Intracardiac echocardiography (ICE) has emerged as an adjunctive tool during electrophysiological procedures. The objective of this study was to validate ICE for assessing atrial mechanical function in patients with atrial fibrillation (AF) by comparing the parameters of atrial mechanical function assessed by transoesophageal echocardiography (TOE) versus ICE.
METHODS
This study enrolled 23 patients (20 men; mean (SD) age 56 (12) years) undergoing ablation of symptomatic drug refractory AF: 11 patients with paroxysmal and 12 with persistent AF of > 6 months' duration. The left anteroposterior atrial size was 45 (8) mm and left ventricular ejection fraction was 63 (13)%. All patients were prospectively enrolled after providing written informed consent.
TOE was performed on the day of the ablation procedure with a Hewlett Packard Sonos 2500 or 5000 or an Acuson Sequoia workstation connected to a multiplane 5–7.5 MHz probe. ICE imaging was performed at the start of the ablation procedure. A 10 French ICE catheter with a 5–10 MHz probe was connected to an Acuson Sequoia workstation. In five patients without adequate imaging of the left atrial appendage (LAA) from the right atrium, the catheter was advanced into the left atrium through a patent foramen ovale or a transseptal puncture. All parameters were measured according to established clinical laboratory practice and were recorded on videotape or digitally for offline analysis.
The following parameters were determined by TOE and ICE: LAA emptying velocity (LAAEV); maximum mitral E wave velocity; left atrial spontaneous echo contrast grade (LASEC); and left pulmonary vein (PV) diameter. Maximum LAAEV was assessed with pulsed wave Doppler by placing the sample volume 1 cm into the mouth of the LAA, with the Doppler beam parallel to LAA longitudinal axis. Maximum E wave velocity was measured by positioning the sample volume at the tip of the leaflets of the mitral valve, with the Doppler beam perpendicular to the atrioventricular valve plane. Measurements were averaged over 20 consecutive cycles. LASEC was graded on a scale of 0 to 4 according to previously published criteria and was assessed independently by two observers with differences resolved by consensus.1 PV diameter was measured at the ostium of each left vein and defined as the intersection of a line that extends from the contour of the left atrium to the PV and the contour of the PV to the left atrium. The right veins were not assessed because they could not be delineated consistently with TOE.
Continuous variables are expressed as mean (SD). Correlations between continuous variables were determined with Pearson's correlation coefficients and linear regression. In addition the limits of agreement between the two techniques were calculated for each variable by the statistical technique described by Bland and Altman.2 For agreement of the ordinal variable LASEC the Kendall's τb test was used. Significance was established at p < 0.05.
RESULTS
The left atria of all patients were successfully imaged by TOE and ICE. All parameters of atrial mechanical function were determined in all patients, whereas PV diameter was measured in 12 patients. Images were recorded during AF in 19 patients and sinus rhythm in four patients. Five patients required imaging from within the left atrium to obtain acceptable image quality.
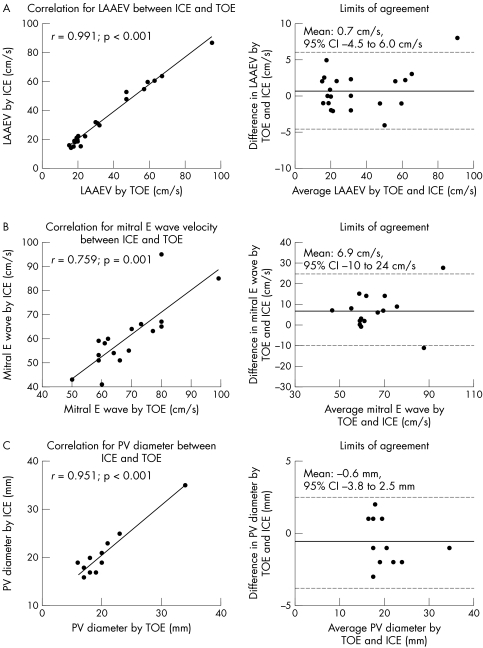
LAAEV was 34 (21) and 35 (22) cm/s by ICE and TOE, respectively. The correlation between TOE and ICE for measurement of LAAEV was highly significant with excellent test agreement (r = 0.991, p < 0.001, mean difference 0.7 cm/s, limits of agreement −4.5 to 6.0 cm/s; fig 1A).
Figure 1 On the left side the correlation for the assessed variables is shown; on the right side the limits of agreement determined by the Bland‐Altman method. The average of measurements by transoesophageal echocardiography (TOE) and intracardiac echocardiography (ICE) are plotted against their difference. The lines represent the 95% confidence intervals (CI) for measurement by the two techniques. (A) Left atrial appendage emptying velocity (LAAEV); (B) Mitral E wave velocity; (C) Pulmonary vein (PV) diameter.
Mitral E wave velocity was 62 (12) and 69 (14) cm/s by ICE and TOE, respectively. The correlation between TOE and ICE was strong (r = 0.759, p = 0.001) with good agreement (mean difference 6.9 cm/s, limits of agreement −10.5 to 24.3 cm/s) (fig 1B).
LASEC was observed only in patients with persistent AF; all patients with paroxysmal AF had a LASEC score of 0. The median observed values were 0 (range 0–2) and 0 (range 0–3) by TOE and ICE, respectively. Good correlation and agreement were found between the two methods (r = 0.821, p = 0.009).
The PV diameter was determined in the left PVs. Mean diameter was 20.9 (5.4) and 20.3 (5.0) mm by ICE and TOE, respectively. A strong correlation and excellent agreement were found between ICE and TOE (r = 0.951, p < 0.001, mean difference −0.6 mm, limits of agreement −3.8 mm to 2.5 mm; fig 1C).
DISCUSSION
The present study validates the use of ICE for the evaluation of atrial mechanical function during catheter ablation of AF. ICE was validated in comparison with TOE as the ideal.3 LAAEV, mitral inflow velocity, and visualisation of spontaneous echo contrast and PV diameter had highly significant correlation and excellent agreement. Furthermore, we showed that ICE imaging from the left atrium is feasible and offers superior image quality for visualisation and measurements of the left atrium.
LAAEV has been clinically used to evaluate atrial mechanical stunning and the recovery of atrial function after cardioversion of atrial flutter and fibrillation.4 It is a strong parameter representative of atrial mechanical function and has been shown together with LASEC to be an excellent predictor of thrombus formation and stroke in patients with atrial arrhythmias.1
Previous studies of ICE have focused on visualisation of anatomical details to guide interventional approaches. Morton et al5 assessed atrial mechanical function in patients undergoing ablation of cavotricuspid isthmus dependent atrial flutter. The study evaluated patients during regular tachycardia or sinus rhythm and observed a strong correlation for LAAEV, LAA fractional area change, and PV and mitral valve Doppler flow velocities. However, atrial function during a more disorganised and chaotic rhythm may be different. In addition, parameters such as Doppler A wave or fractional area change cannot be extrapolated to AF.
The accurate determination of atrial mechanical function by ICE imaging further enhances its usefulness during catheter ablation of AF. Real time assessment of left atrial function may be used to monitor the impact of extended ablation procedures on mechanical function, allowing further insights into pathophysiological changes after ablation. These observations may have an impact on anticoagulation policies.
ACKNOWLEDGEMENTS
This study was partly funded by an unrestricted educational grant from Siemens Medical, Mountain View, California, USA. Dr Rotter is supported by the Swiss National Foundation for Scientific Research, Bern, Switzerland. Dr Sanders is supported by the Neil Hamilton Fairley Fellowship from the National Health and Medical Research Council of Australia and the Ralph Reader Fellowship from the National Heart Foundation of Australia. Dr Rostock is supported by the German Cardiac Society.
Abbreviations
AF - atrial fibrillation
ICE - intracardiac echocardiography
LAA - left atrial appendage
LASEC - left atrial spontaneous echo contrast grade
PV - pulmonary vein
Footnotes
No author has any conflict of interest to disclose
Presented in part at the European Society of Cardiology Congress 2004, Munich, Germany. Published in Abstract form in Eur Heart J 2004;25(Abstract suppl), no 482.
References
- 1.Fatkin D, Kelly R P, Feneley M P. Relations between left atrial appendage blood flow velocity, spontaneous echocardiographic contrast and thromboembolic risk in vivo. J Am Coll Cardiol 199423961–969. [DOI] [PubMed] [Google Scholar]
- 2.Bland J M, Altman D G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet . 1986;i307–310. [PubMed]
- 3.Garcia‐Fernandez M A, Torrecilla E G, San Roman D.et al Left atrial appendage Doppler flow patterns: implications on thrombus formation. Am Heart J 1992124955–961. [DOI] [PubMed] [Google Scholar]
- 4.Sanders P, Morton J B, Kistler P M.et al Reversal of atrial mechanical dysfunction after cardioversion of atrial fibrillation: implications for the mechanisms of tachycardia‐mediated atrial cardiomyopathy. Circulation 20031081976–1984. [DOI] [PubMed] [Google Scholar]
- 5.Morton J B, Sanders P, Sparks P B.et al Usefulness of phased‐array intracardiac echocardiography for the assessment of left atrial mechanical “stunning” in atrial flutter and comparison with multiplane transesophageal echocardiography. Am J Cardiol 200290741–746. [DOI] [PubMed] [Google Scholar]