QT prolongation is known to be associated with increased risk of coronary heart disease and cardiovascular death.1,2 A high prevalence of QT prolongation has been reported in heart failure, but whether it is related to the severity of left ventricular systolic dysfunction (LVSD) or poor prognosis remains controversial.3,4
The Euro heart failure survey was conducted to discover whether appropriate tests were being performed according to European Society of Cardiology guidelines in patients hospitalised with or suspected to have heart failure.5 Data from 12 lead ECGs of these patients were used to evaluate whether QT interval is prolonged in LVSD and whether the degree of QT prolongation is related to the severity of LVSD.
METHODS
Data were collected from 11 356 patients with or suspected to have heart failure in 115 hospitals across 24 European countries over six weeks during 2000–2001. For this analysis we considered 5934 patients who had both ECG and an echocardiogram. A single observer, blinded to other data, measured ECG intervals to an accuracy of 0.1 mm (2–4 ms) with digital callipers (ABSolute digimatic, Mitutoyo). QT variables were measured from three non‐infarct chest or limb leads and averaged. Co‐workers reread and validated 400 ECGs. Bazett's method of correction for heart rate was used.
Local cardiologists reported echocardiograms in the participating hospitals. LVSD was classified qualitatively as none, mild, moderate, or severe.
We examined the relation between the ECG variables and the degree of left ventricular systolic function and the influence of drug treatment on QT variables. The group means were compared by analysis of variance or its non‐parametric equivalent. The interaction of drug treatment with LVSD was examined by log linear analysis. Each QT variable was arbitrarily divided into five categories of 20 ms intervals (QRS: ⩽ 100, 100–120, 121–140, 141–160, and > 160 ms; QTc: ⩽ 440, 441–460, 461–480, 481–500, and > 500 ms; and JTc ⩽ 330; 331–350, 351–370, 371–390, and > 390 ms). Each category was examined by a multivariable logistic regression model to predict the severity of LVSD. Odds ratios (ORs) with 95% confidence intervals (CIs) were obtained. SPSS version 12 (SPSS Inc, Chicago, Illinois, USA) was used for statistical analysis.
RESULTS
In this study group (n = 5934), the mean (SD) age was 69 (13) years, 41% (n = 2445) were women, 65% (n = 3874) had coronary disease, 26% (n = 1572) had diabetes, 47% (n = 2784) had hypertension, and 16% (n = 962) had renal dysfunction. Forty four per cent (n = 2598) were treated with β blockers.
The mean (SD) QT interval was 389 (55) ms, QTc was 447 (41) ms, QRS was 112 (29) ms, JT was 277 (50) ms, JTc was 334 (37) ms, RR was 774 (189) ms, and PR was 178 (36) ms. Fifty five per cent (n = 3236) of patients had QTc > 440 ms, 29% (n = 1709) had QRS > 120 ms, and 20% (n = 1200) had left bundle branch block pattern.
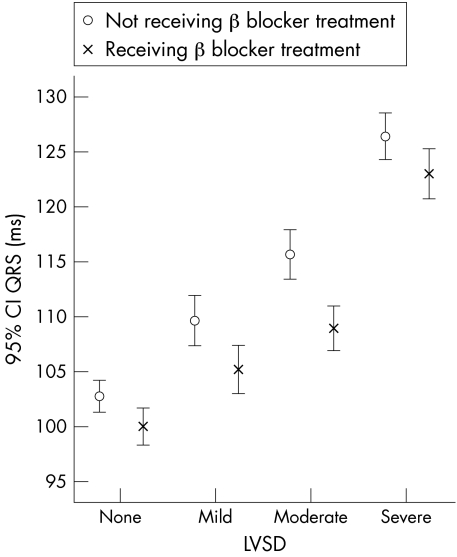
LVSD was present in 71% (n = 4213): mild in 17% (n = 1012), moderate in 23% (n = 1374), and severe in 31% (n = 1827). LVSD was severe in 54% (n = 642) of patients with left bundle branch block. Patients with LVSD had prolonged QT (392 v 383 ms, p < 0.001), QTc (449 v 439 ms, p < 0.001), and QRS (117 v 102 ms, p < 0.001) but not JT intervals (276 v 281 ms). The QT, QTc, and QRS intervals (fig 1) were longer with increasing severity of LVSD. The JT and JTc intervals were shorter as LVSD increased in severity. Patients treated with β blockers (n = 2598; 44%) were younger (66 v 70 years, p < 0.001) and had a shorter QRS (110 v 114 ms, p < 0.001; fig 1), shorter QTc (443 v 449 ms, p < 0.001), and shorter JTc intervals (333 v 336 ms, p = 0.005). β Blocker treatment did not influence the effect of LVSD on the QT variables. There was no interaction between the severity of LVSD and β blocker treatment. No similar relation was found with other drugs such as digoxin or angiotensin converting enzyme inhibitors.
Figure 1 Relation between QRS interval and severity of left ventricular systolic dysfunction (LVSD) and the effect of β blocker treatment. CI, confidence interval.
When the QT variables were subjected to multivariable logistic regression analysis (that also included age, sex, diabetes, and β blocker effect), we found that only QRS prolongation was an independent predictor of moderate to severe left ventricular dysfunction. The OR for having moderate or severe LVSD increased with increasing QRS interval (dose response effect): QRS 100–120 ms, OR 1.5 (95% CI 1.3 to 1.7); 120–140 ms, OR 2.0 (95% CI 1.6 to 2.4); 141–160 ms, OR 2.1 (95% CI 1.7 to 2.5); and > 160 ms, OR 3.1 (95% CI 2.3 to 4.1). But no such effect was seen with QTc interval: QTc 440–460 ms, OR 1.1 (95% CI 1.0 to 1.3); 461–480 ms, OR 1.2 (95% CI 1.0 to 1.4); 480–500 ms, OR 1.1 (95% CI 0.9 to 1.4); and > 500 ms, OR 1.0 (95% CI 0.8 to 1.3). Similar results were obtained when QT interval was corrected for heart rate by the Fridericia method.
DISCUSSION
This study confirms that QT prolongation is related to the presence and severity of LVSD, but this relation is due to QRS prolongation. Indeed, the JT interval shortened with increasing severity of LVSD, which may be an artefact caused by extension of the QRS interval into the start of repolarisation.
The association between QRS interval and the severity of LVSD may be due to: (1) increase in myocardial mass; (2) dilated ventricles, leading to longer activation pathways; and (3) altered electrical conduction. Dyssynchrony is more common in patients with longer QRS and may lead to worsening of the pre‐existing LVSD. Thus, QRS prolongation may reflect both the cause and consequence of LVSD.
It is surprising that use of β blockers was associated with shorter QRS and QTc intervals, as it is generally believed that β blockers have no effect on QRS duration at therapeutic doses. Hence, further studies are needed.
We acknowledge that this is only an observational study and the echocardiographic data were not validated. However, any potential error caused by these limitations is probably overcome by the large patient numbers.
In conclusion, the QRS interval appears to be the best ECG marker of the severity of LVSD.
Footnotes
Conflicting interests: none
References
- 1.Robbins J, Nelson J C, Rautaharju P M.et al The association between the length of the QT interval and mortality in the cardiovascular health study. Am J Med 2003115689–694. [DOI] [PubMed] [Google Scholar]
- 2.Dekker J M, Crow R S, Hannan P J.et al Heart rate corrected QT interval prolongation predicts risk of coronary heart disease in black and white middle aged men and women. The ARIC study. J Am Coll Cardiol 200443566–571. [DOI] [PubMed] [Google Scholar]
- 3.Brooksby P, Batin P D, Nolan J.et al The relationship between QT intervals and mortality in ambulant patients with chronic heart failure (UK‐HEART trial). Eur Heart J 1999201335–1341. [DOI] [PubMed] [Google Scholar]
- 4.Padmanabhan S, Silvet H, Amin J.et al Prognostic value of QT interval and QT dispersion in patients with left ventricular systolic dysfunction: results from a cohort of 2265 patients with an ejection fraction of < or = 40%. Am Heart J 2003145132–138. [DOI] [PubMed] [Google Scholar]
- 5.Cleland J G F, Swedberg K, Cohen‐Solal A.et al The Euro heart failure survey of the EUROHEART survey programme: a survey on the quality of care among patients with heart failure in Europe. Eur J Heart Fail 20002123–132. [DOI] [PubMed] [Google Scholar]