“It is ironic and instructive that in the age of cellular and molecular biology, great advances in our understanding of the pathophysiology of cardiovascular disease continue to be made by pathologists who perform meticulous and imaginative studies”—Heistad.1
Acute coronary syndromes, including unstable angina, myocardial infarction, and sudden ischaemic death, are a leading cause of morbidity and mortality in the Western world. Current pharmacological and mechanical (angioplasty, bypass surgery, stenting) interventions have been effective, but treatment can be improved with more potent pharmacologic strategies based on an understanding of the underlying pathogenic processes. Critical steps in the development of acute coronary syndromes are the disruption of atherosclerotic plaque and the superimposed formation of the platelet‐rich thrombus.2
ATHEROSCLEROTIC PLAQUE DESTABILISATION
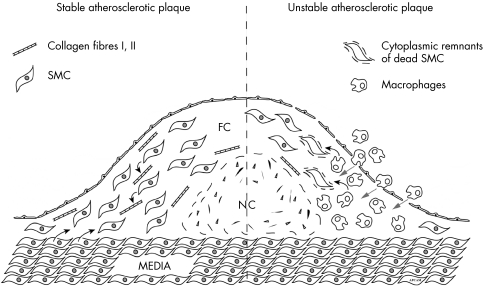
Atherosclerotic plaques differ widely in the relative content of major constituents: collagen, proteoglycans, intracellular lipid, and extracellular lipid, even within a single individual. Predominance of collagen and proteoglycans results in fibrous plaques that are more common in patients with stable coronary artery disease and have accordingly been designated as “stable” plaques (fig 1). Lipid‐rich or “vulnerable” plaques contain a substantial core of lipids separated from the circulation by thin, fibrous caps. A lipid pool often contains collagen, which lends mechanical stability to fibrous caps. The clinical significance of collagen lattice is demonstrated by the postmortem analysis of disrupted plaques in patients who have died of occlusive coronary thrombosis.3 In the great majority of these subjects, fissured plaques contain an extracellular lipid pool but lack collagen. In cases where a lipid pool was not involved, plaque disruptions occurred between collagen layers of fibrous plaques. High lipid content of the atherosclerotic plaque therefore predisposes to a more progressive development of ischaemic heart disease.
Figure 1 Stable versus unstable atherosclerotic plaques. FC, fibrous cap; NC, necrotic core; SMC, smooth muscle cells.
The strength of the fibrous cap separating the core of lipid‐rich lesions from the blood is proportional to its thickness, and this strength influences the probability of plaque rupture.3 Plaques with thicker caps are more resistant to fissuring and to progression of stable disease to an acute coronary syndrome. Major protein components of the fibrous cap are collagen and elastin.
Factors that impair the synthesis of collagen or accelerate its degradation have been proposed to contribute to the weakening of the fibrous cap. An important finding is the higher frequency of macrophage‐rich areas in plaques of patients with unstable angina and non‐Q wave myocardial infarction.4,5 Macrophages may release lytic enzymes that degrade the fibrous cap and therefore produce rupture of the atherosclerotic plaque.
APOPTOSIS AND PLAQUE RUPTURE
Another interesting finding is that cell death in atherosclerosis depends on the stage of the plaque, localisation, and the cell types involved.6 Both macrophages and smooth muscle cells (SMCs) undergo apoptosis in unstable atherosclerotic plaques. Apoptosis of macrophages is mainly present in regions showing signs of DNA synthesis/repair. SMC apoptosis is mainly present in less cellular regions and is not associated with DNA synthesis/repair. Even in early stages of atherosclerosis, SMCs become susceptible to apoptosis since they increase different pro‐apoptotic factors. Micro‐array studies revealed that several pro‐apoptotic genes are upregulated in atherosclerotic plaques.7 This might explain the increased susceptibility of plaque SMCs to undergoing apoptosis. Moreover, recent data indicate that SMCs may be killed by activated macrophages. The loss of SMCs can be detrimental for plaque stability since most of the interstitial collagen fibres, which are important for the tensile strength of the fibrous cap, are produced by SMCs.
Apoptosis of macrophages could be beneficial for plaque stability if apoptotic bodies are removed. Apoptotic cells that are not scavenged in the plaque activate thrombin which could further induce intraplaque thrombosis. Recent data from our group show that the clearance of apoptotic bodies is indeed strongly decreased in atherosclerotic plaques.
It can be concluded that apoptosis in primary atherosclerosis is detrimental since it could lead to plaque rupture and thrombosis. Pharmaco‐pathological data indicate that apoptosis decreased after lipid lowering which could be important in our understanding of the cell biology of plaque stabilisation.
INTRAPLAQUE HAEMORRHAGES AND PLAQUE RUPTURE
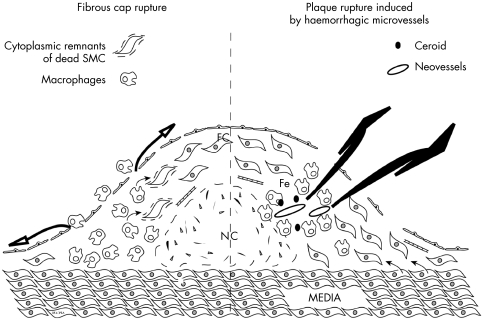
In normal arteries, microvessels (vasa vasorum) are observed only in adventitia and in the outer media of the aorta and its largest branches. Neovascularisation in atherosclerotic arteries occurs primarily by growth from the adventitia, as well as from the arterial lumen, into the intima of advanced plaques. New vasa in plaques appear fragile and may be susceptible to rupture (intraplaque haemorrhage) with a sudden increase in the size of the plaque.1 Repeated cycles of plaque rupture and healing probably explain the finding that there is layering in arterial plaques, which reflects the intermittent pattern of growth of the plaque (fig 2).
Figure 2 Fibrous cap rupture versus plaque rupture induced by haemorrhagic microvessels.
More recently, it was demonstrated by cardiovascular pathologists that these haemorrhagic microvessels could induce foam cell formation by platelet and erythrocyte phagocytosis.8,9 Interestingly this process was associated with macrophage activation, nitric oxide synthase (iNOS) induction, and cell death.8 Therefore it can be concluded that intraplaque haemorrhages trigger multiple processes of plaque destabilisation and plaque rupture.
All these recent histopathological findings will increase our knowledge of the critical underlying pathogenic processes of plaque rupture and could lead to more potent pharmacologic strategies to prevent acute coronary syndromes.
References
- 1.Heistad D D. Unstable coronary‐artery plaques. N Engl J Med 20033492285–2287. [DOI] [PubMed] [Google Scholar]
- 2.Davies M J. A macro and micro view of coronary vascular insult in ischemic heart disease. Circulation 199082(suppl II)II38–II46. [PubMed] [Google Scholar]
- 3.Richardson P D, Davies M J, Born G V R. Influence of plaque configuration and stress distribution on fissuring of coronary atherosclerotic plaques. Lancet 19892941–944. [DOI] [PubMed] [Google Scholar]
- 4.Moreno P R, Falk E, Palacios I F.et al Macrophage infiltration in acute coronary syndromes. Implications for plaque rupture. Circulation 199490775–778. [DOI] [PubMed] [Google Scholar]
- 5.Falk E. Why do plaques rupture? Circulation 199286(suppl III)III30–III42. [PubMed] [Google Scholar]
- 6.Kockx M M, De Meyer G R, Muhring J.et al Apoptosis and related proteins in different stages of human atherosclerotic plaques. Circulation 1998972307–2315. [DOI] [PubMed] [Google Scholar]
- 7.Martinet W, Schrijvers D L, De Meyer G R.et al Gene expression profiling of apoptosis‐related genes in human atherosclerosis: upregulation of death‐associated protein kinase. Arteriorscler Thromb Vasc Biol 2002222023–2029. [DOI] [PubMed] [Google Scholar]
- 8.Kockx M M, Cromheeke K M, Knaapen M W M.et al Phagocytosis and macrophage activation associated with hemorrhagic microvessels in human atherosclerosis. Arterioscler Thromb Vasc Biol 200323440–446. [DOI] [PubMed] [Google Scholar]
- 9.Kolodgie F D, Gold H K, Burke A P.et al Intraplaque hemorrhage and progression of coronary atheroma. N Engl J Med 20033492316–2325. [DOI] [PubMed] [Google Scholar]