Identification of patients with congestive heart failure (CHF) at risk for sudden cardiac death (SCD) remains a major problem. Implantable cardioverter‐defibrillator (ICD) implantation constitutes an effective preventive strategy, both for primary and for secondary prevention of SCD.1,2 Evidence regarding the benefit of ICD implantation in patients with advanced CHF is limited, however, as death caused by pump failure becomes more important in these patients and the projected life span is short. Improved risk stratification for identification of appropriate candidates for ICD implantation appears critical to ensure access of eligible patients to this lifesaving treatment and to spare inappropriate candidates the side effects. Cost effectiveness is critically dependent on identification of appropriate high‐risk subgroups in patient groups with low left ventricular ejection fraction (LVEF).1 The role of the B‐type natriuretic peptides in predicting mortality in patients with CHF including SCD is increasingly being recognised.3,4 The definition of SCD used in clinical trials does not rule out ischaemic or non‐cardiac causes of death, however, as shown by an autopsy study.5 The present study evaluated the hypothesis that raised N‐terminal pro‐brain natriuretic peptide (NT‐proBNP) concentrations may predict ventricular tachyarrhythmia as a surrogate marker of SCD in patients with ischaemic CHF and an ICD device.
METHODS
NT‐proBNP concentrations (Roche Diagnostics, Mannheim, Germany) were determined at ICD implantation in patients with ischaemic CHF (scintigraphic LVEF ⩽ 30%) and were correlated with the results of ICD interrogation during the first postoperative year. Exclusion criteria were NT‐proBNP measurement unavailable at the time of ICD implantation, acute cardiogenic shock, myocardial infarction, renal failure, operation within four weeks before ICD implantation, a combined ICD/cardiac resynchronisation therapy device, patients lost to follow up, and technical ICD defects after implantation. Appropriate ICD therapy comprised defibrillation (active ventricular tachycardia (VT) zones) and antitachycardia pacing to avoid missing critical episodes of ventricular tachyarrhythmia, as no homogeneous predefined ventricular fibrillation zones were available. Inappropriate therapy was for tachyarrhythmic episodes of supraventricular origin or slow VT evaluated by an electrophysiologist in our centre blinded to the study. Kaplan–Meier log rank analyses were performed for a range of potential cut‐off NT‐proBNP concentrations to determine the distribution of tachyarrhythmia‐free survival time. The best discriminating NT‐proBNP concentration was thus derived. Univariate and multivariate Cox regression analyses were performed to determine an association with ICD therapy.
RESULTS
Fifty patients with advanced ischaemic CHF (median New York Heart Association (NYHA) class 3, median LVEF 20%, median NT‐proBNP concentration 1690 pg/ml) were identified who had received an ICD for primary (n = 34, MUSTT (Multicenter Unsustained Tachycardia Trial) criteria) or secondary prevention (n = 16, AVID (Antiarrhythmics Versus Implantable Defibrillators) criteria).1,2 The follow‐up period was restricted to one year (median 0.78 years with a median of four postoperative visits), as NT‐proBNP concentrations are subject to change. Among 193 ICD interrogations, 34 (17.6%) showed appropriate ICD therapy (9 × shock for fast VT, 16 × shock for ventricular fibrillation and 9 × antitachycardia pacing for fast VT). The average annual rate of appropriate ICD therapies per interrogations was 22.6%. In the group of patients with ICD events (n = 16, 11 of whom had 2–4 events) NT‐proBNP concentrations were significantly higher than in the remaining patients (5836 (4140) v 1654 (1431) pg/ml, p = 0.0023).
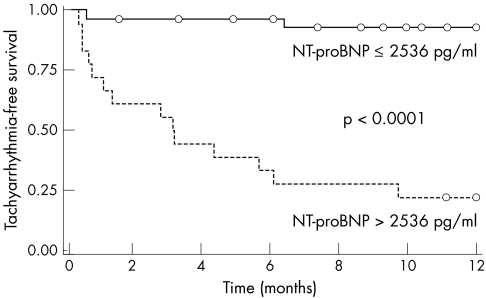
NT‐proBNP concentration of 2536 pg/ml was identified as the optimal cut off for the prediction of ICD therapy during the first postoperative year, characterised by a sensitivity of 87.5% and a specificity of 88%. Patients stratified accordingly did not differ significantly in clinical and demographic parameters (table 1). ICD therapy was detected in significantly more patients with NT‐proBNP concentrations above the cut‐off concentration (14/18 v 2/32, p = 0.0005) and tachyarrhythmia‐free survival was significantly worse (p < 0.0001) (fig 1). Univariate analysis identified raised NT‐proBNP (p < 0.0001, relative risk (RR) 7.73, 95% confidence interval (CI) 2.92 to 20.45), no treatment with statins (p = 0.0103, RR 3.18, 95% CI 1.31 to 7.69), atrial fibrillation (p = 0.0256, RR 2.87, 95% CI 1.14 to 7.25) and indication for ICD implantation (secondary prevention) (p = 0.0341, RR 2.55, 95% CI 1.07 to 6.06) as significant predictors of ICD therapy. Drug, LVEF, sex, heart rate variability (standard deviation of all normal‐to‐normal RR intervals), NYHA functional class, QRS duration, serum creatinine concentration, age, blood pressure, heart rate and non‐sustained VT had no influence. Multivariate analysis identified NT‐proBNP as the only independent predictor of future ICD events (p < 0.0001, RR 11.07, 95% CI 3.57 to 34.30).
Table 1 Patient characteristics.
| Parameter | NT‐proBNP (pg/ml) | |
|---|---|---|
| ⩽2536 (n = 32) | >2536 (n = 18) | |
| Age (years) | 57.7 (7.6) | 60.3 (8.7) |
| Men | 26/32 (81.3%) | 16/18 (88.9%) |
| NYHA class | 2.6 (0.5) | 2.7 (0.7) |
| LVEF by scintigraphy (%) | 21.1 (4.3) | 19.1 (7.4) |
| Serum creatinine (μmol/l) | 97.2 (26) | 97.2 (18) |
| Sinus rhythm | 27/32 (84.4%) | 14/18 (77.8%) |
| QRS duration (ms) | 137.4 (34.0) | 135.6 (27.8) |
| Heart rate variability (SDNN) (ms) | 146.7 (37.9) | 142.1 (31.4) |
| NSVT | 24/32 (75%) | 14/18 (77.8%) |
| Heart rate (beats/min) | 67.3 (13.5) | 70.2 (15.1) |
| Systolic blood pressure (mm Hg) | 112.7 (15.5) | 114.4 (22.1) |
| Diastolic blood pressure (mm Hg) | 72.5 (11.7) | 73.2 (11.3) |
| ACE/ATIIR inhibitor | 30/32 (93.8%) | 14/18 (77.8%) |
| β blocker | 28/32 (87.5%) | 12/18 (66.7%) |
| Statins | 25/32 (78.1%) | 11/18 (61.1%) |
| Spironolactone | 22/32 (68.8%) | 10/18 (55.6%) |
| Digitalis | 18/32 (56.3%) | 13/18 (72.2%) |
| Diuretics | 26/32 (81.3%) | 15/18 (83.3%) |
| Follow up (years) | 0.72 (0.23) | 0.69 (0.23) |
| ICD for secondary prevention | 8/32 (25%) | 8/18 (44.4%) |
| Death or heart transplant | 1/32 (3.1%) | 4/18 (22.2%) |
Continuous and categorical variables were compared by Student's t test and the χ2 test, respectively. All differences were non‐significant.
ACE, angiotensin‐converting enzyme; ATIIR, angiotensin II type 1 receptor; ICD, implantable cardioverter‐defibrillator; NSVT, non‐sustained ventricular tachycardia; NT‐proBNP, N‐terminal pro‐brain natriuretic peptide; NYHA, New York Heart Association; SDNN, standard deviation of all normal‐to‐normal RR intervals.
Figure 1 Event‐free survival (Kaplan–Meier analysis) is shown for the two patient groups stratified according to N‐terminal pro‐brain natriuretic peptide (NT‐proBNP) cut‐off concentration of 2536 pg/ml. Detection of appropriate implantable cardioverter‐defibrillator (ICD) therapy was a censored event; otherwise, follow up extended until completion of the first postoperative year. Open circles represent patients without an ICD event.
Tachyarrhythmia‐free survival remained significantly worse in a subgroup analysis with this NT‐proBNP cut‐off concentration (p = 0.0001 in the primary prevention group, n = 34, and p = 0.0005 in the secondary prevention group, n = 16). In both subgroups NT‐proBNP was the only independent predictor of ICD therapy (p = 0.0058, RR 7.74, 95% CI 1.81 to 33.17, and p = 0.024, RR 13.06, 95% CI 1.40 to 121.59, respectively).
DISCUSSION
Our study identified raised NT‐proBNP concentrations in a high‐risk group of patients with advanced ischaemic CHF as the only independent predictor of appropriate ICD therapy. This finding underscores the data from a previous study in which log BNP was identified as a significant predictor of SCD.4 Our study used a different assay system (NT‐proBNP instead of BNP) and has two major advantages. Firstly, we used appropriate ICD therapy instead of the vague clinical definition of SCD, which cannot exclude non‐arrhythmogenic death.5 Secondly, the NT‐proBNP cut‐off concentration identified in our study is about 10‐fold higher than a reasonable threshold (250 pg/ml) for the diagnosis of CHF in patients with normal renal function, enabling meaningful risk stratification of patients, unlike the very low BNP cut‐off concentration in the previous study (130 pg/ml), comprising the great majority of patients with CHF.4 Furthermore, our NT‐proBNP cut‐off concentration appears safe, as only two of 50 patients (4%) who fell below the cut off had ICD therapy.
Our data suggest that the use of NT‐proBNP may improve candidate selection for ICD implantation. We regard the results from our pilot study as hypothesis generating and not as the basis for clinical decision making. We believe, however, that our study may provide the rationale to conduct a prospective clinical multicentre trial to validate our findings in a larger patient group combining serial measurements of NT‐proBNP with a longer follow up.
ACKNOWLEDGEMENTS
We thank the nursing staff in the heart failure and defibrillator clinics for thorough patient data documentation.
Abbreviations
AVID - Antiarrhythmics Versus Implantable Defibrillators
CHF - congestive heart failure
ICD - implantable cardioverter defibrillator
LVEF - left ventricular ejection fraction
MUSTT - Multicenter Unsustained Tachycardia Trial
NT‐proBNP - N‐terminal pro‐brain natriuretic peptide
NYHA - New York Heart Association
RR - relative risk
SCD - sudden cardiac death
VT - ventricular tachycardia
Footnotes
Funding: This work has not been funded by specific grants or financial support from other sources and there is no conflict of interest with any of the authors.
Competing interests: The contributing authors have not been influenced in any way by a conflict of interest by sponsoring or the like from a pharmaceutical company or any other external influence in the design, data collection, processing of data and writing of this manuscript.
Ethical approval: Patient data and all patient‐related information were gathered and processed after patient consent was obtained. All data were processed with utmost care to preserve privacy and all steps were in accordance with the requirements of the local ethics committee in Heidelberg.
References
- 1.Sanders G D, Hlatky M A, Owens D K. Cost‐effectiveness of implantable cardioverter‐defibrillators. N Engl J Med 20053531471–1480. [DOI] [PubMed] [Google Scholar]
- 2.The Antiarrhythmics Versus Implantable Defibrillators (AVID) Investigators A comparison of antiarrhythmic‐drug therapy with implantable defibrillators in patients resuscitated from near‐fatal ventricular arrhythmias. N Engl J Med 19973371576–1583. [DOI] [PubMed] [Google Scholar]
- 3.Maeda K, Tsutamoto T, Wada A.et al High levels of plasma brain natriuretic peptide and interleukin‐6 after optimized treatment for heart failure are independent risk factors for morbidity and mortality in patients with congestive heart failure. J Am Coll Cardiol 2000361587–1593. [DOI] [PubMed] [Google Scholar]
- 4.Berger R, Huelsman M, Strecker K.et al B‐type natriuretic peptide predicts sudden death in patients with chronic heart failure. Circulation 20021052392–2397. [DOI] [PubMed] [Google Scholar]
- 5.Uretsky B F, Thygesen K, Armstrong P W.et al Acute coronary findings at autopsy in heart failure patients with sudden death: results from the assessment of treatment with lisinopril and survival (ATLAS) trial. Circulation 2000102611–616. [DOI] [PubMed] [Google Scholar]