Direct manual compression without concurrent technical surveillance may be a simple alternative to both ultrasound guided compression repair (UGCR) and ultrasound guided thrombin injection. Since this simple method of manual compression repair (MCR) proved to be effective in a preliminary study, we conducted a prospective, randomised trial comparing MCR versus UGCR.1
PATIENTS AND METHODS
From September 1997 to January 2000 Duplex ultrasonography was performed in all patients with clinically suspected disease in the groin after cardiac and peripheral arterial catheterisation.
Patients were considered for the study when none of the following exclusion criteria existed: (1) imminent rupture of the lesion; (2) coexisting massive haematoma; (3) skin necrosis; (4) active infection in the groin; or (5) lower limb ischaemia. After providing informed consent they were randomly assigned to either UGCR or MCR.
A group of six investigators performed sonography, UGCR, and MCR. UGCR was carried out as previously published for a maximum of 60 minutes.2,3 MCR was performed as for primary haemostasis after arterial catheterisation. Pressure was mainly directed to the area of maximum pulsation and was gradually increased until the pathological pulsation of the haematoma or the femoral thrill disappeared. Pressure was maintained until the pathological pulsation of the haematoma or the femoral bruit had permanently disappeared but not longer than 60 minutes.
After UGCR and MCR, a compression bandage was applied and the patients rested in bed for 24 hours. The next day a follow up ultrasound examination was performed. In case of failed repair of the lesion, the procedure was repeated in an identical manner for a maximum of three times.
The primary end point of the study was the rate of successful repair of the pseudoaneurysm after MCR or UGCR. The primary hypothesis was that MCR is not inferior to UGCR.
RESULTS
Postcatheterisation pseudoaneurysms were diagnosed in 185 patients, 168 of whom met the study criteria. Thus, 84 were randomly assigned to MCR and 84 to UGCR. The two patient groups did not differ in age, sex, body mass index, size of pseudoaneurysms, and treatment with antithrombotics.
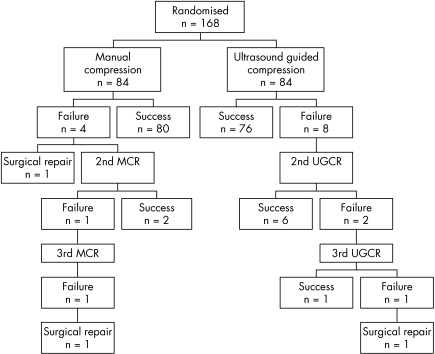
All procedures were completed as planned. MCR was successful in 82 (98%) patients; of these, 80 were cured at the first attempt and two required two compression manoeuvres for definite cure (fig 1). UGCR was successful in 83 patients (99%); of these, 76 were cured at the first attempt; six required two sessions and one patient required three for definite cure (fig 1). The final success rates of MCR and UGCR, the number of compression manoeuvres, and the compression time necessary for success did not differ. The three patients with unsuccessful compression repair were referred for surgical repair.
Figure 1 Time course of compression repair. MCR, manual compression repair; UGCR, ultrasound guided compression repair.
Compared with patients who were successfully treated at the first attempt, a significantly greater proportion of those who needed several attempts or who could not be treated successfully with compression were taking oral anticoagulants or heparin. No such difference was observed for antiplatelet drugs, patient characteristics, and geometry of the pseudoaneurysm. Although compression time was significantly greater for those who could not be cured at first attempt, pain as assessed on a numeric analogue scale was not greater among this patient group.
The only side effects observed were occasional mild vagal reactions requiring administration of atropine in one patient undergoing MCR. No other complications were observed; in particular, there were no cases of acute vessel occlusion or distal embolisation. Analgesics or sedatives had to be administered to eight patients in the MCR group and in 12 patients in the UGCR group. Pain and discomfort as estimated on a numeric analogue scale differed widely between patients, with a similar distribution pattern in both treatment groups.
DISCUSSION
Our data show that MCR without ultrasound control is as effective and safe as performance of the procedure with ultrasound control. MCR allows a more comfortable and less fatiguing posture for the operator and can be performed on any ward without the prolonged use of costly equipment. The success rate in both patient groups is higher than in our earlier experience1,2,3 and in that of most other authors. This may in part be due to increasing skill; however, the major reason for improving success rates most likely is the reduced use of anticoagulants after vascular interventions, since anticoagulants are known to reduce significantly the success rate of compression repair.2,4 Accordingly, we were successful at the first attempt in 95% (120 of 126) of patients without anticoagulants and in 86% (36 of 42) of patients given anticoagulants. Apart from occasional mild vagal reactions, none of our patients had significant side effects or complications as a result of blind groin compression. In particular, we observed no cases of acute arterial or venous thrombosis or distal embolisation.
Lately, ultrasound guided injection of thrombin has been proposed as an alternative to UGCR.4,5 It has several problems, however. Acute arterial occlusion and blue toe syndrome, deep vein thrombosis, large residual haematoma necessitating surgical removal, groin abscess, and anaphylaxis have all been reported. A recent study with long term follow up after a mean of 99 days showed residual groin haematoma in 26% of the patients and partial reperfusion of the pseudoaneurysm in 4%. Although ultrasound guided percutaneous thrombin injection appears attractive, mainly because it seems to be less cumbersome and less time consuming than compression repair, promoting it as a first line approach for the treatment of postcatheterisation pseudoaneurysms is premature. It may, however, have a place as a rescue procedure after failed MCR or UGCR.
Clinically guided MCR is as successful and safe as UGCR. It is non‐invasive and avoids the risks of thrombin injection. Since it requires less technical equipment than both UGCR and ultrasound guided percutaneous thrombin injection, MCR is more cost effective than the other two methods. MCR appears to be the first treatment of choice for the vast majority of patients with a pseudoaneurysm.
References
- 1.Theiss W, Schreiber K, Schomig A. Manual compression repair of post‐catheterization femoral pseudoaneurysms: an alternative to ultrasound guided compression repair? Vasa 20023195–99. [DOI] [PubMed] [Google Scholar]
- 2.Schaub F, Theiss W, Heinz M.et al New aspects in ultrasound‐guided compression repair of postcatheterization femoral artery injuries. Circulation 1994901861–1865. [DOI] [PubMed] [Google Scholar]
- 3.Schaub F, Theiss W, Busch R.et al Management of 219 consecutive cases of postcatheterization pseudoaneurysm. J Am Coll Cardiol 199730670–675. [DOI] [PubMed] [Google Scholar]
- 4.La Perna L, Olin J W, Goines D.et al Ultrasound‐guided thrombin injection for the treatment of postcatheterization pseudoaneurysms. Circulation 20001022391–2395. [DOI] [PubMed] [Google Scholar]
- 5.Agarwal R, Agrawal S K, Roubin G S.et al Clinically guided closure of femoral arterial pseudoaneurysms complicating cardiac catheterization and coronary angioplasty. Cathet Cardiovasc Diagn 19933096–100. [DOI] [PubMed] [Google Scholar]