Although depression symptoms are associated with an increased risk of recurrent cardiovascular disease in patients who have experienced an acute coronary syndrome (ACS) event, the exact mechanisms remain poorly understood. Inflammation has been suggested to be a mechanism in the depression–ACS prognosis link, as raised concentrations of inflammatory biomarkers, especially C reactive protein (CRP), are associated with recurrent cardiovascular events.1 In the few studies that have examined the relation between depression status and CRP concentrations after an ACS event, depression and CRP concentrations were assessed 2–6 months after the index ACS event, when the rate of depression remission would already be relatively high.2,3,4 The objective of this study was to examine the relation between the course of depression and CRP concentrations after an ACS event.
METHODS
Patients were enrolled from an ancillary study of COPES (Coronary Psychosocial Patient Evaluation Study), a multisite, observational cohort study designed to investigate the aetiology and naturalistic course of depressive symptoms in the three‐month period after an ACS event. Patients were eligible for inclusion in COPES if they had been hospitalised for an ACS event (either acute myocardial infarction with or without ST segment elevation or unstable angina) and scored between 0 and 4 (indicative of no depressive symptoms) or ⩾ 10 (at least mild depressive symptoms) on the Beck Depression Inventory (BDI) within one week after the index ACS event. The BDI is a self‐report measure of depressive symptom severity, and a score of ⩾ 10 is associated with increased mortality risk after an ACS event.5 The BDI was readministered three months after enrolment.
Of the 275 patients enrolled in the COPES parent study between May 2003 and May 2005, 162 (58.9%) consented to a substudy in which blood was drawn to assess CRP concentrations at baseline and at the three‐month follow up. Substudy participants did not differ from non‐participants on age, sex, baseline depression score and several clinical variables (p > 0.20) (table 1 lists the variables). Of the 162 participants, 59 (36.4%) did not get their blood drawn at three months: 50 patients (30.9%) were lost to follow up, 5 (3.0%) declined follow up and 4 (2.5%) died.
Table 1 Group characteristics.
| Depression category | p Value | |||
|---|---|---|---|---|
| Persistent (n = 21) | Remittent (n = 24) | Persistent non‐depression (n = 55) | ||
| Mean age (years) | 59.1 (SD 16.4) | 60.3 (SD 11.5) | 60.5 (SD 10.6) | 0.91 |
| Women | 52.4% | 75.0%* | 36.4% | 0.01 |
| Current smoker† | 23.8% | 29.2% | 12.7% | 0.19 |
| Diabetes mellitus | 14.3% | 33.3% | 21.8% | 0.30 |
| History of hypertension | 71.4% | 65.2% | 67.9% | 0.91 |
| History of hypercholesterolaemia | 65.0% | 87.0%* | 67.9% | 0.01 |
| Overweight (BMI 25–29.9 kg/m2) | 30.0% | 50.0% | 41.8% | 0.53 |
| Obese (BMI ⩾30 kg/m2) | 50.0% | 37.5% | 38.2% | 0.81 |
| History of CHF | 9.5% | 0 | 5.6% | 0.34 |
| Killip class ⩾II | 9.5% | 4.2% | 3.2% | 0.57 |
| Statin use at baseline | 40.0% | 62.5% | 41.5% | 0.19 |
| Statin use at any time during the 3 months of follow up | 81.0% | 87.5% | 90.9% | 0.49 |
*Significantly different from the persistently non‐depressed group (p<0.05); †assessed by self‐report at baseline.
BMI, body mass index; CHF, congestive heart failure.
As the primary objective of this study was to determine the relation between CRP concentration and depression remission status over time, patients were classified into three comparison groups: persistently depressed (BDI score ⩾ 10 at baseline and after three months), remittently depressed (BDI score ⩾ 10 at baseline and < 10 after three months) and persistently non‐depressed (BDI score 0–4 at baseline and < 10 after three months).
After centrifugation, serum samples were stored in aliquot portions at −70°C until they were shipped to a core laboratory (Specialty Laboratories, Valencia, California, USA) for analysis of high sensitivity CRP concentrations. Concentrations of CRP were determined by turbidimetry (Bayer Diagnostics, Leverkusen, Germany). We divided CRP concentrations into two categories: ⩽ 3 mg/l and > 3 mg/l as previously described.1 A cut off of 3 mg/l identifies a group at increased risk for recurrent events and death after an ACS event.1 Written informed consent was obtained from all participants, and the study was approved by the research ethics committees of the three university‐affiliated hospitals from which the participants were recruited (Mount Sinai Hospital, New York, New York; University of Medicine & Dentistry of New Jersey, New Jersey; and Yale–New Haven Hospital, New Haven, Connecticut, USA).
Differences in baseline characteristics between groups and differences in CRP concentrations in depression groups were analysed by univariate analyses of variance or χ2 analyses. To test for the impact of potential confounders that were specified a priori, a hierarchical logistic regression analysis was conducted. We used two‐tailed tests of significance and SPSS statistical software (V.12.0; SPSS Inc, Chicago, Illinois, USA).
RESULTS
Of 103 patients, 58 (56.3%) were depressed (BDI score ⩾ 10) and 45 (43.7%) were non‐depressed (BDI score ⩽ 4) at baseline. After three months, 21 patients (20.4%) were classified as persistently depressed, 24 (23.3%) as remittently depressed and 55 (53.4%) as persistently non‐depressed. Three patients (2.9%) became newly depressed at follow up (non‐depressed at baseline and depressed at three months). As we were primarily interested in studying the relation between depression remission status and CRP concentrations, these three patients were omitted from the analysis. Thus, the final study sample comprised 100 patients.
Among the three groups (persistently depressed, remittently depressed and persistently non‐depressed), the percentages of women and patients with a history of hypercholesterolaemia were significantly higher in the remittently depressed group than in the persistently non‐depressed group (table 1). The groups did not otherwise differ significantly in clinical characteristics.
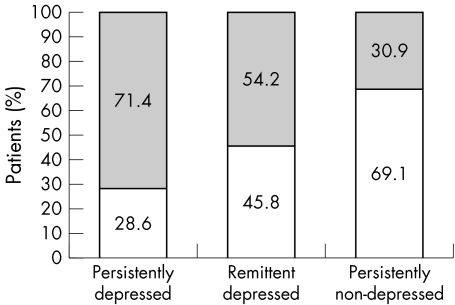
At baseline, no significant differences were found in CRP concentrations among the three groups (95.2%, 79.2%, and 72.7% respectively, p = 0.10). At three months (fig 1), persistently depressed patients were more likely to have raised CRP concentrations than were the persistently non‐depressed group (p = 0.002). Compared with the remittently depressed patients, the persistently non‐depressed group also were less likely to have raised CRP concentrations, although this difference was not significant (p = 0.08). CRP concentrations did not differ significantly between the remittently and persistently depressed patients (p = 0.36). The differences in raised CRP concentrations among the three groups remained unchanged after controlling for age, sex, body mass index, diabetes mellitus, hypertension, hypercholesterolaemia, history of congestive heart failure, Killip class and statin use at any time during the three months after the index ACS event.
Figure 1 Relation of depression remission status and raised C reactive protein (CRP) concentrations three months after an acute coronary syndrome event. The grey area indicates raised CRP concentrations (> 3 mg/l) and the white area, not raised CRP concentrations (⩽ 3 mg/l). p = 0.002 for comparison between persistently depressed and persistently non‐depressed patients; p = 0.08 for comparison between persistently non‐depressed and remittently depressed patients.
DISCUSSION
Our study is the first to assess depression and CRP concentrations within one week after an ACS event and again after three months. We found that depression remission status three months after an ACS event was significantly associated with raised CRP concentrations, independent of several possible confounders.
To our knowledge, three other studies have examined the relation between depression and inflammatory biomarker concentrations after an ACS event.2,3,4 Only one study has shown that depressive symptoms are significantly associated with increased concentrations of CRP, independent of several confounders.4 As these cross‐sectional studies assessed depression and CRP concentrations about 2–6 months after the index ACS event, discrepant results may be explained by the inclusion of patients with new‐onset depression in the depressed group and those with remittent depression in the non‐depressed group.
Spontaneous improvement in BDI scores after an ACS hospitalisation is associated with a significantly greater survival of patients with at least mild baseline depressive symptoms than of patients whose BDI scores remain raised.5 Our data suggest a dose–response‐like relation between depression remission status after an ACS event and raised CRP concentrations. Thus, the lower survival rate observed among persistently depressed patients may be associated with raised CRP concentrations and, conversely, the higher survival rate observed among patients with remittent depression may be associated with lower CRP concentrations.
Our study has potential limitations. Although these associations are plausible, our study cannot discriminate between the several possible causal directions between depression and inflammation. The study is also limited by the size of the cohort and the lack of information about antidepressant use. Further research should be conducted to confirm our findings and to examine whether raised CRP concentrations mediate the relation between depression course and the recurrence of cardiovascular events.
Abbreviations
ACS - acute coronary syndrome
BDI - Beck Depression Inventory
COPES - Coronary Psychosocial Patient Evaluation Study
CRP - C reactive protein
Footnotes
This work was supported by grants HC25197, HL072866, HL04458 and HL76857 from the National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, Maryland. The funding source supported the collection and analyses of data, but had no direct role in the interpretation of data, the writing of the report and the decision to submit the paper for publication.
Competing interests: None declared.
References
- 1.Biasucci L M. CDC/AHA workshop on markers of inflammation and cardiovascular disease: application to clinical and public health practice. Clinical use of inflammatory markers in patients with cardiovascular diseases: a background paper, Circulation 2004110e560–e567. [DOI] [PubMed] [Google Scholar]
- 2.Schins A, Tulner D, Lousberg R.et al Inflammatory markers in depressed post‐myocardial infarction patients. J Psychiatr Res 200539137–144. [DOI] [PubMed] [Google Scholar]
- 3.Lesperance F, Frasure‐Smith N, Theroux P.et al The association between major depression and levels of soluble intercellular adhesion molecule 1, interleukin‐6, and C‐reactive protein in patients with recent acute coronary syndromes. Am J Psychiatry 2004161271–277. [DOI] [PubMed] [Google Scholar]
- 4.Miller G E, Freedland K E, Duntley S.et al Relation of depressive symptoms to C‐reactive protein and pathogen burden (cytomegalovirus, herpes simplex virus, Epstein‐Barr virus) in patients with earlier acute coronary syndromes. Am J Cardiol 200595317–321. [DOI] [PubMed] [Google Scholar]
- 5.Lesperance F, Frasure‐Smith N, Talajic M.et al Five‐year risk of cardiac mortality in relation to initial severity and one‐year changes in depression symptoms after myocardial infarction. Circulation 20021051049–1053. [DOI] [PubMed] [Google Scholar]