Abstract
Objective
To determine the prevalence and predictors of left ventricular (LV) diastolic dysfunction in older adults.
Design, setting and participants
A cross‐sectional survey of 1275 randomly selected residents of Canberra, aged 60 to 86 years (mean age 69.4; 50% men), conducted between February 2002 and June 2003.
Main outcome measures
Prevalence of LV diastolic dysfunction as characterised by comprehensive Doppler echocardiography.
Results
The prevalence of any diastolic dysfunction was 34.7% (95% CI 32.1% to 37.4%) and that of moderate to severe diastolic dysfunction was 7.3% (95% CI 5.9% to 8.9%). Of subjects with moderate to severe diastolic dysfunction, 77.4% had an LV ejection fraction (EF) > 50% and 76.3% were in a preclinical stage of disease. Predictors of diastolic dysfunction were higher age (p < 0.0001), reduced EF (p < 0.0001), obesity (p < 0.0001) and a history of hypertension (p < 0.0001), diabetes (p = 0.02) and myocardial infarction (p = 0.003). Moderate to severe diastolic dysfunction with normal EF, although predominantly preclinical, was independently associated with increased LV mass (p < 0.0001), left atrial volume (p < 0.0001), and circulating amino‐terminal pro‐B‐type natriuretic peptide concentrations (p < 0.0001), and with decreased quality of life (p < 0.005).
Conclusion
Diastolic dysfunction is common in the community and often unaccompanied by overt congestive heart failure. Despite the lack of symptoms, advanced diastolic dysfunction with normal EF is associated with reduced quality of life and structural abnormalities that reflect increased cardiovascular risk.
Over the past decade, several important observations on the pathophysiological mechanisms underlying heart failure in the community have been documented through population‐based echocardiographic surveys.1,2,3,4,5,6,7,8 Firstly, congestive heart failure (CHF) has been reported in the presence of a normal left ventricular (LV) ejection fraction (EF).7,8 Although controversial, the presumed pathophysiology for most patients with heart failure and a normal EF is LV diastolic dysfunction.9,10 Secondly, subjects with heart failure and a normal LV EF have been shown to have a poor prognosis, even though mortality and morbidity in this group are not as high as in patients with a reduced EF.7,11
Following these observations, interest in the epidemiology of diastolic dysfunction has been growing, which has been facilitated by the availability of non‐invasive Doppler methods of characterising diastolic function.12 A recent study5 showed that subjects with normal EF can have moderate or severe diastolic dysfunction, most often without accompanying clinical evidence of heart failure. The validity of findings from these cross‐sectional surveys of diastolic dysfunction has, however, been compromised by low participation rates5 and the failure to use comprehensive Doppler methods13 to distinguish subjects with normal and pseudonormal mitral inflow patterns, which have increased the potential for selection bias and misclassification of diastolic function. In addition, there is a paucity of data regarding echocardiographic and clinical characteristics of subjects with diastolic dysfunction and normal EF (DD‐NEF) and their influence on clinical status. Our objectives in this study were to determine the prevalence of diastolic dysfunction in older adults and to describe the clinical spectrum of subjects with DD‐NEF.
METHODS
As part of the Canberra Heart Survey, the Australian Capital Territory Health and Community Care Committee and Australian National University Human Research Ethics Committee approved this study in January 2002.
Study population
Simple random sampling from a population register (federal electoral roll, January 2002) was used to select 2000 Canberra residents, aged 60–85 years, to constitute our study population. The sample size was selected on the basis of the precision of estimates to determine a prevalence of advanced “isolated” LV diastolic dysfunction of 4% and the assumption of a 60% participation rate. Subjects were invited to participate by letter. Institutionalised subjects and those who had died or had moved away from the Territory were excluded from the study sample. All study participants provided written and informed consent for the study investigations and were enrolled between February 2002 and June 2003.
Assessment of clinical risk factors for heart failure
A self‐administered questionnaire was used to gather data on a history of myocardial infarction, angina, hypertension or diabetes. Brachial artery systolic and diastolic blood pressures were measured after 10 min of rest in a seated position; two sets were averaged for each participant. Height and weight were measured while the subject was wearing light clothing but not shoes. Body mass index was calculated for each participant (weight in kilograms divided by the square of height measured in metres) and categorised according to the World Health Organization classification scheme (not overweight or obese < 25 kg/m2, overweight 25.0–29.9 kg/m2, obese ⩾ 30 kg/m2).
Echocardiography
One of two experienced sonographers assessed cardiac structure and function by using transthoracic echocardiography (Acuson 128 XP/10, equipped with native tissue harmonic imaging technology) according to a standardised protocol. Measurements were made online and recorded on tape with participants' initials and study number as their only identification. A cardiologist, blinded to the participant's clinical data, interpreted the echocardiogram after review off line. LV EF was quantified by the biplane disc summation method (Simpson's rule) on the two‐dimensional echocardiographic images from the apical four‐ and two‐chamber views.14 LV systolic function was categorised according to EF (⩽ 40%, 41–50%, > 50%) and the presence of regional LV wall motion abnormalities. LV diastolic function was graded into four categories by Doppler evaluation of the mitral and pulmonary venous inflow and by tissue Doppler imaging of the lateral mitral annulus motion (table 1).13 In a stratified subsample of 50 participants, interobserver reproducibility for grading of systolic and diastolic function was very good (κsystolic = 0.88, 95% confidence interval (CI) 0.63 to 1.0 and κdiastolic = 0.89, 95% CI 0.64 to 1.0). Valvular heart disease was defined as at least moderate stenosis or regurgitation of the aortic or mitral valve on colour Doppler and quantitative Doppler echocardiographic evaluation. LV mass was assessed by the area–length method, by using the two‐dimensional short‐axis parasternal view at the papillary muscle level to measure LV muscle area and the apical four‐chamber view to measure the LV length.15 The LV mass was indexed for each participant's body surface area. Maximum left atrial volume was quantified by the modified prolate ellipse method16 and indexed for body surface area.
Table 1 Doppler assessment of left ventricular diastolic function (LVDD).
| Mitral inflow | Pulmonary venous inflow | TDI MAM | |
|---|---|---|---|
| Normal | 0.75 < E:A <1.5 | S>D | E/e′ <10 |
| DT >160 ms | MV Adur > PV Adur | ||
| Mild LVDD | E:A <0.75 | S>D | E/e′ <10 |
| DT >240 ms | MV Adur > PV Adur | ||
| Moderate LVDD | 0.75 < E:A <1.5 | S<D | E/e′ ⩾10 |
| DT >160 ms | MV Adur + 30 ms < PV Adur | ||
| Severe LVDD | E:A >1.5 | S<D | E/e′ ⩾10 |
| DT <160 ms | MV Adur + 30 ms < PV Adur |
At least two Doppler criteria consistent with moderate to severe left ventricular diastolic function were required to distinguish from normal diastolic function.
A, peak mitral filling velocity at atrial contraction; D, peak velocity of pulmonary venous forward flow during diastole; DT, deceleration time of mitral E wave; E, peak early mitral inflow filling velocity; e′, peak velocity of lateral mitral annulus motion during early diastole; MV Adur, duration of mitral A wave; PV Adur, duration of pulmonary venous reversal wave at atrial contraction; S, peak velocity of pulmonary venous forward flow during systole; TDI MAM, tissue Doppler imaging of mitral annular motion.
Ascertainment of CHF status
A self‐reported history of clinical heart failure was verified by a review of the subject's medical records. During a consultation with a cardiologist who was blinded to the echocardiographic findings and medical history, participants were asked if they had symptoms of dyspnoea, orthopnoea, paroxysmal nocturnal dyspnoea or dependant oedema. They were also examined for the presence of a tachycardia, raised jugular venous pressure, displaced apex beat, added heart sounds, cardiac murmurs, lung crepitations and peripheral oedema. Heart failure clinical status was ascertained according to clinical scores based on the New York Heart Association classification of functional status17 and Framingham criteria for the clinical diagnosis of CHF.18 Subjects with systolic or diastolic dysfunction without a history or clinical evidence of heart failure were considered to be in the preclinical phase of disease. Serum amino‐terminal B‐type natriuretic peptide (N‐BNP) concentrations were measured with a fully automated electrochemiluminescence sandwich immunoassay (proBNP, Roche Diagnostics).
Quality of life
The standardised SF‐36 questionnaire was administered to assess general health status.
Statistical analysis
Continuous variables are presented as mean (SD). Categorical variables are displayed as percentages. Differences between groups were assessed by likelihood ratio tests (categorical variables) or Kruskal–Wallis tests and non‐parametric tests for trend (continuous variables), as appropriate. We calculated the point estimate and 95% CI (by the exact binomial method) for diastolic dysfunction (for any EF and for subjects with EF > 50%), stratified for five‐year age groups and sex. Ordinal logistic regression was used to assess the association between the ordinal variable, diastolic function grade and clinical or echocardiographic predictors in univariable and multivariable analyses, adjusted for age and sex and relevant covariates. Least squares linear regression was used to assess the relationship between general health status score and diastolic function grade, after adjustment for age, sex and significant covariates. All hypothesis testing was two sided, and significance was declared if p < 0.05. The assumptions for regression models were checked statistically.
RESULTS
Study participants
Seventy‐five per cent (1388 of 1846) of the eligible subjects agreed to participate in the survey. The only groups with participation rates < 70% were women aged 75–79 years (68%) and > 80 years (49%). Consequently, compared with the source population, the sample population had a higher proportion of men (50.5% v 47.2%, p < 0.012) and were younger (68.9 years v 69.6 years, p = 0.0005). About 92% participants (1275 of 1388; mean age 69.4; 50% men) completed all the echocardiographic investigations necessary for assessment of LV function.
Diastolic dysfunction in the community
For 32 subjects, diastolic function grade could not be determined (atrial fibrillation with deceleration time of mitral E wave > 140 ms; mitral stenosis; E:A fusion; and only a single criterion suggestive of moderate to severe diastolic dysfunction). The prevalence of any diastolic dysfunction was 34.7% (95% CI 32.1% to 37.4%) and that of moderate to severe diastolic dysfunction was 7.3% (95% CI 5.9% to 8.9%). Table 2 presents the prevalence of diastolic dysfunction stratified by age group, sex and EF status.
Table 2 Prevalence of diastolic dysfunction in the cohort (n = 1275) stratified by age group, sex and left ventricular ejection fraction status.
| Age groups (years) | ||||||
|---|---|---|---|---|---|---|
| 60–64 | 65–69 | 70–74 | 75–79 | 80–86 | All | |
| Diastolic dysfunction, any ejection fraction | ||||||
| Mild | ||||||
| Men | 30 (15.3%) | 39 (23.8%) | 36 (31.0%) | 29 (32.2%) | 36 (51.4%) | 170 (26.7%) |
| Women | 31 (16.1%) | 37 (24.8%) | 45 (30.8%) | 43 (41.7%) | 23 (47.9%) | 179 (28.0%) |
| All | 61 (15.7%) | 76 (24.3%) | 81 (30.9%) | 72 (37.3%) | 59 (50.0%) | 349 (27.4%) |
| Moderate or severe | ||||||
| Men | 10 (5.1%) | 13 (7.9%) | 8 (6.9%) | 8 (8.9%) | 8 (11.4%) | 47 (7.4%) |
| Women | 4 (2.1%) | 6 (4.0%) | 13 (8.9%) | 14 (13.6%) | 9 (18.8%) | 46 (7.2%) |
| All | 14 (3.6%) | 19 (6.1%) | 21 (8.0%) | 22 (11.4%) | 17 (14.4%) | 93 (7.3%) |
| Diastolic dysfunction with normal ejection fraction | ||||||
| Mild | ||||||
| Men | 28 (14.3%) | 33 (20.1%) | 29 (25.0%) | 21 (23.3%) | 23 (32.9%) | 134 (21.1%) |
| Women | 31 (16.1%) | 35 (23.5%) | 43 (29.5%) | 37 (35.9%) | 19 (39.6%) | 165 (25.8%) |
| All | 59 (15.2%) | 68 (21.7%) | 72 (27.5%) | 58 (30.1%) | 42 (35.6%) | 299 (23.5%) |
| Moderate or severe | ||||||
| Men | 6 (3.1%) | 9 (5.5%) | 6 (5.2%) | 4 (4.4%) | 7 (10.0%) | 32 (5.0%) |
| Women | 2 (1.0%) | 6 (4.0%) | 12 (8.2%) | 14 (13.6%) | 6 (12.5%) | 40 (6.3%) |
| All | 8 (2.1%) | 15 (4.8%) | 18 (6.9%) | 18 (9.3%) | 13 (11.0%) | 72 (5.6%) |
Table 3 outlines the univariate associations between clinical characteristics and diastolic function. Higher age was associated with any diastolic dysfunction (p < 0.0001) and moderate to severe diastolic dysfunction (3.6% in subjects aged 60–64 years v 14.4% in subjects aged > 80 years, ptrend < 0.001), but rates of any diastolic dysfunction (p = 0.68) or moderate to severe diastolic dysfunction did not differ significantly between men and women (7.4% v 7.2%, respectively, p = 0.90). After adjustment for age and sex, a history of hypertension (p = 0.002), diabetes (p = 0.03), angina (p = 0.048), myocardial infarction (p < 0.0001), overweight (p = 0.01) and obesity (p < 0.0001) were associated with diastolic dysfunction (table 4).
Table 3 Clinical characteristics of participants according to left ventricular diastolic function status*.
| Diastolic dysfunction, any ejection fraction | p Value | |||
|---|---|---|---|---|
| Normal (n = 801) | Mild (n = 349) | Moderate to severe (n = 93) | ||
| Age (years) | 68 (6) | 72 (7) | 73 (7) | <0.0001 |
| Women | 403 (50.3%) | 179 (51.3%) | 46 (49.5%) | 0.94 |
| Systolic blood pressure (mm Hg) | 137 (17) | 140 (17) | 139 (18) | 0.001 |
| Hypertension | 337 (42.0%) | 191 (54.7%) | 59 (63.4%) | <0.0001 |
| Angina | 75 (9.4%) | 53 (15.2%) | 22 (23.7%) | <0.0001 |
| Myocardial infarction | 37 (4.6%) | 33 (9.5%) | 21 (22.6%) | <0.0001 |
| Diabetes | 73 (9.1%) | 37 (10.6%) | 18 (19.4%) | 0.007 |
| Obesity | 223 (27.8%) | 98 (28.1%) | 39 (41.9%) | 0.01 |
| Excessive alcohol intake | 30 (3.7%) | 18 (5.2%) | 6 (6.5%) | 0.32 |
Data are mean (SD) or number (%).
*Excluding 32 participants with indeterminate left ventricular diastolic function.
Table 4 Association between clinical and echocardiographic parameters and left ventricular diastolic dysfunction.
| Adjusted OR (95% CI)* | p Value | |
|---|---|---|
| Men | 0.97 (0.76 to 1.23)† | 0.78 |
| Age group (referent: 60–69 years) | ||
| 70–79 years | 2.5 (1.9 to 3.2)‡ | <0.0001 |
| 80–86 years | 5.7 (3.9 to 8.4)‡ | <0.0001 |
| Hypertension | 1.5 (1.2 to 2.0) | 0.002 |
| Diabetes | 1.4 (1.03 to 2.0) | 0.029 |
| Myocardial infarction | 2.8 (1.8 to 4.4) | <0.0001 |
| Coronary disease | 1.8 (1.3 to 2.4) | <0.0001 |
| Body mass index (referent: <25 kg/m2) | ||
| 25–29.9 kg/m2 | 1.5 (1.1 to 2.0) | 0.01 |
| ⩾30 kg/m2 | 1.9 (1.3 to 2.6) | <0.0001 |
| Ejection fraction ⩽50% | 5.4 (3.3 to 8.8) | <0.0001 |
*Adjusted for age and sex unless specified; †adjusted for age; ‡adjusted for sex.
CI, confidence interval; OR, odds ratio.
Rates of diastolic dysfunction increased with decreasing EF (p = 0.0001). Indeed, there were no subjects with an EF ⩽ 40% with normal LV diastolic function.
Diastolic dysfunction with normal EF
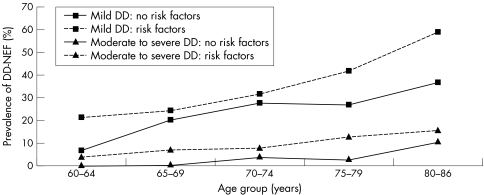
The prevalence of moderate to severe diastolic dysfunction with an EF > 50% and no regional LV wall motion abnormalities was 5.6% (95% CI 4.4% to 7.1%). Rates of DD‐NEF increased with age (p < 0.0001) but did not differ between men and women (p = 0.34). Clinical predictors of DD‐NEF were a history of hypertension (p < 0.0001), angina (p = 0.04), myocardial infarction (p = 0.003), and obesity (p < 0.0001). Figure 1 presents the impact of cardiovascular risk factors on age‐specific rates of DD‐NEF. Of subjects aged < 70 years and without a history of hypertension, ischaemic heart disease, diabetes or obesity, advanced DD‐NEF was documented in only one person.
Figure 1 Influence of age and risk factor status on the prevalence of mild and moderate to severe diastolic dysfunction (DD) in subjects with left ventricular ejection fraction >50% and no regional wall motion abnormalities. Risk factor status was dichotomised according to history of the risk factors; hypertension, ischaemic heart disease (angina or myocardial infarction), obesity, and diabetes. NEF, normal ejection fraction.
Doppler evidence of moderate or severe DD‐NEF was accompanied by echocardiographic and biochemical markers of impaired LV relaxation and increased LV filling pressure. Even after we controlled for age, sex and EF, worsening DD‐NEF was associated with an increase in indexed left atrial volume (p < 0.0001) and N‐BNP concentration (p < 0.0001). Indexed left atrial volume (p = 0.61) and N‐BNP concentration (p = 0.10), however, did not differ significantly between subjects with normal and those with mild diastolic dysfunction, even after stratification for age and sex.
In subjects with DD‐NEF, there was evidence of LV remodelling and alterations in long‐axis systolic function (table 5). LV mass index increased and mitral annular systolic velocity decreased with advancing diastolic dysfunction (p < 0.0001 for both), independent of age and sex. However, EF did not decrease significantly in subjects with DD‐NEF (ptrend = 0.11).
Table 5 Echocardiographic characteristics of participants with normal EF by diastolic function status.
| Normal* (n = 755) | Diastolic dysfunction, normal EF† | p Value | ||
|---|---|---|---|---|
| Mild (n = 299) | Moderate to severe (n = 72) | |||
| Age (years) | 68 (6) | 71 (7) | 73 (6) | <0.0001 |
| Women | 394 (52.2%) | 165 (55.2%) | 38 (54.3%) | 0.34 |
| General health status score (/100) | 69 (22) | 63 (24) | 54 (26) | <0.0001 |
| LV EF (%) | 68 (5) | 67 (5) | 66 (7) | 0.11 |
| Mitral annular systolic velocity (cm/s) | 10.6 (3) | 10.8 (3) | 8.4 (2) | <0.0001 |
| LVEDD index (cm/m2) | 2.67 (0.3) | 2.68 (0.4) | 2.70 (0.3) | 0.31 |
| LV mass index (g/m) | 100 (24) | 106 (31) | 121 (33) | <0.0001 |
| Left atrial volume index (ml/m2) | 22.4 (6.6) | 23.4 (8.3) | 37.5 (14) | <0.0001 |
| Mitral annular diastolic velocity (cm/s) | 10.1 (2) | 8.6 (2) | 8.5 (2.8) | <0.0001 |
| Amino‐terminal pro‐BNP (pmol/l) | 14 (13) | 19 (31) | 105 (164) | <0.0001 |
*Ejection fraction (EF) >50%, no regional wall motion abnormalities and normal diastolic function; †EF >50% and no regional wall motion abnormalities.
BNP, B‐type natriuretic peptide; LV, left ventricular; LVEDD, left ventricular end diastolic diameter.
Quality of life, as assessed by general health status (table 5), progressively deteriorated with increasing severity of DD‐NEF, independent of age, sex, overweight or obesity status, history of hypertension, diabetes or ischaemic heart disease, or EF (p < 0.0001).
Relationship between DD‐NEF and heart failure status
Of subjects with a previous diagnosis of heart failure, 47% (95% CI 35% to 59%) had an EF > 50% and no evidence of regional wall motion abnormalities. Of subjects with moderate to severe DD‐NEF, 86% were in the preclinical stage of disease as assessed by strict Framingham criteria. Even when clinical status was judged by the New York Heart Association classification, 36% of subjects with moderate to severe DD‐NEF were asymptomatic. Thus, about one in 20 subjects in the sample population had preclinical advanced DD‐NEF (4.9%, 95% CI 3.7% to 6.2%). In contrast, preclinical advanced systolic dysfunction (EF ⩽ 40%) was rare (0.5%, 95% CI 0.2% to 1.0%).
Markers of progression from preclinical DD‐NEF to overt CHF were decreased EF (66% in preclinical advanced DD‐NEF v 59% in clinical advanced DD‐NEF, p = 0.003), increased N‐BNP concentration (84 pmol/l v 248 pmol/l, p = 0.03) and trends towards increased LV end diastolic size (2.67 cm/m2v 2.83 cm/m2, p = 0.13) and indexed left atrial volume (36.3 ml/m2v 45.1 ml/m2, p = 0.11).
DISCUSSION
In this population‐based sample of older adults, diastolic dysfunction was common and increased in frequency with age. In contrast to the female preponderance documented in studies of heart failure with normal EF,7 we found that diastolic dysfunction was equally common in men and women. Co‐morbid cardiovascular conditions such as hypertension, ischaemic heart disease, diabetes, obesity and systolic dysfunction were predictors of diastolic dysfunction, independent of age and sex. Advanced (moderate or severe) diastolic dysfunction rarely equated to “diastolic” heart failure. Indeed, 76% of patients with advanced diastolic dysfunction did not have overt symptoms or a history of CHF. We observed that advanced DD‐NEF was as common as systolic dysfunction (EF ⩽ 50%) and more likely to be present in the preclinical phase of disease. Despite the frequent absence of symptoms, subjects with advanced DD‐NEF had evidence of structural remodelling, including increased left atrial size and LV mass, and raised N‐BNP concentrations compared with subjects with normal or mildly impaired diastolic function. Furthermore, DD‐NEF was independently associated with a reduction in general health status.
Several factors enhance the validity of results from this study compared with previously published surveys. Our estimates of systolic and diastolic dysfunction are less likely to be affected by selection bias arising from a low participation rate5 or misclassification error resulting from the failure to use comprehensive Doppler methods to distinguish subjects with normal diastolic function from those with moderate diastolic dysfunction.6 Nonetheless, the consistency in prevalence and clinical predictors of diastolic dysfunction between our study and the only other study that employed detailed Doppler methods of estimating LV filling pressure5 provides reassurance as to the generalisability of our findings.
This study extends previously published observations on the relationship between DD‐NEF and CHF status.5 In addition to surveillance of medical records, the incorporation of a clinical examination to detect symptoms and signs of CHF has provided a more robust classification of clinical status of subjects with DD‐NEF. By using an array of clinical scores that offer varying degrees of sensitivity and specificity, we have confirmed the existence of a preclinical phase of advanced diastolic dysfunction that is detectable by comprehensive Doppler echocardiography. Indeed, the prevalence of preclinical advanced DD‐NEF is 10‐fold greater than that of advanced systolic dysfunction. There is scant evidence regarding the prognostic significance of preclinical diastolic dysfunction. Despite their lack of symptoms, subjects with preclinical advanced DD‐NEF have biochemical and morphological evidence supporting the presence of current and chronic rise of LV filling pressures as assessed by N‐BNP concentration and left atrial size, respectively. Further, as left atrial size has been shown to be an independent risk marker for the development of atrial fibrillation,19,20 stroke,21 incident CHF22 and cardiovascular death,23 preclinical DD‐NEF is likely to be a condition that portends a poor cardiovascular prognosis. Our conclusion is supported by longitudinal data from a study of Olmsted County residents, which has shown that people with advanced diastolic dysfunction, most of whom were in a preclinical stage of disease, had a 10‐fold higher risk of all cause death than subjects with normal diastolic function after adjustment for age, sex and EF.5
Despite evidence from convenience samples that patients with heart failure24,25,26 or DD‐NEF have a subtle decrease in LV long‐axis systolic dysfunction,26,27 subjects with diastolic dysfunction with an EF > 50% have recently been classified as having isolated diastolic dysfunction.5 Our results suggest that this term may be an oversimplification. We have observed that, in subjects with an EF > 50% and no regional wall motion abnormalities, advancing diastolic dysfunction was associated with a decrease in long‐axis systolic function and CHF status was related to a reduction in radial systolic function, although EF remained within “normal” limits. Furthermore, there was a trend towards an increase in LV end diastolic size with advancing diastolic dysfunction and in subjects with symptomatic DD‐NEF. Thus, at least some subjects with advanced DD‐NEF may have cardiac remodelling as a pathophysiological response to co‐morbid cardiovascular conditions (hypertension, ischaemic heart disease or obesity), with increased LV filling pressure related to an increased ventricular capacitance rather than a shift in the end diastolic pressure–volume relationship caused by a pure decrease in LV compliance. Although recent studies have provided an insight into the mechanisms underlying such a response by showing that patients with advanced DD‐NEF have load‐dependent alterations in diastolic function caused by increased LV systolic and arterial stiffness,28 more work is required to confirm these findings.
Study limitations
A low participation rate from women aged > 80 may have resulted in an underestimation of the true prevalence of LV dysfunction in the source population. Although echocardiography is widely accepted as a safe and convenient method for the diagnosis and follow up of patients with diastolic dysfunction,12 it is recognised that Doppler echocardiographic methods reflect integrative properties of diastolic function that lack specificity.29 In this study of survey participants, we could not justify the use of invasive methods for the assessment of active and passive diastolic LV properties. Most (97.6%) of our sample was white and our results may not be applicable to non‐white populations. As our data are cross sectional, we were unable to determine temporal relationships (and thus causal relationships) between clinical parameters, cardiac remodelling and diastolic function.
Implications
The burden of DD‐NEF in the community will probably increase with the ageing population and escalating rates of obesity and diabetes in the community. Whether this burden can be reduced by screening efforts remains to be determined. Our observations suggest that, as preclinical advanced DD‐NEF is relatively common and associated with cardiac markers that portend a poor cardiovascular prognosis, screening efforts may be warranted. Before community‐based screening programmes for LV (systolic and diastolic) dysfunction are adopted, however, more data are required detailing the natural history of the disease, the efficacy of treatment for preclinical LV dysfunction, the screening performance of biomarkers and ultimately the cost effectiveness of screening strategies. As DD‐NEF is rare in subjects without co‐morbid cardiovascular conditions, the efficiency of screening programmes could be optimised by targeting high‐risk groups, defined according to age (> 70 years) or risk factor status (hypertension, ischaemic heart disease, diabetes or obesity).
Conclusion
Diastolic dysfunction is common in the community and is often unaccompanied by overt symptoms and signs of CHF. Despite the absence of symptoms, subjects with advanced DD‐NEF have accompanying structural abnormalities that reflect an increased risk for adverse cardiovascular outcomes and have a reduced quality of life.
ACKNOWLEDGEMENTS
This study was supported by a grant from the Canberra Hospital Salaried Medical Officers' Private Practice Fund. The authors acknowledge the support and assistance during study conduct from Dr Ian Jeffery, Alice Kam and Pearle Taverner (research nurses), Kate Abhayaratna (research assistant) and Christine O'Reilly (sonographer), Siemens Ultrasound (Australia) and Roche Diagnostics (Australia).
Abbreviations
CHF - congestive heart failure
DD‐NEF - diastolic dysfunction and normal ejection fraction
EF - ejection fraction
LV - left ventricular, N‐BNP, amino‐terminal B‐type natriuretic peptide
Footnotes
Competing interests: None declared.
References
- 1.McDonagh T A, Morrison C E, Lawrence A.et al Symptomatic and asymptomatic left‐ventricular systolic dysfunction in an urban population. Lancet 1997350829–833. [DOI] [PubMed] [Google Scholar]
- 2.Mosterd A, Hoes A W, de Bruyne M C.et al Prevalence of heart failure and left ventricular dysfunction in the general population. The Rotterdam Study. Eur Heart J 199920447–455. [PubMed] [Google Scholar]
- 3.Davies M, Hobbs F, Davis R.et al Prevalence of left‐ventricular systolic dysfunction and heart failure in the Echocardiographic Heart of England Screening study: a population based study. Lancet 2001358439–444. [DOI] [PubMed] [Google Scholar]
- 4.Devereux R B, Roman M J, Paranicas M.et al A population‐based assessment of left ventricular systolic dysfunction in middle‐aged and older adults: the Strong Heart Study. Am Heart J 2001141439–446. [DOI] [PubMed] [Google Scholar]
- 5.Redfield M M, Jacobsen S J, Burnett J C., Jret al Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. JAMA 2003289194–202. [DOI] [PubMed] [Google Scholar]
- 6.Fischer M, Baessler A, Hense H W.et al Prevalence of left ventricular diastolic dysfunction in the community: results from a Doppler echocardiographic‐based survey of a population sample. Eur Heart J 200324320–328. [DOI] [PubMed] [Google Scholar]
- 7.Vasan R S, Larson M G, Benjamin E J.et al Congestive heart failure in subjects with normal versus reduced left ventricular ejection fraction: prevalence and mortality in a population‐based cohort. J Am Coll Cardiol 1999331948–1955. [DOI] [PubMed] [Google Scholar]
- 8.Kitzman D W, Gardin J M, Gottdiener J S.et al Importance of heart failure with preserved systolic function in patients > or = 65 years of age. CHS Research Group. Cardiovascular Health Study. Am J Cardiol 200187413–419. [DOI] [PubMed] [Google Scholar]
- 9.Gandhi S K, Powers J C, Nomeir A M.et al The pathogenesis of acute pulmonary edema associated with hypertension. N Engl J Med 200134417–22. [DOI] [PubMed] [Google Scholar]
- 10.Zile M R, Baicu C F, Gaasch W H. Diastolic heart failure: abnormalities in active relaxation and passive stiffness of the left ventricle. N Engl J Med 20043501953–1959. [DOI] [PubMed] [Google Scholar]
- 11.Gottdiener J S, McClelland R L, Marshall R.et al Outcome of congestive heart failure in elderly persons: influence of left ventricular systolic function. The Cardiovascular Health Study. Ann Intern Med 2002137631–639. [DOI] [PubMed] [Google Scholar]
- 12.Nishimura R A, Tajik A J. Evaluation of diastolic filling of left ventricle in health and disease: Doppler echocardiography is the clinician's Rosetta Stone. J Am Coll Cardiol 1997308–18. [DOI] [PubMed] [Google Scholar]
- 13.Ommen S R, Nishimura R A. A clinical approach to the assessment of left ventricular diastolic function by Doppler echocardiography: update 2003. Heart 200389(Suppl 3)iii18–iii23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Starling M R, Crawford M H, Sorensen S G.et al Comparative accuracy of apical biplane cross‐sectional echocardiography and gated equilibrium radionuclide angiography for estimating left ventricular size and performance. Circulation 1981631075–1084. [DOI] [PubMed] [Google Scholar]
- 15.Schiller N B, Shah P M, Crawford M.et al Recommendations for quantitation of the left ventricle by two‐dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two‐Dimensional Echocardiograms. J Am Soc Echocardiogr 19892358–367. [DOI] [PubMed] [Google Scholar]
- 16.Pritchett A M, Jacobsen S J, Mahoney D W.et al Left atrial volume as an index of left atrial size: a population‐based study. J Am Coll Cardiol 2003411036–1043. [DOI] [PubMed] [Google Scholar]
- 17.Criteria Committee of the New York Heart Association Nomenclature and criteria for diagnosis of the heart and great vessels. 9th ed. Boston: Little, Brown, 1994253–256.
- 18.Mosterd A, Deckers J W, Hoes A W.et al Classification of heart failure in population based research: an assessment of six heart failure scores. Eur J Epidemiol 199713491–502. [DOI] [PubMed] [Google Scholar]
- 19.Vaziri S M, Larson M G, Benjamin E J.et al Echocardiographic predictors of nonrheumatic atrial fibrillation. The Framingham Heart Study. Circulation 199489724–730. [DOI] [PubMed] [Google Scholar]
- 20.Tsang T S, Barnes M E, Bailey K R.et al Left atrial volume: important risk marker of incident atrial fibrillation in 1655 older men and women. Mayo Clin Proc 200176467–475. [DOI] [PubMed] [Google Scholar]
- 21.Barnes M E, Miyasaka Y, Seward J B.et al Left atrial volume in the prediction of first ischemic stroke in an elderly cohort without atrial fibrillation. Mayo Clin Proc 2004791008–1014. [DOI] [PubMed] [Google Scholar]
- 22.Gardin J M, McClelland R, Kitzman D.et al M‐mode echocardiographic predictors of six‐ to seven‐year incidence of coronary heart disease, stroke, congestive heart failure, and mortality in an elderly cohort (the Cardiovascular Health Study). Am J Cardiol 2001871051–1057. [DOI] [PubMed] [Google Scholar]
- 23.Benjamin E J, D'Agostino R B, Belanger A J.et al Left atrial size and the risk of stroke and death. The Framingham Heart Study. Circulation 199592835–841. [DOI] [PubMed] [Google Scholar]
- 24.Petrie M C, Caruana L, Berry C.et al “Diastolic heart failure” or heart failure caused by subtle left ventricular systolic dysfunction? Heart 20028729–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yip G, Wang M, Zhang Y.et al Left ventricular long axis function in diastolic heart failure is reduced in both diastole and systole: time for a redefinition? Heart 200287121–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yu C M, Lin H, Yang H.et al Progression of systolic abnormalities in patients with “isolated” diastolic heart failure and diastolic dysfunction. Circulation 20021051195–1201. [DOI] [PubMed] [Google Scholar]
- 27.Nagueh S F, Middleton K J, Kopelen H A.et al Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol 1997301527–1533. [DOI] [PubMed] [Google Scholar]
- 28.Leite‐Moreira A F, Correia‐Pinto J, Gillebert T C. Afterload induced changes in myocardial relaxation: a mechanism for diastolic dysfunction. Cardiovasc Res 199943344–353. [DOI] [PubMed] [Google Scholar]
- 29.Kass D A, Bronzwaer J G, Paulus W J. What mechanisms underlie diastolic dysfunction in heart failure? Circ Res 2004941533–1542. [DOI] [PubMed] [Google Scholar]