Vascular surgery is associated with a substantial risk of cardiovascular events and death.1,2 There is no effective method for determining cardiac risk preoperatively: validated risk prediction instruments are limited by complexity and poor predictive value, and other cardiac investigations such as nuclear stress testing and coronary angiography are limited by time and resources. For these reasons, alternative methods that can predict outcome of at risk patients would be an important advance.
Plasma brain natriuretic peptide (BNP) has counter‐regulatory vasodilator and natriuretic properties. Plasma BNP concentrations are often increased in cardiac disorders, such as angina and heart failure. The plasma concentrations of BNP are related to prognosis in these conditions.3 Many of these cardiovascular conditions occur in patients with peripheral vascular disease.
We investigated the predictive value of preoperative plasma BNP concentration for the occurrence of perioperative fatal or non‐fatal myocardial infarction (MI) in high risk vascular surgical patients. We also compared the predictive value of plasma BNP concentration with the Eagle score, a conventional surgical risk assessment instrument.1,2
METHODS
We screened consecutive patients undergoing major surgery for aortic or peripheral arterial occlusive disease in Gartnavel General Hospital, Glasgow, between April and September 2004. All patients at high risk, defined according to the American Society of Anesthesiology grade 3 (severe systemic disease without incapacitation) or 4 (severe incapacitating systemic disease with constant threat to life), were invited to participate in this study. A sample size (n = 40) had been calculated based on (1) an anticipated rate of fatal or non‐fatal MI of 10% at 48 hours; and (2) median (interquartile range) BNP concentrations in patients with or without cardiovascular disease who had participated in the North Glasgow MONICA (monitoring trends and determinants in cardiovascular disease) study.4 MI was defined by the presence of raised plasma cardiac biomarker concentrations (for example, serum troponin I > 0.2 μg/l) together with diagnostic changes on an ECG.
A blood sample was obtained preoperatively and postoperatively at 48 hours for measurement of troponin I and BNP concentrations. An ECG was also obtained at these time points. A cardiologist blinded to the study data compared the paired preoperative versus postoperative ECGs.
Continuous data were analysed by a Mann‐Whitney test. Categorical data were analysed by either a Pearson's χ2 test or a two tailed Fisher's exact test.
The study was approved by the hospital's ethics committee.
All patients underwent conventional preoperative work up, which included routine blood tests, an ECG, and a chest radiograph. Additional tests, such as echocardiography, were performed at the discretion of the surgical team.
An aliquot of venous blood, obtained from recumbent patients at the time of routine preoperative venesection (< 48 hours before surgery), was collected in EDTA and aprotinin 50 IU/ml (Trasylol; Bayer). These samples were centrifuged and stored at −20°C. BNP was detected with a standard radioimmunoassay.4 Samples were analysed in two batches at the conclusion of this study. The troponin I assay used was ADVIA Centaur (Bayer Diagnostics).
RESULTS
Forty one patients who were in American Society of Anesthesiology grade 3 or 4 were enrolled (table 1). Of these, 17 underwent lower limb bypass surgery, 11 had aortic surgery, and 13 had an amputation. In the first 48 hours postoperatively, four patients died of an acute MI and seven other patients experienced a non‐fatal MI, three of which were clinically silent. One patient died of sepsis.
Table 1 Cardiac event rate by case mix, risk factor, and brain natriuretic peptide (BNP) concentration.
| BNP (pg/ml) | Cardiac event rate | |||
|---|---|---|---|---|
| No* | χ2 | p Value | ||
| Case mix | ||||
| Sex | ||||
| Male | 60 | 7/27 (25.9%) | ||
| Female | 79 | 4/14 (28.6%) | 0.03 | 1.000 |
| Heart disease | ||||
| Absent | 50 | 5/24 (20.8%) | ||
| Present | 85 | 6/17 (35.3%) | 1.06 | 0.476 |
| β Blockers | ||||
| Used | 73 | 1/6 (16.7%) | ||
| Not used | 67 | 10/35 (28.6%) | 0.37 | 1.000 |
| Diabetes mellitus | ||||
| Absent | 44 | 7/30 (23.3%) | ||
| Present | 110 | 4/11 (36.4%) | 0.70 | 0.445 |
| Operation | ||||
| Amputation | 121 | 6/13 (46.2%) | ||
| Revascularisation | 41 | 3/17 (17.6%) | ||
| Aortic surgery | 60 | 2/11 (18.2%) | 3.62 | 0.163† |
| Eagle criteria‡ | ||||
| 0 | 19 | 0/12 (0%) | ||
| >0 | 93 | 11/29 (37.9%) | 6.22 | 0.018 |
| BNP (pg/ml) | ||||
| <100 | 0/27 (0%) | |||
| ⩾100 | 11/14 (78.6%) | 29.0 | 0.001 | |
| Risk factor | ||||
| Ischaemic heart disease | ||||
| Absent | <100 | 0/18 (0%) | ||
| ⩾100 | 5/6 (83.3%) | 18.95 | 0.001 | |
| Present | <100 | 0/9 (0%) | ||
| ⩾100 | 6/8 (75.0%) | 10.43 | 0.002 | |
| Eagle criteria | ||||
| 0 | <100 | 0/12 (0%) | ||
| ⩾100 | 0/0 | NA | NA | |
| >0 | <100 | 0/15 (0%) | ||
| ⩾100 | 11/14 (78.6%) | 18.99 | <0.001 | |
p Values derived from two tailed Fishers' exact test.
*The numerator indicates the number of patients who experienced a cardiac event and the denominator indicates the total number of patients who share an attribute (for example, seven of 27 men experienced a cardiac event); †p value derived from χ2.
‡The Eagle criteria are the cardiac risk factors diabetes, age >70 years, angina, previous myocardial infarction, and history of congestive heart failure.1
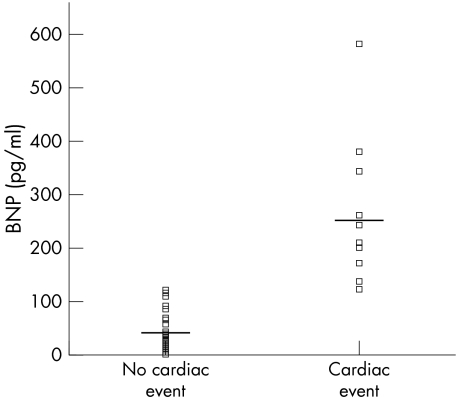
The median (interquartile range) plasma BNP concentration in patients who experienced a fatal or non‐fatal MI (n = 11) was 240 (172–344) pg/ml, compared with 39 (15–70) pg/ml in those who did not (n = 30) (fig 1). All patients who experienced an event had a preoperative BNP concentration > 120 pg/ml. BNP concentrations > 100 pg/ml had a greater predictive value than an Eagle score > 0 (receiver operating curve statistic for BNP 0.957 v Eagle 0.714, p < 0.001).
Figure 1 Brain natriuretic peptide (BNP) concentrations by cardiac event incidence. Median (interquartile range) BNP concentrations were 39 (15–70) pg/ml and 240 (172–344) pg/ml, p<0.001.
BNP concentrations were highly predictive of perioperative cardiac events irrespective of other variables. Although patients with a history of ischaemic heart disease were more likely to have higher BNP concentrations, a BNP concentration > 100 pg/ml was equally effective at identifying patients who were likely to have a cardiac event in both those with and those without a history of ischaemic heart disease (table 1). Similarly, in patients with an Eagle criterion > 0, BNP measurement effectively identified those at higher risk of a cardiac event. Compared with the Eagle scoring system, a BNP concentration of 100 pg/ml had similar sensitivity and negative predictive value (100% for both) for cardiac events but a superior specificity (90% v 40%) and a greater positive predictive value (78% v 38%).
DISCUSSION
We found that preoperative plasma BNP concentrations were increased in patients who subsequently experienced a perioperative fatal or non‐fatal MI. Plasma BNP concentration was not only highly predictive of these events but was also a more powerful predictor than a conventional risk prediction tool.
A history of ischaemic heart disease doubled the likelihood of a cardiac event, but only half of all patients who experienced an event had a history of ischaemic heart disease. Treatment with a β blocker reduced the likelihood of a cardiac event by one half. β Blocker use was associated with a lower event rate, in keeping with the cardioprotective role of these drugs.
In the recent coronary artery revascularisation prophylaxis trial 510 patients with obstructive coronary artery disease and an indication for vascular surgery were randomly assigned to coronary revascularisation before surgery or to conventional management. Perhaps surprisingly, coronary revascularisation did not confer any survival advantage.5 This result illustrates the complexity of risk management in high risk surgical patients and underscores the need for further investigations in this area.
We believe that our research will be of interest to a wide range of clinicians who manage surgical patients. Our data suggest that a single blood BNP measurement may predict risk in this, and potentially other, surgical settings. Our thesis requires validation in a larger population of patients. If reproduced, these findings may enhance the cost effectiveness of interventions in patients with disease requiring surgery.
References
- 1.Eagle K A, Berger P B, Calkins H.et al ACC/AHA guideline update for perioperative cardiovascular evaluation for noncardiac surgery: executive summary. A report of the American College of Cardiology/American Heart association task force on practice guidelines (committee to update the 1996 guidelines on perioperative cardiovascular evaluation for noncardiac surgery). Circulation 20021051257–1267. [PubMed] [Google Scholar]
- 2.Eagle K A, Coley C M, Newell J B.et al Combining clinical and thallium data optimizes preoperative assessment of cardiac risk before major vascular surgery. Ann Intern Med 1989110859–866. [DOI] [PubMed] [Google Scholar]
- 3.Wang T J, Larson M G, Levy D.et al Plasma natriuretic peptide levels and the risk of cardiovascular events and death. N Engl J Med 2004350655–663. [DOI] [PubMed] [Google Scholar]
- 4.McDonagh T A, Cunningham A D, Morrison C E.et al Left ventricular dysfunction, natriuretic peptides, and mortality in an urban population. Heart 20018621–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McFalls E O, Ward H B, Moritz T E.et al Coronary artery revascularization before elective major vascular surgery. N Engl J Med 20043512795–2804. [DOI] [PubMed] [Google Scholar]