Abstract
Objective
To conduct a one year follow up study of patients seen in a combined rapid access chest pain, arrhythmia and heart failure clinic.
Methods
Local general practitioners, accident and emergency department clinicians and other hospital clinicians were invited to refer patients with a new presentation of chest pain, palpitations and suspected cardiac‐induced breathlessness to the rapid access cardiology clinics at Charing Cross Hospital, London, on a one‐stop, no appointment basis. Consent to be followed up by a postal questionnaire one year later was sought from all patients attending between 1 November 2002 and 31 October 2003.
Results
1223 patients were seen in the 12 month study period. 940 (77%) consented to one year follow up. 216 (23%) patients had a diagnosis of definite cardiac, 621 (66%) of not cardiac and 103 of possible cardiac disease (11%). 98% of patients diagnosed “not cardiac” did not receive a diagnosis of cardiac disease over the following 12 months. Of patients with diagnosed definite cardiac disease, one year cardiac mortality was 7 of 216 (3%), compared with an age‐ and sex‐matched expected cardiac mortality of 0.9% (standardised mortality ratio 3.5, 95% confidence interval (CI) 1.4 to 7.2). For patients with an initial diagnosis of possible or not cardiac disease, cardiac mortality at one year was 0.3% compared with an expected cardiac mortality of 0.4% (standardised mortality ratio 0.8, 95% CI 0.1 to 2.8).
Conclusions
A rapid access cardiology clinic accurately diagnoses and risk stratifies patients into those with cardiac disease at high risk of cardiac death and those without significant cardiac disease.
Keywords: arrhythmia, chest pain, heart failure, rapid access clinic
Rapid access chest pain clinics (RACPCs) were identified as the model of choice for the assessment of patients presenting with suspected angina in March 2000 as part of the National Service Framework for coronary heart disease.1 By April 2002, the number of RACPCs to greatly exceeded the original expected number of 100 nationwide.
Extrapolating from the experience of RACPCs to the symptoms of palpitations and cardiac‐related breathlessness we have developed rapid access arrhythmia (RAAC)2 and heart failure clinics (RAHFC).3,4 In the same way as an RACPC determines whether the symptom chest pain indicates ischaemia, an RAAC or RAHFC determines whether palpitations or syncope and breathlessness indicate a significant arrhythmia or heart failure, respectively. Uniquely, since February 2002 an NHS funded rapid access cardiology service has been open each weekday at Charing Cross Hospital in west London.
The aim of rapid access cardiology is that first presentations of suspected cardiac disease are identified, diagnosed and risk stratified promptly. If a positive diagnosis is made, effective management is initiated immediately.
Support for such diagnostic clinics is provided not only in the original National Service Framework for coronary heart disease but also in the recently published additional chapter 8 on arrhythmias,1 which recommends the establishment of RAACs. The National Institute for Health and Clinical Excellence (NICE) guidelines on heart failure also recommend that specialist diagnostic clinics be set up.5
Data on the effectiveness of rapid access cardiology services are limited, however. Much of what is known applies to RACPCs. There are no randomised trials, only reports from observational cohorts from (often academically staffed and funded) chest pain clinics.4,6,7,8,9,10,11,12,13 Even fewer reports provide the evidence base for arrhythmia and heart failure clinics.2,3,4 Although the case for a service model that prioritises prompt diagnosis and effective management has been strongly advocated, several publications have highlighted the need for a study evaluating long term follow up of patients seen in rapid access clinics.14,15,16
We performed a prospective observational study to assess whether a rapid access cardiology service effectively evaluates patients presenting with suspected cardiac disease and identifies patients at high risk.
METHODS
Charing Cross Hospital, situated in west London, is a teaching hospital with secondary care services for cardiology in the catchment area of Hammersmith and Fulham Primary Care Trust with a population of 165 000.
The rapid access cardiology service is open every weekday morning from 09 30 to 12 30.
The core team consists of a specialist registrar‐grade clinical fellow (JT) supported by specialist registrars who take the lead on patients presenting with suspected heart failure or arrhythmias, a senior nurse at an F or G grade level who takes the lead on patients presenting with suspected angina, with a physiologist and overall consultant supervision (KF).
Referrals to the clinic are invited from local general practitioners, the hospital accident and emergency department and other hospital specialties.
The criteria for referral are a suspected first presentation of chest pain thought to be caused by stable angina; palpitations or a syncopal episode thought to be caused by a significant arrhythmia; and breathlessness thought to be caused by heart failure. Referrers are asked to provide a referral letter, which is faxed, emailed or brought to the cardiology department by the patient. In some cases where referrers send a referral letter to the cardiology department first, for example, to seek advice as to whether a rapid access referral is appropriate, an invitation letter is sent to the patient asking him or her to attend at their next opportunity.
No appointments are needed. Patients are seen on the day of attendance, which in most cases is also the day of referral. Patients are encouraged to attend before 10 30 when possible.
The clinic operates on a one‐stop principle, integrating the clinical assessment with relevant non‐invasive investigations into a single assessment.
All patients have a history taken, examination performed, and appropriate investigations initiated. All patients attending the chest pain clinic are discussed with or seen by the physician. Investigations available are treadmill exercise testing, echocardiography, blood tests including full blood count, creatinine, urea and electrolytes, liver function tests, thyroid function tests if appropriate, random (or if required, fasting) cholesterol and glucose, near‐patient B‐type natriuretic peptide (Biosite Ltd, Belfast, UK; normal cut off < 100 pg/ml), near‐patient troponin T(Biosite Ltd) (normal range < 0.1 μg/l) and Holter monitoring (24 h, 48 h, or 7 day event monitoring).
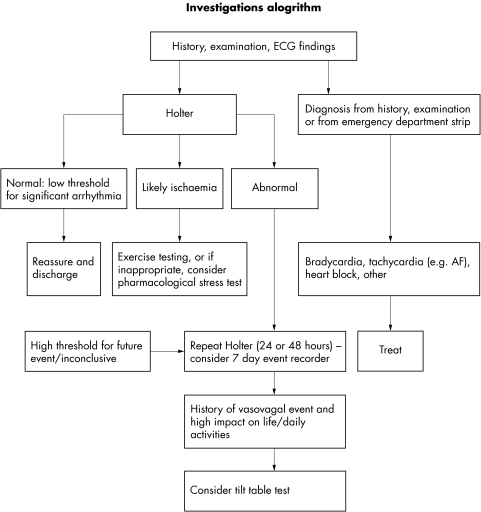
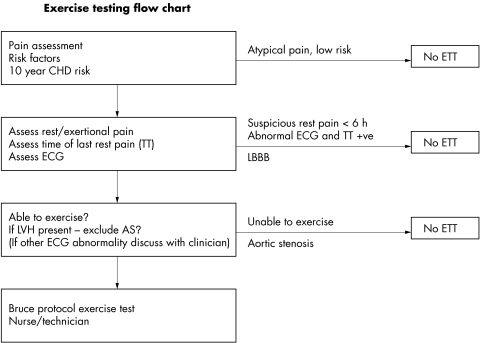
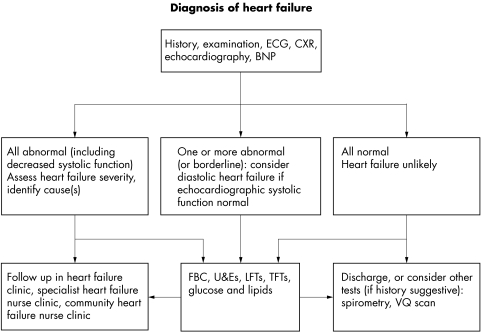
Myocardial perfusion scintigraphy and dobutamine stress echocardiography are available although not necessarily performed on the day of attendance. Arterial blood gases, ventilation perfusion scanning and multiple gated acquisition scanning are also available as needed. Figures 1–3 show protocols for diagnostic pathways for the three types of clinics.
Figure 1 Investigation algorithm for rapid access cardiology clinics. AF, atrial fibrillation.
Figure 2 Exercise testing algorithm for rapid access cardiology clinics. AS, aortic stenosis; CHD, coronary heart disease; ETT, exercise tolerance test; FBC, full blood count; LBBB, left bundle branch block; LVH, left ventricular hypertrophy; TT, troponin T.
Figure 3 Heart failure diagnosis algorithm for rapid access cardiology clinics. BNP, B‐type natriuretic peptide; CXR, chest x ray; FBC, full blood count; LFTs, liver function tests; TFTs, thyroid function tests; U&Es, urea and electrolytes; VQ, ventilation perfusion scintigraphy.
Descriptive statistical analysis was used. Data were analysed with SPSS for Windows V.11.5 and STATA V.8.2.
When possible, a definitive diagnosis is made by the end of the assessment and appropriate treatment is initiated. Patients with a diagnosis of exertional angina start treatment with aspirin, a β blocker and a statin unless these are contraindicated. Patients with heart failure start a diuretic and an angiotensin converting enzyme (ACE) inhibitor (unless contraindicated). Patients with atrial fibrillation start warfarin (or aspirin) unless contraindicated, with or without rate control, and antiarrhythmics and other arrhythmias are managed according to the specific diagnosis and mode of presentation.
The minority of patients who need further follow up either with a definitive diagnosis pending or for management are given appointments in the appropriate general or subspecialty cardiology clinic.
A Microsoft Access database is used to record individual patient data as well as to generate written communication back to the referrer.
Patient consent
Informed written consent for the study was obtained from patients (or from a relative or friend on their behalf) participating in the study. Ethics approval was obtained from Riverside Research Ethics Committee (reference RREC 3194).
Diagnosis
Three main categories and two minor categories of diagnosis were used:
Definite cardiac disease: a positive diagnosis of exertional angina, significant arrhythmia or heart failure is made at the end of the initial presentation to the relevant rapid access clinic. This also comprises “other cardiac” (see below).
Not cardiac disease: a diagnosis of exertional angina, significant arrhythmia or heart failure is ruled out at the end of the initial presentation. This also comprises “other non‐cardiac” (see below).
Possible cardiac disease: the clinician is unsure of the diagnosis or is awaiting the results of further investigations before making a definitive positive or negative diagnosis at the end of the initial presentation.
Other cardiac disease: a positive diagnosis of cardiac disease is made but in a clinic other than one that would normally be regarded as appropriate—for example, a diagnosis of exertional angina when a patient presents to the RAHFC with breathlessness. This category also includes other cardiac diagnoses when the patient has been referred to the appropriate clinic—for example, a diagnosis of severe aortic stenosis when a patient presents to the RACPC with exertional chest pain.
Other non‐cardiac disease: a non‐cardiac but significant other medical diagnosis is made that obviously explains the patient's symptoms, such as significant anaemia in a patient presenting with breathlessness.
Below is a summary of cardiac definitions used in this study:
Heart failure: symptoms of breathlessness, lethargy or fluid retention with evidence of a cardiac abnormality.17 Evidence includes echocardiographic data such as abnormal systolic or diastolic or valvular abnormalities or raised B‐type natriuretic peptide concentrations5;
Angina18: exertional angina; symptoms of myocardial ischaemia at rest or minimal exertion if troponin T is negative (< 0.1 μg/l) more than 12 h after the onset of chest pain;
Significant arrhythmia.
For this study the following arrhythmias were defined as significant (on the basis of their clear pathological and adverse prognosis in terms of cardiac morbidity and mortality):
Atrial fibrillation (sustained/persistent or paroxysmal);
Atrial flutter (sustained or paroxysmal);
Supraventricular tachycardia;
Atrioventricular re‐entrant tachycardia;
Atrioventricular re‐entrant nodal tachycardia;
Wolff–Parkinson–White syndrome;
Atrial tachycardia;
Complete heart block;
Second‐degree heart block (symptomatic);
Sinus node disease: evidence of symptomatic sinus bradycardia with no obvious cause such as drug induced with or without intermittent tachycardia.
Follow up
Vital status of consenting patients was sought from the Office for National Statistics (ONS). Data from hospital systems, hospital notes and records were also collated.
Each consenting patient's general practitioner was sent a short questionnaire inquiring about the subsequent diagnosis of a cardiovascular event (myocardial or cerebral infarct, angina, atrial fibrillation or heart failure) and vital status of the patient. Concurrently, patients were sent a longer postal questionnaire one year after their attendance at the rapid access clinic inquiring about their symptoms, investigations and procedures, use of primary and secondary care resources, drug treatment and comments on the rapid access clinic.
Data collected from patients and general practitioners were corroborated with data from hospital data systems, patient notes and returns from the ONS. Data acquired were collated and reviewed by one clinician (JT). A 10% sample of the collated patient data was reviewed and validated by a second clinician (KF).
Initial diagnosis denotes the diagnosis made at the end of the rapid access consultation, whereas final diagnosis denotes diagnosis made at the end of further investigations—for example, angiography censored at one year after the initial presentation at the rapid access clinic.
Vital status of patients was recorded at one year after attendance at the rapid access clinic. Cardiac death and non‐cardiac death were defined by the primary diagnosis or cause of death as stated on the death certificate (section 1 categorised by the International classification of diseases, 10th revision).
RESULTS
Between 1 November 2002 and 31 October 2003, 1223 patients (46.1% men) were seen in the rapid access clinics. The age range of patients was 17–99 years, with a mean of 57.6 years. One hundred and thirty were seen in the RAHFC, 499 in the RAAC and 594 in the RACPC. Of these, 940 (77%) consented to participate in the study, of whom 107 were seen in the RAHFC (that is, 82% of patients presenting to the RAHFC consented), 425 in the RACPC (72%) and 408 (82%) in the RAAC.
Of the 940 consenters, 487 (52%) returned completed questionnaires. Data on use of primary care resources were obtainable for 867 (92%) of consenting patients from the questionnaires completed by general practitioners. Data on use of secondary care resources were available for all responders and consenting non‐responders who attended our centre for cardiac or other clinics and from admissions (80% of the cohort of 940 patients lived within the catchment area of the primary care trust).
Mortality data were available for 931 of 940 (99%) patients. Nine patients were untraceable by the ONS due to, for example, emigration.
Non‐consenters did not differ significantly from consenters in terms of sex, age, race and postcode but were more likely to have an initial diagnosis of possible cardiac disease (p = 0.002) and to have been referred from an accident and emergency department (p < 0.001).
Positive predictive value of investigations undertaken at rapid access clinics
Of 425 RACPC patients, 225 (53%) had an exercise tolerance test, 42 (19%) of which were abnormal. Of 46 patients with a final diagnosis of angina who had an exercise tolerance test, 30 (65%) had abnormal results—that is, the positive predictive value (PPV) of the exercise tolerance test was 65%. Fifty four patients (13%) had a non‐invasive investigation of ischaemia (myocardial perfusion scintigraphy or stress echocardiography), 22 (41%) of which were abnormal. The PPV was 95% (19 of 20). Forty nine (12%) patients underwent coronary angiography, with 36 (73%) showing significant ischaemia. PPV of coronary angiography was 97% (33 of 34).
Of 408 RAAC patients, 240 (59%) underwent ambulatory Holter monitoring. Of these, 19 (8%) showed a significant arrhythmia. The PPV was 56% (18 of 32).
Of 107 RAHFC patients, 48 (45%) had B‐type natriuretic peptide tests, 18 (38%) of which were abnormal. PPV was 100% (11 of 11). Ninety seven (91%) had echocardiography; 29 (30%) had ECGs deemed consistent with impaired systolic or diastolic function. PPV was 88% (22 of 25).
Table 1 shows the initial diagnoses made at each rapid access clinic.
Table 1 Initial diagnosis by type of rapid access clinic.
| Initial diagnosis | Type of clinic | ||
|---|---|---|---|
| RACPC (n = 425) | RAAC (n = 408) | RAHFC (n = 107) | |
| Definite cardiac | 35 (8%) | 110 (27%) | 25 (23%) |
| Exertional angina (35) including 2 ACS | Sustained AF (45), paroxysmal AF (40), atrial flutter (3), SVT/WPW/AVRT/AVNRT (14), complete heart block (3), second‐degree heart block (1), sinus node disease (4) | Heart failure (25) | |
| Possible cardiac | 67 (16%) | 26 (6%) | 10 (10%) |
| Not cardiac | 310 (73%) | 233 (57%) | 59 (55%) |
| Other cardiac | 11 (3%) | 22 (6%) | 13 (12%) |
| SVT/AF (2), valvular heart disease/congenital (5), suspected heart failure (2), hypertension (2) | Sinus bradycardia (3), valvular heart disease/congenital (2), suspected heart failure (1), hypertension (5), suspected CAD (11) | SVT/AF(2), valvular heart disease/congenital (1), suspected CAD (3), hypertension (7) | |
| Other non‐cardiac | 2 (<1%) | 17 (4%) | |
| Anaemia (1), other (1) | Anaemia (1), vasovagal syncope (3), TIA (3), micturition/unexplained/neurogenic syncope (6), other4 | ||
ACS, acute coronary syndrome; AF, atrial fibrillation; AVNRT, atrioventricular nodal re‐entrant tachycardia; AVRT, atrioventricular re‐entrant tachycardia; CAD, coronary artery disease; RAAC, rapid access arrhythmia clinic; RACPC, rapid access chest pain clinic; RAHFC, rapid access heart failure clinic; SVT, supraventricular tachycardia; WPW, Wolff–Parkinson–White syndrome; TIA, transient ischaemic attack.
The diagnosis was definite cardiac disease for 216 (23%) patients, non‐cardiac disease for 621 (66%) and possible cardiac disease for 103 (11%).
Positive and negative predictive values of a rapid access clinic initial diagnosis
Table 2 shows the positive and negative predictive values of a rapid access clinic diagnosis at initial presentation.
Table 2 Positive and negative predictive values of a rapid access clinic diagnosis at initial presentation.
| Initial diagnosis | Final diagnosis (1 year) | |||
|---|---|---|---|---|
| Definite cardiac | Possible cardiac | Not cardiac | Total | |
| Definite cardiac | 164 | 1 | 51 | 216 |
| Possible cardiac | 29 | 14 | 60 | 103 |
| Not cardiac | 13 | 2 | 606 | 621 |
| Total | 186 | 17 | 717 | 940 |
Positive predictive value 76% (164/216); negative predictive value 98% (606/621).
Just 15 of 621 patients (2%) with a diagnosis of non‐cardiac disease at the initial assessment had cardiac disease diagnosed over the ensuing 12 months. Most patients (89 of 103; 86%) with possible cardiac disease had this modified to not cardiac or definite at the end of the 12 month follow up.
Mortality at one year
Table 3 shows vital status of study patients, grouped according to initial diagnosis and compared with the age‐ and sex‐matched expected cardiac mortality based on general population cardiac mortality data for England and Wales during 2003.19
Table 3 Cardiac mortality by initial diagnosis.
| Vital status | Initial diagnosis | |||
|---|---|---|---|---|
| Definite cardiac | Possible cardiac | Not cardiac | Total | |
| Alive | 202 (93.5%) | 99 (96.1%) | 606 (97.5%) | 907 (97%) |
| Cardiac death (all 3 clinics) | 7 (3.3%) | 0 | 2 (0.3%) | 9 (1%) |
| RACPC | 2 (4.3%) | 0 | 0 | 2 (4.3%) |
| RAAC | 1 (0.8%) | 0 | 0 | 1 (0.8%) |
| RAHFC | 4 (10.5%) | 0 | 2 (3.4%) | 6 (13.9%) |
| Non‐cardiac death | 5 (2.3%) | 2 (1.9%) | 6 (1%) | 13 (1.8%) |
| Unknown cause of death | 0 | 1 (1%) | 1 (0.2%) | 2 (0.2%) |
| Unknown vital status | 2 (0.9%) | 1 (1%) | 6 (1%) | 9 (1%) |
| Total | 216 (100%) | 103 (100%) | 621 (100%) | 940 (100%) |
| Expected cardiac mortality based on general population data | 2 (0.9%) | 0.6 (0.6%) | 2.4 (0.4%) | 5 (0.6%) |
RAAC, rapid access arrhythmia clinic; RACPC, rapid access chest pain clinic; RAHFC, rapid access heart failure clinic.
Patients with diagnosed cardiac disease had a threefold greater cardiac mortality than age‐ and sex‐matched controls. Patients with a not cardiac diagnosis had a trend towards a lower one‐year cardiac mortality than their age‐ and sex‐matched controls.
DISCUSSION
These data show that a rapid access cardiology service is an effective way of risk stratifying patients who present with cardiac symptoms into those with and without cardiac disease and at low or high cardiac risk. This is the first study to evaluate outcomes and prognosis in a cohort of patients seen in a combined rapid access cardiology clinic setting.
The first principle of this service was to establish an accurate diagnosis.
Our definitions of angina and heart failure are based on the recommendations of the European Society of Cardiology and NICE guidelines for the diagnosis of heart failure. The concept of diastolic heart failure is included as a positive diagnosis of heart failure where current diagnostic criteria for diastolic heart failure are met and no other cause is identified for the patient's symptoms. One possible limitation of this study (but a problem of overdiagnosis) is therefore related to the current controversy surrounding diastolic heart failure.
Given the seriousness of cardiac disease it is essential that patients not be falsely reassured. A key finding is therefore that a rapid access cardiology assessment of not cardiac disease had a 98% negative predictive value for the development of a cardiac diagnosis in the ensuing 12 months. The second principle of the service, closely linked but not identical to the first, was to identify patients at high risk of cardiac death. The patient group with diagnosed cardiac disease had a cardiac mortality 10‐fold greater than that of patients with a non‐cardiac diagnosis and threefold greater than that of cohort age and sex matched to the definite group. The standardised mortality ratio for patients with a diagnosis of cardiac disease was 3.5 (95% CI 1.4 to 7.2). The lower mortality of the not cardiac group than of an age‐ and sex‐matched cohort did not reach significance but suggests that a reassuring rapid access clinic outcome predicts a low mortality. Overall these data provide evidence of effective risk stratification.
The model on which this study is based is necessarily not a randomised trial. A trial of RACPCs, now a National Service Framework‐recommended and established part of secondary‐care cardiology service provision, is ethically dubious, and a trial of rapid access cardiology would not be complete without an RACPC component.
In terms of other limitations to the generalisability of this study, the non‐consenters tended to be referred from the accident and emergency department rather than by their general practitioner, and were more likely at initial presentation to have a diagnosis of possible cardiac disease than of definite or non‐cardiac disease. The differences between consenters and non‐consenters, however, were not significant in terms of age, sex, residential postcode or race. A substantial part of the effort in this study was aimed at determining the patients' diagnostic status at one year. So, although only 52% returned questionnaires (comparable with other similar reports), it is important to note that the final diagnosis was not reliant on returning the questionnaire but was based on information from the general practitioner and hospital systems combined with submitted questionnaire data. Vital status was completely established through ONS registration.
The initial diagnosis was purposely left as the diagnosis made by the person seeing the patient in the clinic. This specifically assesses clinic operation in the real world. In fact all clinic data are reviewed by a consultant cardiologist as part of a clinical governance programme. For these reasons we did not use an initial diagnosis validated by a panel of experts only available to research cohorts. The final diagnosis was based on evidence from diagnostic investigations and specialist assessments where appropriate. It is of course possible that these final diagnoses were incorrect but it was not feasible or appropriate to thoroughly assess and reinvestigate the 940 patients at one year, nor would this have enhanced the generalisability of our results. One potential gap was patients with a diagnosis subsequently made at a distant hospital. Patients had chosen to come to our centre for their initial assessment, however, and logically the great majority would return to our hospital subsequently. Furthermore, this would still not be a problem as long as either the general practitioner or the patient alerted us to the new diagnosis in the one year questionnaire, further diminishing the importance of this potential source of error.
The feasibility of extending the concept of RACPCs seems clear. The advantage of a rapid access cardiology service as opposed to three distinct rapid access clinics is illustrated by the inclusion of patients who, while referred to one subgroup of the service (such as chest pain), ultimately had cardiac disease diagnosed but within another subgroup (such as heart failure). As table 1 shows, 3%, 6% and 12% of patients seen in the RACPC, RAAC and RAHFC, respectively, had a crossover diagnosis. We believe that patients present across the spectrum of cardiac disease. Subgrouping them according to chest pain or heart failure or arrhythmias is artificial and may be detrimental to disease diagnosis, particularly on referral to the RAHFC, where up to 12% of patients may have a relevant other cardiac diagnosis.
The service was established by a re‐engineering rather than a substantial expansion of cardiac services and we believe this is widely applicable. Details such as the role and use of nurse practitioners or general practitioners with a special interest in cardiology may vary. The overall resources and organisation required to operate a rapid access cardiology service are available to cardiology departments, particularly in collaboration with primary care and the developing cardiac networks.
Rapid access cardiology has been developed to be an improved service for patients and general practitioners but also because it is likely, but not proved, that early intervention improves outcomes. The risk of myocardial infarction, coronary artery bypass grafting or death from coronary heart disease is known to be 30% in new cases of exertional angina that occurs within the first 12 months of diagnosis.7 In traditional cardiology outpatient settings, the wait for a first appointment was usually at least 8–18 weeks8 and further visits for investigations usually delayed the initiation of a management strategy to around 12 months. Hence, most cardiac events may occur before definitive diagnosis if previous models of care are followed. ACE inhibitors improve morbidity and mortality in patients with heart failure20 but may also cause side effects. It is reasonable to assume that accurate diagnosis and prompt initiation of an ACE inhibitor is advantageous. For patients with new onset atrial fibrillation the risk of stroke is maximal early after development of the arrhythmia21 and it seems similarly logical that early anticoagulation or restoration of sinus rhythm would reduce adverse events. Rapid access services may be applicable beyond cardiology. Suitable conditions for this model of care are those that are common and difficult to diagnose in primary care but whose outcome may be improved in the short term by prompt diagnosis and initiation of known effective treatments.
Conclusion
This study shows that a rapid access cardiology service for the assessment of patients presenting with suspected cardiac disease accurately identifies cardiac disease and patients with non‐cardiac symptoms. Furthermore, a rapid access cardiology service effectively risk stratifies patients according to high or low cardiac mortality at 12 months.
Abbreviations
ACE - angiotensin converting enzyme
NICE - National Institute for Health and Clinical Excellence
ONS - Office For National Statistics
PPV - positive predictive value
RAAC - rapid access arrhythmia clinic
RACPC - rapid access chest pain clinic
RAHFC - rapid access heart failure clinic
Footnotes
Support: Coronary Heart Disease (CHD) collaborative.
Conflicts of interest: None declared.
Ethics: Riverside Research Ethics Committee approved.
References
- 1.Department of Health The National Service Framework for coronary heart disease. London: Department of Health, 2000
- 2.Martins J L, Fox K F, Wood D A.et al A rapid access arrhythmia clinic for the diagnosis and management of arrhythmias in the population. Heart 200285(suppl I)i21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fox K F, Cowie M R, Wood D A.et al A rapid access heart failure clinic provides a prompt diagnosis and appropriate management of new heart failure presenting in the community.Eur J Heart Fail 20002423–429. [DOI] [PubMed] [Google Scholar]
- 4.Cowie M R, Wood D A, Coats A J.et al Survival of patients with a new diagnosis of heart failure: a population study.Heart 200083505–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Institute for Health and Clinical Excellence Chronic heart failure: national clinical guideline for diagnosis and management in primary and secondary care. NICE guideline no 5. London: Royal College of Physicians, 2003, http://www.nice.org.uk/pdf/Full_HF_Guideline.pdf (accessed 1 Feb 2006)
- 6.Jain D, Fluck D, Sayer J W.et al One stop chest pain clinic can identify high cardiac risk. J R Coll Physicians Lond 199731401–404. [PMC free article] [PubMed] [Google Scholar]
- 7.Ghandi M M, Lampe F C, Wood D A. Incidence, clinical characteristics and prognosis of angina pectoris. Br Heart J 199573193–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dougan J P, Mathew T P, Riddell J W.et al Suspected angina pectoris: a rapid‐access chest pain clinic. Q J M 200194679–686. [DOI] [PubMed] [Google Scholar]
- 9.McManus R J, Mant J, Davies A K.et al A systematic review of the evidence for rapid access chest pain clinics. Int J Clin Pract 20025629–33. [PubMed] [Google Scholar]
- 10.Newby D E, Fox K A A, Flint L L.et al A same day direct access chest pain clinic: improved management and reduced hospitalization.Q J M 199891333–337. [DOI] [PubMed] [Google Scholar]
- 11.Byrne J, Murdoch D, Morrison C.et al An audit of activity and outcome from a daily and a weekly “one stop” rapid assessment chest pain clinic. Postgrad Med J 20027843–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.El Gaylani N, Weston C F, Shandall A.et al Experience of a rapid access acute chest pain clinic.Irish Med J 199790139–140. [PubMed] [Google Scholar]
- 13.Davie A P, Caesar D, Caruana L.et al Outcome from a rapid‐assessment chest pain clinic. Q J Med 199891339–343. [DOI] [PubMed] [Google Scholar]
- 14.Tenkorang J N, Fox K F, Wood D A. A brief report on the data available on rapid access cardiology clinics. Br J Cardiol 200512139–141. [Google Scholar]
- 15.Wood D A, Fox K F, Gibbs S R. Rapid cardiology: for chest pain, breathlessness and palpitations.Q J M 200194177–178. [DOI] [PubMed] [Google Scholar]
- 16.Sekhri N, Timmis A D. Rapid access chest pain clinics: are they clinically effective? Hosp Med 200364324–325. [DOI] [PubMed] [Google Scholar]
- 17.Remme W J, Swedberg K. Taskforce for the diagnosis and treatment of chronic heart failure. European Society of Cardiology. Guidelines for the diagnosis and treatment of chronic heart failure. Eur Heart J 2001221527–1560. [DOI] [PubMed] [Google Scholar]
- 18.European Society of Cardiology Management of stable angina pectoris: recommendations of the task force of the European Society of Cardiology. Eur Heart J 199718394–413. [DOI] [PubMed] [Google Scholar]
- 19.Office For National Statistics Table 2.9. Deaths: underlying cause, sex and age‐group, 2003, Chapter IX. Diseases of the circulatory system. In: Mortality statistics: review of the Registrar General on deaths by cause, sex and age, in England and Wales, 2003 Series DH2, no 30. London: Office For National Statistics, 2004: 90–107. ( http://www.statistics.gov.uk/downloads/theme_health/Dh2_30/DH2No30.pdf (accessed 1 Feb 2006)
- 20.Garg R, Yusuf S. Overview of randomised trials of angiotensin‐converting enzyme inhibitors on mortality and morbidity in patients with heart failure. Collaborative group on ACE inhibitor trials. JAMA 19952731450–1456. [PubMed] [Google Scholar]
- 21.Marini C, De Santis F, Sacco S.et al Contribution of atrial fibrillation to incidence and outcome of ischemic stroke: results from a population‐based study. Stroke 2005361115–1119. [DOI] [PubMed] [Google Scholar]