Abstract
Objective
To recalibrate an existing Framingham risk score to produce a web‐based tool for estimating the 10‐year risk of coronary heart disease (CHD) and cardiovascular disease (CVD) in seven British black and minority ethnic groups.
Design
Risk prediction models were recalibrated against survey data on ethnic group risk factors and disease prevalence compared with the general population. Ethnic‐ and sex‐specific 10‐year risks of CHD and CVD, at the means of the risk factors for each ethnic group, were calculated from the product of the incidence rate in the general population and the prevalence ratios for each ethnic group.
Setting
Two community‐based surveys.
Participants
3778 men and 4544 women, aged 35–54, from the Health Surveys for England 1998 and 1999 and the Wandsworth Heart and Stroke Study.
Main outcome measures
10‐year risk of CHD and CVD.
Results
10‐year risk of CHD and CVD for non‐smoking people aged 50 years with a systolic blood pressure of 130 mm Hg and a total cholesterol to high density lipoprotein cholesterol ratio of 4.2 was highest in men for those of Pakistani and Bangladeshi origin (CVD risk 12.6% and 12.8%, respectively). CHD risk in men with the same risk factor values was lowest in Caribbeans (2.8%) and CVD risk was lowest in Chinese (5.4%). Women of Pakistani origin were at highest risk and Chinese women at lowest risk for both outcomes with CVD risks of 6.6% and 1.2%, respectively. A web‐based risk calculator (ETHRISK) allows 10‐year risks to be estimated in routine primary care settings for relevant risk factor and ethnic group combinations.
Conclusions
In the absence of cohort studies in the UK that include significant numbers of black and minority ethnic groups, this risk score provides a pragmatic solution to including people from diverse ethnic backgrounds in the primary prevention of CVD.
Targeting preventive interventions at those at highest risk is an accepted approach in the primary prevention of cardiovascular disease (CVD). Recommended risk‐scoring methods are derived from the Framingham Heart Study and feature in many charts, tables, computer programs, policy documents and guidelines.1,2,3,4,5,6,7 The rates of CVDs vary considerably between ethnic groups, which may be due to differential susceptibility to established risk factors along with exposure to “emerging” risk factors, although debate on whether genetic susceptibility is important continues.8,9,10,11,12
As the Framingham risk score has never been validated in British black and minority ethnic groups (BMEGs), there is little guidance on how to assess risk among these populations, excluding these people from the main risk assessment process and inhibiting consistent access to preventive treatment. For South Asians (those originating from India, Pakistan, Bangladesh and Sri Lanka), multiplying the Framingham score by a correction factor of 1.4 has been suggested,7 but this does not acknowledge the heterogeneity in CVD risk between people of South Asian origin.13 Recent guidance acknowledges that risk assessment in BMEGs is particularly unclear.5 It is essential for health equity reasons that accurate risk‐scoring systems be used to improve access of these populations to effective preventive treatments and to avoid over‐ or underdefinition of “at risk” status.
Prospective data from large numbers of American minority ethnic groups have been used to improve the accuracy of a Framingham score.14 Unfortunately, the same method cannot be directly applied in the UK due to insufficient longitudinal data on BMEGs. However, a considerable amount of cross‐sectional survey data on BMEGs provides information on their risk factor levels and prevalence of existing CVD. By using this cross‐sectional data, we developed a web‐based tool for calculating the 10‐year risk of coronary heart disease (CHD) and CVD in seven British BMEGs as well as that of the general population.
METHODS
To derive a new model for British BMEGs, we followed the methods of D'Agostino et al,14 who recalibrated an existing Framingham equation for different ethnic groups from the United States. In summary, the authors substituted the mean risk factor levels and the ratio of the survival estimates from specific cohort studies of ethnic minority populations for the corresponding values from the Framingham study, resulting in a new model for each of the ethnic groups. However, owing to the lack of prospective data on British BMEGs, we estimated the incidence rate from prevalence data for Indian, Pakistani, Bangladeshi, black Caribbean, Chinese and Irish populations from the Health Surveys for England 1998 and 1999, and from the Wandsworth Heart and Stroke Study for black Africans. Details are given below.
Health Surveys for England 1998 and 1999
The Health Surveys for England 1998 and 199915,16 are large‐scale surveys of a representative sample of adults and children from England and Wales. The 1999 survey included a “boost” component to increase the number of informants from six minority ethnic groups. We used risk factor data from men and women aged 35–54 for our study. The prevalence of CHD and CVD was also obtained for this age group.
Wandsworth Heart and Stroke Study
The Wandsworth Heart and Stroke Study17 is a population‐based cross‐sectional survey of 1577 men and women resident in a geographically defined area of London. The 523 white, 549 people of African origin, and 505 people of South Asian origin underwent comprehensive screening of physical measurements, a questionnaire, and blood and urine tests. For this analysis, we used only the risk factor and disease prevalence data from the black Africans aged between 35 and 54 years, as they were not represented in the Health Survey for England.
The definition of CHD was death from CHD (sudden or non‐sudden), myocardial infarction, angina pectoris and coronary insufficiency. The definition of CVD additionally includes stroke and transient ischaemia.
Statistical methods
Published data on CVD mortality and morbidity by ethnic group were used to assess risk of disease in each ethnic group relative to the general population.8 The standardised mortality ratio (SMR) for CVD for the ethnic groups showed a similar pattern to the age‐standardised prevalence ratio for CVD. Therefore, as adequate CVD incidence data by ethnic group are lacking, we substituted the prevalence ratio for the incidence ratio and used this as a multiplicative factor relating CVD risk in ethnic groups to that of the general population.
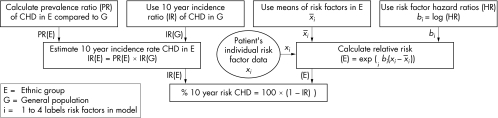
The sex‐specific and age‐standardised prevalence ratio for CHD and for CVD for each ethnic group compared with the general British population was obtained from the Health Surveys for England.15,16 As the prevalence ratios were not available for black Africans, the SMR had to be used instead.8 Separate risk scores were developed for CHD and CVD for both men and women of each ethnic group. Figure 1 illustrates the recalibration method applied to the Framingham risk score used in current guidelines1 and can be summarised in three steps: (1) estimating CHD/CVD incidence in the general population; (2) estimating CHD/CVD incidence in ethnic groups by using the prevalence ratios as a multiplicative adjusting factor; and (3) generating sex‐ and ethnic group‐specific models by using hazard ratios from British cohort studies. The consistency of hazard ratios for each risk factor used in the models was examined in four contemporary British cardiovascular cohort studies.18,19,20 Differences in mean levels of risk factors for each sex and ethnic‐specific group were also taken into account in the recalibration method. Further details of the method are described in the technical appendix, where we describe in detail the model for CHD risk in men.
Figure 1 Flow diagram illustrating the development of the ethnic group‐specific model for predicting 10‐year risk of coronary heart disease (CHD) based on recalibration of the standard Framingham model.
The models predict 10‐year risk of CHD and CVD for men and women, aged 35–74 years, according to their ethnic group, sex, age, systolic blood pressure, total and high density lipoprotein (HDL) cholesterol and smoking status. Patients who have diabetes, left ventricular hypertrophy or a history of CVD are excluded from this prediction model, as they are considered to be at high risk of CVD and already requiring risk factor control irrespective of their Framingham risk.
Sensitivity analyses
The 10‐year risks of CHD and CVD based on the upper and lower range of the 95% confidence intervals around the age‐standardised prevalence ratio were used in a sensitivity analysis to assess the precision of the risk estimates. The validity of using cross‐sectional prevalence data in this recalibration method was tested on data from two cohort studies with both prevalence and incidence data available. Further details are available in the technical appendix.
RESULTS
Tables 1 (men) and 2 (women) show the distribution of risk factors, CHD and CVD prevalences and prevalence ratios for BMEGs and the general British population. For men and women, blood total cholesterol concentrations were broadly similar across all groups, but HDL cholesterol concentrations were lowest in Bangladeshis. Systolic blood pressures were highest and comparable in male Indians, black Africans and the general population, and were lowest in Bangladeshis. Smoking prevalence varied greatly, with rates being highest (50%) among Bangladeshi men and only 4% in black African men. Among women, smoking rates were very low among all South Asian groups but were high among black Caribbeans, Irish and the general population. CVD prevalence ratios varied considerably: for men, the ratio was highest in Bangladeshis (1.39) and lowest among Chinese (0.49); for women, the ratio (1.33) was highest in Pakistanis and lowest (0.22) among Chinese.
Table 1 Means (proportions) of risk factors, prevalence and prevalence ratio for CHD and CVD by ethnic group for men aged 35–54*.
| Indian | Pakistani | Bangladeshi | All South Asian† | Chinese | Black Caribbean | Black African‡ | Irish§ | General population¶ | |
|---|---|---|---|---|---|---|---|---|---|
| Number | 263 | 205 | 149 | 617 | 132 | 137 | 51 | 247 | 2594 |
| Age (years) | 43.9 | 42.6 | 40.6 | 43.2 | 44.3 | 40.7 | 47.4 | 44.0 | 44.3 |
| Total cholesterol (mmol/l) | 5.7 | 5.3 | 5.4 | 5.6 | 5.4 | 5.3 | 5.3 | 5.6 | 5.6 |
| HDL cholesterol (mmol/l) | 1.2 | 1.1 | 1.0 | 1.2 | 1.4 | 1.4 | 1.3 | 1.3 | 1.3 |
| Log (cholesterol:HDL) | 1.6 | 1.6 | 1.8 | 1.6 | 1.4 | 1.4 | 1.4 | 1.5 | 1.6 |
| SBP (mm Hg) | 133.5 | 129.5 | 124.9 | 131.4 | 128.0 | 132.6 | 130.9 | 132.4 | 133.7 |
| Current smoker (%) | 23 | 31 | 50 | 28 | 21 | 48 | 4 | 42 | 30 |
| Waist:hip ratio | 0.94 | 0.94 | 0.93 | 0.94 | 0.90 | 0.87 | 0.91 | 0.92 | 0.92 |
| Body mass index (kg/m2) | 26.0 | 26.6 | 25.1 | 26.1 | 24.7 | 27.4 | 26.8 | 26.9 | 27.2 |
| SES (% manual) | 54% | 64% | 81% | 60% | 50% | 69% | 47% | 56% | 51% |
| Diabetes | 8.0% | 9.6% | 10.6% | 8.7% | 2.2% | 3.2% | 9.8% | 0.8% | 2.2% |
| CHD prevalence (doctor diagnosed MI, angina) | 4.1% | 4.6% | 2.8% | 4.1% | 1.6% | 0% | 2% | 2.9% | 5.2% |
| CHD prevalence ratio age adjusted (95% CI) | 1.31 (0.92 to 1.70) | 1.41 (0.88 to 1.94) | 1.53 (0.88 to 2.18) | 1.36 (1.07 to 1.65) | 0.34 (0.09 to 0.59) | 0.27 (0.09 to 0.45) | NA | 0.95 (0.62 to 1.28) | 1 |
| SMR** ICD‐9 410–414 (95% CI) age 20–74 | 142 (137 to 147) | 148 (138 to 158) | 151 (136 to 167) | 145 NA | 44 (36 to 54) | 62 (58 to 67) | 58 (47 to 70) | NA | 100 |
| CVD prevalence (CHD + stroke) | 4.7% | 5.9% | 3.9% | 4.9 % | 2.1% | 1.6 | 3.9 | 2.6% | 3.2% |
| CVD prevalence ratio age adjusted (95% CI) | 1.34 (0.97 to 1.71) | 1.32 (0.87 to 1.77) | 1.39 (0.82 to 1.96) | 1.34 (1.07 to 1.61) | 0.49 (0.16 to 0.82) | 0.61 (0.30 to 0.92) | NA | 0.95 (0.66 to 1.24) | 1 |
| SMR** ICD‐9 390–459 (95% CI) age 20–74 | 134 (130 to 139) | 139 (131 to 147) | 156 (143 to 170) | 138 (wt av) | 61 (53 to 70) | 95 (90 to 99) | 113 (100 to 128) | NA | 100 |
*Source: Health Survey for England—The Health of Minority Ethnic Groups '99 (http://www.archive.official‐documents.co.uk/document/doh/survey99/hse99.htm).
†All South Asian is a weighted mean base on population frequencies 6:3:1. This does not permit the calculation of 95% CIs around the standardised mortality ratio (SMR).
‡Data for black Africans is from the Wandsworth study. Numbers are too small to calculate meaningful prevalence ratios.
§No SMR data available for the Irish group.
¶Data for general population is from the Health Survey for England 1998.
**SMR for each sex by five‐year age group with the 1991 census data on population of England and Wales as the standard based on mortality data from the Office for National Statistics for the four‐year period 1989–1992. Source: http://hcna.radcliffe‐oxford.com/bemg.htm.
CHD, coronary heart disease; CVD, cardiovascular disease; HDL, high density lipoprotein; ICD‐9, International classification of diseases, 9th revision; MI, myocardial infarction; NA, not available; SBP, systolic blood pressure; SES, socioeconomic status; wt av, weighted average.
Table 2 Means (proportions) of risk factors, prevalence and prevalence ratio for CHD and CVD by ethnic group for women aged 35–54*.
| Indian | Pakistani | Bangladeshi | All South Asian† | Chinese | Black Caribbean | Black African‡ | Irish§ | General population¶ | |
|---|---|---|---|---|---|---|---|---|---|
| Number | 269 | 206 | 135 | 610 | 195 | 284 | 87 | 312 | 3056 |
| Age (years) | 43.0 | 42.6 | 43.7 | 43.0 | 44.0 | 41.4 | 47.6 | 43.5 | 42.9 |
| Total cholesterol (mmol/l) | 5.1 | 5.1 | 5.1 | 5.1 | 5.0 | 4.9 | 5.5 | 5.4 | 5.4 |
| HDL cholesterol (mmol/l) | 1.4 | 1.3 | 1.1 | 1.3 | 1.6 | 1.6 | 1.7 | 1.6 | 1.6 |
| Log (cholesterol:HDL) | 1.3 | 1.4 | 1.6 | 1.4 | 1.2 | 1.1 | 1.2 | 1.2 | 1.2 |
| SBP (mm Hg) | 124.5 | 126.2 | 127.7 | 125.3 | 124.7 | 127.8 | 133.6 | 125.1 | 127.5 |
| Current smoker | 3% | 4% | 2% | 3% | 8% | 27% | 2 | 36% | 30% |
| Waist:hip ratio | 0.82 | 0.86 | 0.87 | 0.84 | 0.81 | 0.82 | 0.82 | 0.80 | 0.79 |
| BMI (kg/m2) | 26.7 | 29.3 | 26.5 | 27.5 | 23.9 | 28.3 | 29.3 | 27.1 | 26.7 |
| SES (% manual) | 52% | 65% | 83% | 59% | 43% | 53% | 47% | 48% | 48% |
| Diabetes | 4.4% | 7.4% | 12.1% | 6.1% | 0.7% | 3.9% | 6.9% | 1.9% | 1.2% |
| CHD prevalence (doctor diagnosed MI, angina) | 0.7% | 2.5% | 2.8% | 1.5% | 0.3% | 1.6% | 1.2% | 1.8% | 2.4% |
| CHD prevalence ratio age adjusted (95% CI) | 0.77 (0.30 to 1.24) | 1.40 (0.62 to 2.18) | 0.97 (0.32 to 1.62) | 1.0 (0.65 to 1.35) | 0.16 (0 to 0.32) | 0.98 (0.51 to 1.45) | NA | 0.97 (0.52 to 1.42) | 1 |
| SMR** ICD‐9 410–414 (95% CI) age 20–74 | 158 (148 to 168) | 111 (93 to 130) | 91 (60 to 133) | 137 NA | 70 (57 to 85) | 86 (77 to 96) | 61 (37 to 94) | NA | 100 |
| CVD prevalence (CHD + stroke) | 1.3% | 2.7% | 4.6% | 2.1% | 0.3% | 1.6% | 3.5% | 1.8% | 1.9% |
| CVD prevalence ratio age adjusted (95% CI) | 0.78 (0.39 to 1.17) | 1.33 (0.70 to 1.96) | 0.93 (0.38 to 1.48) | 0.96 (0.61 to 1.31) | 0.22 (0 to 0.53) | 0.83 (0.46 to 1.20) | NA | 0.98 (0.61 to 1.35) | 1 |
| SMR** ICD‐9 390–459 (95% CI) age 20–74 | 149 (135 to 164) | 122 (108 to 137) | 107 (81 to 138) | 137 (NA) | 61 (53 to 70) | 137 (128 to 146) | 148 (119 to 181) | NA | 100 |
*Source: Health Survey for England—The Health of Minority Ethnic Groups '99 (http://www.archive.official‐documents.co.uk/document/doh/survey99/hse99.htm).
†All South Asian is a weighted mean base on population frequencies 6:3:1. This does not permit the calculation of 95% CIs around the standardised mortality ratio (SMR).
‡Data for black Africans is from the Wandsworth study. Numbers are too small to calculate meaningful prevalence ratios.
§No SMR data available for the Irish group.
¶Data for general population is from the Health Survey for England 1998.
**SMR for each sex by five‐year age group with the 1991 census data on population of England and Wales as the standard based on mortality data from the Office for National Statistics for the four‐year period 1989–1992. Source: http://hcna.radcliffe‐oxford.com/bemg.htm.
CHD, coronary heart disease; CVD, cardiovascular disease; HDL, high density lipoprotein; ICD‐9, International classification of diseases, 9th revision; MI, myocardial infarction; NA, not available; SBP, systolic blood pressure; SES, socioeconomic status.
Table 3 shows that the hazard ratios for each risk factor used in the model are consistent with those of four contemporary British cohort studies.18,19,20 The consistency of risk factor hazard ratios for both outcomes across these studies, together with the findings of a multiple ethnic group investigation,14 suggests that the hazard ratio estimates used in our models were reasonably robust to differences in source populations.
Table 3 Hazard ratios used in the recalibrated model with hazard ratios for CHD and CVD risk factors for BRHS, Caerphilly study, Speedwell study and BWHHS.
| BRHS* (n = 7001) | Caerphilly (n = 2197) | Speedwell (n = 2028) | BWHHS† (n = 3144) | Model HR | |
|---|---|---|---|---|---|
| Hazard ratio CHD‡ (95% CI) | |||||
| No of events | 493 | 199 | 165 | 160 | |
| Age (per 10 years) | 2.02 (1.71 to 2.38) | 1.59 (1.15 to 2.19) | 2.05 (1.41 to 2.98) | 1.54 (1.14 to 2.07) | 2.0 |
| Log (TC:HDL) | 4.05 (3.02 to 5.43) | 2.47 (1.67 to 3.63) | 2.33 (1.68 to 3.23) | 2.48 (1.53 to 4.03) | 2.5 |
| SBP (per 10 mm Hg) | 1.16 (1.12 to 1.21) | 1.14 (1.06 to 1.22) | 1.16 (1.09 to 1.23) | 1.07 (1.00 to 1.13) | 1.1 |
| Current smoker | 1.62 (1.36 to 1.94) | 1.78 (1.35 to 2.37) | 1.29 (0.94 to 1.75) | 2.01 (1.35 to 2.98) | 1.6 |
| Hazard ratio CVD‡ (95% CI) | |||||
| Number of events | 632 | 246 | 212 | 200 | |
| Age (per 10 years) | 2.15 (1.86 to 2.50) | 1.78 (1.33 to 2.38) | 2.21 (1.58 to 3.09) | 1.65 (1.26 to 2.16) | 2.1 |
| Log (TC:HDL) | 3.03 (2.32 to 3.65) | 2.12 (1.50 to 3.01) | 2.05 (1.52 to 2.76) | 2.20 (1.43 to 3.40) | 2.2 |
| SBP (per 10 mm Hg) | 1.20 (1.16 to 1.24) | 1.15 (1.08 to 1.22) | 1.19 (1.13 to 1.25) | 1.05 (0.99 to 1.11) | 1.2 |
| Current smoker | 1.81 (1.55 to 2.12) | 1.92 (149 to 2.48) | 1.40 (1.07 to 1.83) | 2.50 (1.79 to 3.50) | 1.8 |
*Follow up was censored at 10 years in the men's cohorts of the British Regional Heart Study (BRHS), the Caerphilly Study and the Speedwell Study.
†The median follow up was 4.7 years (range 3.4–5.7 years) for women in the British Women's Heart and Health Study (BWHHS) and the age group was older than in the men's cohorts.
‡Coronary heart disease (CHD) and cardiovascular disease (CVD) excluded those with a prior diagnosis of myocardial infarction, stroke and diabetes from the analysis.
HDL, high density lipoprotein; HR, hazard ratio; SBP, systolic blood pressure; TC, total cholesterol.
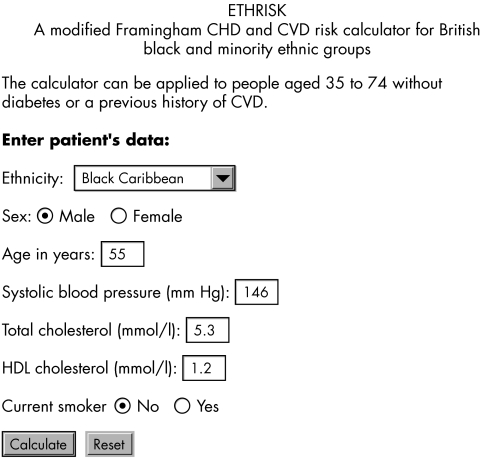
Table 4 (men) and table 5 (women) show examples of the 10‐year risk of CHD and CVD for the seven ethnic groups, as well as a composite South Asian group and, for comparison, the Framingham risk score, for a man and a woman with a systolic blood pressure of 130 mm Hg, total cholesterol of 5.5 mmol/l, and HDL cholesterol of 1.3 mmol/l at ages 40, 50, and 60 and for smokers and non‐smokers. For men, the 10‐year risk for both outcomes was highest for those of Pakistani and Bangladeshi origin, with the risk in Indians a little lower; CHD risk was lowest in black Caribbeans and CVD risk was lowest in Chinese. For women, those of Pakistani origin were at highest risk, with Chinese women being at very low risk. An interactive web‐based calculator (ETHRISK) is available at http://www.epi.bris.ac.uk/CVDethrisk/. ETHRISK is designed for use in the primary care setting to predict 10‐year risk of CHD and CVD for all relevant risk factor and ethnic group combinations. Figure 2 shows a screen image of ETHRISK.
Table 4 Example of the output from the model: 10‐year risk of a CHD event and a CVD event by ethnic group for a man with systolic blood pressure 130 mm Hg, cholesterol 5.5 mmol/l and HDL cholesterol 1.3 mmol/l at ages 40, 50 and 60 and for non‐smoker and smoker.
| Non‐smoker | Smoker | |||||
|---|---|---|---|---|---|---|
| 40 | 50 | 60 | 40 | 50 | 60 | |
| 10‐year risk of CHD event (%) | ||||||
| Indian | 5.0 (3.5–6.5) | 9.8 (6.8–12.6) | 18.5 (13.1–23.5) | 7.9 (5.5–10.2) | 15.2 (10.7–19.3) | 27.9 (20.2–34.9) |
| Pakistani | 5.9 (3.6–8.1) | 11.3 (7.1–15.5) | 21.3 (13.6–28.5) | 9.2 (5.7–12.6) | 17.5 (11.1–23.6) | 31.8 (20.9–41.5) |
| Bangladeshi | 5.8 (3.3–8.4) | 11.3 (6.5–16.0) | 21.2 (12.5–29.4) | 9.2 (5.2–13.1) | 17.4 (10.1–24.3) | 31.7 (19.2–42.7) |
| All South Asian | 5.3 (4.1–6.4) | 10.3 (8.1–12.4) | 19.5 (15.4–23.2) | 8.4 (6.5–10.1) | 16.0 (12.6–19.1) | 29.3 (23.5–34.5) |
| Chinese | 1.6 (0.4–2.7) | 3.1 (0.9–5.4) | 6.1 (1.7–10.4) | 2.5 (0.7–4.3) | 4.9 (1.4–8.4) | 9.6 (2.7–16.1) |
| Caribbean | 1.4 (0.5–2.2) | 2.8 (0.9–4.4) | 5.4 (1.8–8.6) | 2.2 (0.7–3.6) | 4.4 (1.5–7.0) | 8.5 (2.9–13.4) |
| Black African | 2.3 (1.9–2.8) | 4.6 (3.7–5.5.) | 8.9 (7.3–10.7) | 3.7 (3.0–4.5) | 7.2 (5.9–8.7) | 13.9 (11.5–16.6) |
| Irish | 3.6 (2.3–4.9) | 7.1 (4.6–9.5) | 13.7 (8.9–18.0) | 5.7 (3.7–7.7) | 11.1 (7.2–14.7) | 20.9 (13.9–27.2) |
| Framingham score | 3.6 | 7.2 | 11.8 | 6.5 | 12.0 | 18.2 |
| 10‐year risk of CVD event (%) | ||||||
| Indian | 5.6 (4.0–7.2) | 11.4 (8.3–14.5) | 22.4 (16.5–28.0) | 9.9 (7.1–12.6) | 19.6 (14.4–24.7) | 36.7 (27.8–44.8) |
| Pakistani | 6.2 (4.1–8.4) | 12.6 (8.4–16.9) | 24.7 (16.8–32.1) | 11.0 (7.3–14.7) | 21.6 (14.6–28.3) | 40.0 (28.2–50.2) |
| Bangladeshi | 6.3 (3.7–9.0) | 12.8 (7.6–17.9) | 24.9 (15.3–33.9) | 11.1 (6.6–15.6) | 21.9 (13.3–30.0) | 40.4 (25.8–52.6) |
| All South Asian | 5.9 (4.7–7.2) | 12.1 (9.7–14.4) | 23.6 (19.2–27.8) | 10.5 (8.4–12.5) | 20.7 (16.8–24.5) | 38.5 (32.0–44.5) |
| Chinese | 2.6 (0.8–4.5) | 5.4 (1.7–9.1) | 11.1 (3.6–18.1) | 4.7 (1.5–7.9) | 9.6 (3.1–15.8) | 19.1 (6.4–30.3) |
| Caribbean | 3.2 (1.6–4.8) | 6.6 (3.2–9.9) | 13.3 (6.7–19.6) | 5.7 (2.8–8.6) | 11.6 (5.8–17.1) | 22.7 (11.7–32.6) |
| Black African | 5.0 (3.9–6.5) | 10.1 (8.0–13.1) | 20.1 (16.1–25.5) | 8.8 (6.9–11.4) | 17.6 (14.0–22.4) | 33.3 (27.1–41.2) |
| Irish | 3.9 (2.7–5.1) | 8.0 (5.6–10.4) | 16.0 (11.3–20.6) | 6.9 (4.8–9.0) | 13.9 (9.8–18.0) | 27.0 (19.4–34.0) |
| Framingham score | 4.1 | 8.4 | 14.1 | 7.5 | 14.1 | 22.3 |
Range in brackets estimated by substituting 95% limits of the confidence interval of the prevalence ratio.
CHD, coronary heart disease; CVD, cardiovascular disease; HDL, high density lipoprotein.
Table 5 Example of the output from the model: 10‐year risk of a CHD event and a CVD event by ethnic group for a woman with systolic blood pressure 130 mm Hg, cholesterol 5.5 mmol/l and HDL cholesterol 1.3 mmol/l at ages 40, 50 and 60 and for non‐smoker and smoker.
| Non‐smoker | Smoker | |||||
|---|---|---|---|---|---|---|
| 40 | 50 | 60 | 40 | 50 | 60 | |
| 10‐year risk of CHD event (%) | ||||||
| Indian | 1.6 (0.6–2.5) | 3.2 (1.2–4.9) | 6.4 (2.3–9.6) | 2.6 (0.9–4.0) | 5.1 (1.8–7.8) | 10.0 (3.6–14.9) |
| Pakistani | 2.6 (1.2–4.1) | 5.1 (2.3–8.0) | 9.8 (4.5–15.3) | 4.1 (1.8–6.4) | 8.0 (3.6–12.4) | 15.3 (7.1–23.3) |
| Bangladeshi | 1.4 (0.5–2.3) | 2.7 (0.9–4.6) | 5.3 (1.9–8.9) | 2.2 (0.8–3.7) | 4.3 (1.5–7.2) | 8.3 (3.0–13.8) |
| All South Asian | 1.8 (1.2–3.8) | 3.6 (2.4–7.4) | 7.1 (4.8–14.1) | 2.9 (1.9–5.9) | 5.7 (3.8–11.5) | 11.1 (7.5–21.6) |
| Chinese | 0.3 (0.0–0.7) | 0.6 (0.0–1.3) | 1.1 (0.0–2.7) | 0.5 (0.0–1.1) | 0.9 (0.0–2.1) | 1.8 (0.0–4.2) |
| Caribbean | 2.2 (1.2–3.4) | 4.4 (2.4–6.6) | 8.6 (4.8–12.7) | 3.6 (2.0–5.3) | 7.0 (3.9–10.3) | 13.4 (7.6–19.5) |
| Black African | 0.9 (0.6–1.4) | 1.8 (1.1–2.8) | 3.6 (2.2–5.5) | 1.5 (0.9–2.3) | 2.9 (1.8–4.5) | 5.7 (3.6–8.7) |
| Irish | 1.7 (1.0–2.6) | 3.4 (1.9–5.1) | 6.8 (3.8–10.0) | 2.8 (1.5–4.2) | 5.5 (3.0–8.1) | 10.6 (5.9–15.5) |
| Framingham score | 1.7 | 4.6 | 7.1 | 3.4 | 8.1 | 11.7 |
| 10‐year risk of CVD event (%) | ||||||
| Indian | 2.0 (1.1–3.1) | 4.2 (2.2–6.4) | 8.7 (4.6–13.0) | 3.7 (1.9–5.5) | 7.5 (4.0–11.3) | 15.1 (8.2–22.2) |
| Pakistani | 3.2 (1.7–4.7) | 6.6 (3.5–9.7) | 13.4 (7.2–19.2) | 5.7 (3.0–8.4) | 11.6 (6.3–16.8) | 22.8 (12.7–32.0) |
| Bangladeshi | 1.7 (0.7–2.8) | 3.6 (1.4–5.7) | 7.4 (3.0–11.7) | 3.1 (1.2– 5.0) | 6.4 (2.6–10.1) | 13.0 (5.4–20.0) |
| All South Asian | 2.3 (1.5–3.1) | 4.8 (3.1–6.4) | 9.7 (6.5–12.9) | 4.1 (2.7–5.5) | 8.4 (5.6–11.2) | 16.9 (11.3–22.1) |
| Chinese | 0.6 (0.0–1.3) | 1.2 (0.0–2.8) | 2.5 (0.0–5.7) | 1.0 (0.0–2.4) | 2.1 (0.0–4.9) | 4.4 (0.0–10.0) |
| Caribbean | 2.3 (1.3–3.4) | 4.8 (2.6–6.9) | 9.7 (5.4–13.9) | 4.1 (2.3–6.0) | 8.4 (4.7–12.1) | 16.9 (9.5–23.7) |
| Black African | 2.6 (1.7–3.9) | 5.3 (3.5–8.0) | 10.8 (7.1–15.9) | 4.6 (3.0–6.9) | 9.4 (6.2–13.9) | 18.7 (12.5–26.9) |
| Irish | 2.2 (1.3–3.0) | 4.5 (2.8–6.1) | 9.1 (5.7–12.5) | 3.8 (2.4–5.3) | 7.9 (4.9–10.8) | 15.8 (10.0–21.3) |
| Framingham score | 2.1 | 5.5 | 8.7 | 4.1 | 9.7 | 14.7 |
Range in brackets estimated by substituting 95% limits of the confidence interval of the prevalence ratio.
CHD, coronary heart disease; CVD, cardiovascular disease; HDL, high density lipoprotein.
Figure 2 The ETHRISK coronary heart disease (CHD) and cardiovascular disease (CVD) risk calculator for different British ethnic groups (available at http://www.epi.bris.ac.uk/CVDethrisk/).
Sensitivity analyses
Tables 4 and 5 show the impact of survey sample size on precision of the estimates of CHD and CVD risk, by showing the predictions obtained from substituting the lower and upper 95% confidence intervals of the prevalence ratios in the model. The precision is greater in the larger groups with higher prevalence and is least in the smallest groups at lowest risk. For example, with the lower point of the 95% confidence interval, the estimated 10‐year CHD risk of a 60‐year‐old Indian male smoker is 20.2% and 34.9% with the upper point. However, the estimated risk for a Chinese woman of the same age and smoking status ranges from 0–4.2%. In general, few CVD events were recorded for women in the survey data, so the prevalence ratios, and consequently this model, are less precise for women.
The technical appendix and web table 1 (available on the Heart website—http://www.heartjnl.com/supplemental) show the results from the test of “proof of principle” in prospective populations.
DISCUSSION
In the absence of large‐scale investment in cohort studies for BMEGs in the UK, we have used a range of data sources to predict CHD and CVD risk among populations of BMEGs free of CVD on the basis of risk factors used in the Framingham risk score. We have developed a web‐based risk calculator for estimating the 10‐year risk of CHD and CVD in seven ethnic groups that may be applied in routine primary care settings. This is a major advance from existing guidance that does not account for heterogeneity between South Asians or between the sexes and offers no guidance for other ethnic groups.
Strengths and weaknesses
We used a method from a validated recalibration technique14 and adapted it for use with prevalence data. This method was reasonably accurate in subgroups of prospective populations in which both the prevalence and incidence of CHD were known. This suggests that the method is acceptably transferable between populations. We used hazard ratios for the risk factors consistent with those from four British prospective studies, and these relationships between risk factors and outcomes have been shown to be reasonably consistent across national and ethnic groups.14,21
Prevalence estimates for both CHD and CVD were used, as risks of each outcome differ between ethnic groups.22 We assumed that data on people aged 35–54 would be most suited to constructing the models, as younger age groups have little prevalent CVD. The prevalence in older age groups may be affected by differential case fatality in different ethnic groups, but there would be few deaths from CVD below the age of 55. Where possible, prevalence ratios were chosen in preference to SMRs to reduce misclassification of ethnicity, as death certificates record country of birth, not ethnicity, and because of the possible influence of differential case fatality between ethnic groups. We extrapolated the models to include patients up to 74 years, as the Framingham risk scores on which they are based can be estimated up to this age. As the SMR was similar to the prevalence ratio across the ethnic groups, we assumed that extrapolation of the prevalence ratio to the older age group was reasonable. The Wandsworth study was used to permit inclusion of black Africans, although it should be recognised that black Africans, like South Asians, are a heterogeneous group. The means of the risk factors in the Health Survey for England and the Wandsworth study for the ethnic groups they both surveyed were consistent, so the values for the black Africans from this study are likely to be generalisable to the UK23,24 (data are available from the authors.) However, people who declined to participate in the surveys may not be representative of patients who attend general practices.
The predicted disease rates are imprecise, particularly in women, due to the small amount of available data on CHD and CVD prevalence by ethnic group. However, presenting the 95% confidence intervals of the prevalence ratios and their impact on the risk estimates is an advance on existing risk scores that give no indication of their precision.2,3,4,5,6,7,25 The performance of new prediction rules should be evaluated prospectively in different populations26 but, owing to the lack of large‐scale prospective cohort data on CVD in BMEGs, this was not possible. Examining the proof of principle of the method applied to other groups of differing CVD risk was the closest alternative we could use.
We chose not to include diabetes or left ventricular hypertrophy as risk factors in our model even though they are included in the standard Framingham tool. Although diabetes is an important risk factor, especially among South Asians, formal risk assessment of patients with diabetes may not be necessary, as, once identified, these patients should receive attention to all their CVD risk factors irrespective of predicted risk.6 We also did not include measures of central obesity, such as waist to hip ratio, which previous research has found to be independently associated with CVD risk,27 as it is not included in the Framingham risk tool and therefore could not be included in this recalibrated Framingham model. Although this risk factor may be particularly relevant to South Asians, as they are known to be at high risk of insulin resistance and glucose intolerance, to estimate the effect of including waist hip ratio would require prospective data, which are not available.
Previous studies
This is the first study that has devised a risk calculator ready for primary care teams that presents absolute risk for seven different ethnic groups with the existing Framingham score. Two recent studies have compared predicted CHD with that expected by using mortality rates among South Asians. One found discrepancies between predicted risks by ethnic group and SMR by country of birth.28 The other reported that both the Framingham and FINRISK models gave similar rankings, unlike the SCORE model.29 Cappuccio et al22 compared predicted CHD and CVD risk in white, African and South Asian ethnic groups, concluding that using current CHD thresholds would underestimate CVD risk in people of South Asian and African origin. Lastly, a recent study found that adding 10 years to the age was the simplest way of making the estimated Framingham risk match an assumed excess risk of 1.79 among South Asians.30
Implications and further research
As minority ethnic communities tend to cluster in deprived urban areas,8 our risk calculator is a considerable advance on existing ad hoc guidance for clinicians in targeting the primary prevention of CVD in these localities. We do not expect the estimates from this model to be applicable to ethnic groups outside Britain. However, this novel method can be applied to other populations and countries possessing cross‐sectional, but lacking longitudinal, data to provide ethnic‐specific risk estimates. The precision of our risk estimates may be further improved when larger datasets become available. Our model also requires validation with prospective data. This may be achieved by using data routinely collected from primary care practices serving large ethnic minority populations. Much of these data are already being collected for quality assurance and payment reasons; however, this application requires the routine recording of ethnicity within primary care.31
Conclusion
Precisely accurate risk estimations across populations that vary in their risk over time are an unrealistic goal, as prognostic models are necessarily trailing indicators of present risk. The ideal situation would be to link risk calculators to primary care records to enable updating of estimates with recently collected data. However, given that the limitations of our risk‐scoring method are acknowledged, we provide a pragmatic solution to including some BMEGs in the primary prevention process.
Supplemental table appears on the Heart website—http://www.heartjnl.com/supplemental
Supplementary Material
ACKNOWLEDGEMENTS
We thank Richard Morris and Peter Whincup for providing data from the British Regional Heart Study, Paola Primatesta for her assistance with the Health Survey for England, Rita Patel for providing data from the British Women's Heart and Health Study, Yoav ben Shlomo for providing data from the Caerphilly and Speedwell studies and Raj Bhopal for providing comparison data from the Newcastle Heart Project and helpful comments on a draft of this paper.
Abbreviations
BMEG - black and minority ethnic group
CHD - coronary heart disease
CVD - cardiovascular disease
HDL - high density lipoprotein
SMR - standardised mortality ratio
TECHNICAL APPENDIX: STATISTICAL METHODS
RECALIBRATION PROCEDURE
We describe in detail the three‐step recalibration method applied to the Framingham model for CHD risk in men. The flow diagram given in fig 1 also illustrates the method. In our notation G refers to the general population and E refers to the ethnic group population.
Step 1. Estimating CHD/CVD incidence in general population
Estimate 10‐year incidence rate of CHD in the general British population (IR[G]) by inputting the mean levels of risk factors in the general population (given in table 1) into the Framingham risk score: (IR[G] = 6.54%).1
Step 2. Estimating CHD/CVD incidence in ethnic groups by adjusting by prevalence ratios
For each ethnic group, estimate the 10‐year incidence rate of CHD (IR[E]) at ethnic group‐specific means of risk factors, by multiplying the estimated general population 10‐year incidence rate (IR[G]) by the ethnic group‐specific prevalence (or mortality) ratio (PR[E]): IR[E] = IR[G]×PR[E]
Step 3. Generating sex‐ and ethnic‐specific models by using hazard ratios from British cohort studies
Construct risk prediction models by using the ethnic‐ and sex‐specific mean risk factor levels and the corresponding estimates of incidence rates, together with risk factor hazard ratios estimated from existing British cohort studies given in table 2.
TEST OF “PROOF OF PRINCIPLE” IN PROSPECTIVE POPULATIONS
The validity of using cross‐sectional prevalence data in this recalibration method was tested on data from populations with both prevalence and incidence data available. Models were derived from only prevalence data to predict the CHD and CVD rates in higher‐risk subpopulations defined by four different risk factors that are not in the Framingham score (socioeconomic position, height, body mass index (BMI) and geographical area). Predictions of the CHD and CVD rates from the model were then compared with the observed rates in each dataset. Men from the Caerphilly Study were divided into non‐manual and manual (higher risk), and into groups who were above or below (higher risk) 170 cm tall.19 Similarly, men from the British Regional Heart Study were divided into those below and above (higher risk) a BMI of 27 kg/m, and from the south of England versus the rest (higher risk).20
Web table 1 (available on the Heart website at http://www.heartjnl.com/supplemental) shows the results of applying our method to cross‐sectional data in different subgroups of the two cohort studies and comparing the risk estimates produced from the model with observed incidence rates. The error between the predicted CHD rate and the observed ranged from 1.9%, when using prevalence ratios and risk factor information from men with low BMI to predict the rate in the high BMI group, to 21.7%, when predicting risk in people not from the south and using relevant data from those in the south of UK, in the British Regional Heart Study.
Footnotes
This study was funded by a grant from the British Heart Foundation (reference number PG/03/160) and PB was funded by a Wellcome Trust training fellowship in health services research. BWHHS and BRHS are funded by the (UK) Department of Health and the British Heart Foundation. The Caerphilly & Speedwell Study is supported by grants from the MRC and NHS Research & Development programme and the Alzheimer's Disease Society. The views expressed in this publication are those of the authors and not necessarily those of any of the funding bodies. The funding bodies have had no influence over the scientific work or its publication.
Competing interests: None declared.
Ethics: This study had approval from the United Bristol Healthcare Trust local research ethics committee (E5759)
Contributions: PB had the idea for the study, obtained funding, developed the study aim and drafted the paper. MM designed the statistical model, performed the analysis and drafted the methods sections with PB. MM, PG, FC, RD'A and SE developed the study aim and with CF contributed to the writing of the paper. PB and MM will act as guarantors.
Supplemental table appears on the Heart website—http://www.heartjnl.com/supplemental
References
- 1.Anderson K M, Odell P M, Wilson P W.et al Cardiovascular disease risk profiles. Am Heart J 1990121293–298. [DOI] [PubMed] [Google Scholar]
- 2.Sheridan S, Pignone M, Mulrow C. Framingham‐based tools to calculate the global risk of coronary heart disease: a systematic review of tools for clinicians. J Gen Intern Med 2003181039–1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anon National Cholesterol Education Program. Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Full Report. http://www.nhlbi.nih.gov/guidelines/cholesterol/atp3_rpt.htm (accessed 24 Jul 2006)
- 4.Anon National Service Framework for Coronary Heart Disease. London: Department of Health, 2000
- 5.Anon North of England Hypertension Guideline Development Group. Essential hypertension: managing adult patients in primary care (NICE guideline). Newcastle upon Tyne: University of Newcastle upon Tyne, 2004 [PubMed]
- 6.Williams B, Poulter N R, Brown M J.et al Guidelines for management of hypertension: report of the fourth working party of the British Hypertension Society, 2004‐BHS IV. J Hum Hypertens 200418139–185. [DOI] [PubMed] [Google Scholar]
- 7.Anon Joint British recommendations on prevention of coronary heart disease in clinical practice. British Cardiac Society, British Hyperlipidaemia Association, British Hypertension Society, endorsed by the British Diabetic Association. Heart 199880(Suppl 2)S1–29. [PMC free article] [PubMed] [Google Scholar]
- 8.Gill P S, Kai J, Bhopal R.et al Health care needs assessment: black and minority ethnic groups. In: Raftery J, Stevens A, Mant J, eds. Health care needs assessment: the epidemiological based needs assessment reviews, 3rd series. Abingdon: Radcliffe Medical Press Ltd, (in press.) http://hcna.radcliffe‐oxford.com/bemgframe.htm
- 9.Cooper R S, Kaufman J S, Ward R. Race and genomics. N Engl J Med 20033481166–1170. [DOI] [PubMed] [Google Scholar]
- 10.Chaturvedi N. Ethnic differences in cardiovascular disease. Heart 200389681–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McKeigue P M, Shah B, Marmot M G. Relation of central obesity and insulin resistance with high diabetes prevalence and cardiovascular risk in South Asians. Lancet 1991337382–386. [DOI] [PubMed] [Google Scholar]
- 12.Wild S, McKeigue P. Cross sectional analysis of mortality by country of birth in England and Wales, 1970–92. BMJ 1997314705–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bhopal R, Unwin N, White M.et al Heterogeneity of coronary heart disease risk factors in Indian, Pakistani, Bangladeshi, and European origin populations: cross sectional study. BMJ 1999319215–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.D'Agostino R B Sr, Grundy S, Sullivan L M.et al Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA 2001286180–187. [DOI] [PubMed] [Google Scholar]
- 15.Erans B, Primatesta P.Health Survey for England 1998: cardiovascular disease. London: The Stationery Office, 1999
- 16.Anon Joint National Surveys Unit. Health Survey for England: the health of minority ethnic groups '99. Report no 1. London: Department of Health, 1999
- 17.Cappuccio F P, Cook D G, Atkinson R W.et al The Wandsworth Heart and Stroke Study: a population‐based survey of cardiovascular risk factors in different ethnic groups. Methods and baseline findings. Nutr Metab Cardiovasc Dis 19988371–385. [Google Scholar]
- 18.Lawlor D A, Bedford C, Taylor M.et al Geographical variation in cardiovascular disease, risk factors, and their control in older women: British Women's Heart and Health Study. J Epidemiol Community Health 200357134–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anon Caerphilly and Speedwell collaborative heart disease studies. The Caerphilly and Speedwell Collaborative Group. J Epidemiol Community Health 198438259–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shaper A G, Pocock S J, Walker M.et al Risk factors for ischaemic heart disease: the prospective phase of the British Regional Heart Study. J Epidemiol Community Health 198539197–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Anon Diverse Populations Collaborative Group. Prediction of mortality from coronary heart disease among diverse populations: is there a common predictive function, Heart 200288222–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cappuccio F P, Oakeshott P, Strazzullo P.et al Application of Framingham risk estimates to ethnic minorities in United Kingdom and implications for primary prevention of heart disease in general practice: cross sectional population based study. BMJ 20023251271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Agyemang C, Bhopal R. Is the blood pressure of people from African origin adults in the UK higher or lower than that in European origin white people? A review of cross‐sectional data. J Hum Hypertens 200317523–534. [DOI] [PubMed] [Google Scholar]
- 24.Agyemang C, Bhopal R S. Is the blood pressure of South Asian adults in the UK higher or lower than that in European white adults? A review of cross‐sectional data. J Hum Hypertens 200216739–751. [DOI] [PubMed] [Google Scholar]
- 25.De Backer G, Ambrosioni E, Borch‐Johnsen K.et al European guidelines on cardiovascular disease prevention in clinical practice. Third Joint Task Force of European and Other Societies on Cardiovascular Disease Prevention in Clinical Practice. Eur Heart J 2003241601–1610. [DOI] [PubMed] [Google Scholar]
- 26.McGinn T G, Guyatt G H, Wyer P C.et al Users' guides to the medical literature: XXII: how to use articles about clinical decision rules. Evidence‐Based Medicine Working Group. JAMA 200028479–84. [DOI] [PubMed] [Google Scholar]
- 27.Yusuf S, Hawken S, Ounpuu S.et al Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case‐control study. Lancet 2004364937–952. [DOI] [PubMed] [Google Scholar]
- 28.Quirke T P, Gill P S, Mant J W.et al The applicability of the Framingham coronary heart disease prediction function to black and minority ethnic groups in the UK. Heart 200389785–786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bhopal R, Fischbacher C, Vartiainen E.et al Predicted and observed cardiovascular disease in South Asians: application of FINRISK, Framingham and SCORE models to Newcastle Heart Project data. J Public Health (Oxf) 20052793–100. [DOI] [PubMed] [Google Scholar]
- 30.Aarabi M, Jackson P R. Predicting coronary risk in UK South Asians: an adjustment method for Framingham‐based tools. Eur J Cardiovasc Prev Rehabil 20051246–51. [PubMed] [Google Scholar]
- 31.Gill P S, Johnson M. Ethnic monitoring and equity: collecting data is just the beginning. BMJ 1995310890. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.