed] [Google Scholar]
- 26.The SOLVD Investigators Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. The SOLVD investigators. N Engl J Med 1991325293–302. [DOI] [PubMed] [Google Scholar]
- 27.Pfeffer M A, Braunwald E, Moye L A.et al Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction: results of the survival and ventricular enlargement (SAVE) trial. N Engl J Med 1992327669–677. [DOI] [PubMed] [Google Scholar]
- 28.Kober L, Torp‐Pedersen C, Carlsen J E.et al A clinical trial of the angiotensin‐converting‐enzyme inhibitor trandolapril in patients with left ventricular dysfunction after myocardial infarction. Trandolapril cardiac evaluation (TRACE) study group. N Engl J Med 19953331670–1676. [DOI] [PubMed] [Google Scholar]
- 29.Garg R, Yusuf S. Overview of randomized trials of angiotensin‐converting enzyme inhibitors on mortality and morbidity in patients with heart failure. Collaborative group on ACE inhibitor trials. JAMA 19952731450–1456. [PubMed] [Google Scholar]
- 30.Packer M, Bristow M R, Cohn J N.et al The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. N Engl J Med 19963341349–1355. [DOI] [PubMed] [Google Scholar]
- 31.Packer M, Fowler M B, Roecker E B.et al Effect of carvedilol on the morbidity of patients with severe chronic heart failure: results of the carvedilol prospective randomized cumulative survival (COPERNICUS) study. Circulation 20021062194–2199. [DOI] [PubMed] [Google Scholar]
- 32.MERIT‐HF Study Group Effect of metoprolol CR/XL in chronic heart failure: metoprolol CR/XL randomised intervention trial in congestive heart failure (MERIT‐HF). Lancet 19993532001–2007. [PubMed] [Google Scholar]
- 33.Young J B M, Abraham W T M, Smith A L M.et al Combined cardiac resynchronization and implantable cardioversion defibrillation in advanced chronic heart failure: the MIRACLE ICD trial. JAMA 20032892685–2694. [DOI] [PubMed] [Google Scholar]
- 34.Cleland J G, Daubert J C, Erdmann E.et al The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med 20053521539–1549. [DOI] [PubMed] [Google Scholar]
- 35.Linde C, Leclercq C, Rex S.et al Long‐term benefits of biventricular pacing in congestive heart failure: results from the multisite stimulation in cardiomyopathy (MUSTIC) study. J Am Coll Cardiol 200240111–118. [DOI] [PubMed] [Google Scholar]
- 36.Gueyffier F, Boutitie F, Boissel J P.et al Effect of antihypertensive drug treatment on cardiovascular outcomes in women and men. A meta‐analysis of individual patient data from randomized, controlled trials. The INDANA investigators. Ann Intern Med 1997126761–767. [DOI] [PubMed] [Google Scholar]
- 37.Lansky A J. Outcomes of percutaneous and surgical revascularization in women. Prog Cardiovasc Dis 200446305–319. [DOI] [PubMed] [Google Scholar]
- 38.Komajda M, Follath F, Swedberg K.et al The EuroHeart failure survey programme – a survey on the quality of care among patients with heart failure in Europe. Part 2: treatment. Eur Heart J 200324464–474. [DOI] [PubMed] [Google Scholar]
- 39.Cleland J G, Aguilar J C, Dietz R.et al Management of heart failure in primary care (the IMPROVEMENT of heart failure programme): an international survey. Lancet 20023601631–1639. [DOI] [PubMed] [Google Scholar]
- 40.Ellis C, Shamini G. Prevalence and management of heart failure in general practice in England and Wales, 1994–98. Health Statistics Quarterly 20011117–24. [Google Scholar]