Abstract
Objective
To analyse short‐ and long‐term outcomes and prognostic factors in a large population‐based cohort of unselected patients with a first emergency admission for suspected acute coronary syndrome between 1990 and 2000 in Scotland.
Methods
All first emergency admissions for acute myocardial infarction (AMI) and all first emergency admissions for angina (the proxy for unstable angina) between 1990 and 2000 in Scotland (population 5.1 million) were identified. Survival to five years was examined by Cox multivariate modelling to examine the independent prognostic effects of diagnosis, age, sex, year of admission, socioeconomic deprivation and co‐morbidity.
Results
In Scotland between 1990 and 2000, 133 429 individual patients had a first emergency admission for suspected acute coronary syndrome: 96 026 with AMI and 37 403 with angina. After exclusion of deaths within 30 days, crude five‐year case fatality was similarly poor for patients with angina and those with AMI (23.9% v 21.6% in men and 23.5% v 26.0% in women). The longer‐term risk of a subsequent fatal or non‐fatal event in the five years after first hospital admission was high: 54% in men after AMI (53% in women) and 56% after angina (49% in women). Event rates increased threefold with increasing age and 20–60% with different co‐morbidities, but were 11–34% lower in women.
Conclusions
Longer‐term case fatality was similarly high in patients with angina and in survivors of AMI, about 5% a year. Furthermore, half the patients experienced a fatal or non‐fatal event within five years. These data may strengthen the case for aggressive secondary prevention in all patients presenting with acute coronary syndrome.
Every year, hospitals admit large numbers of emergency patients with suspected acute coronary syndromes: about one million in the UK and two million in the USA.1,2,3,4 This massive health service burden is a high priority.5 By time of discharge, most patients with acute coronary syndrome have a clear diagnosis of acute myocardial infarction (AMI) or unstable angina. However, the subsequent management plan is crucially dependent on a sound assessment of the patient's prognosis.4,5,6
A few small population‐based surveys in Australia, Iceland and the United Kingdom have suggested that, compared with survival after myocardial infarction, long‐term survival of middle‐aged men was apparently much better for angina, whether defined as ECG abnormalities or “Rose‐positive angina” on a Rose angina questionnaire with a normal ECG.7,8,9,10 However, none specifically examined unstable angina. Although long‐term survival after AMI has been extensively studied,11 much less is known about prognosis after emergency admission for unstable angina. The few data available are sparse and conflicting; different studies have reported one‐year case fatalities ranging from 1%12 to 19%,13 with fatal plus non‐fatal event rates up to 30%.14 Furthermore, most analyses describe relatively small numbers of selected patients in disease registers or randomised trials.12,13,14 In Canada, however, Chang et al15 recently analysed a large administrative database; they reported a five‐year case‐fatality rate of 19.5% in men and 21.6% in women after unstable angina, compared with 26.8% and 38.8%, respectively, after AMI. Longer‐term prognosis also reflected associated conditions including age, ventricular function and co‐morbidity.15
Cardiology has seen a therapeutic revolution since the 1980s. In addition to coronary artery bypass graft (CABG) surgery and angioplasty, a growing armamentarium of effective medical treatments now include thrombolysis, aspirin, β blockers, platelet glycoprotein antagonists and statins.4,5,6,16,17 But has this evidence‐based treatment actually benefited ordinary patients in the general population?14,15 Despite the increasingly widespread use of these treatments, there are almost no recent UK data describing survival of unselected patients in a population context. This highlights the practical difficulties of long‐term follow up in large unselected patient cohorts. However, such studies are now increasingly facilitated by the record linkage achieved in Britain and elsewhere.11,18,19,20 The Scottish Record Linkage System now includes over one million individual patients presenting with suspected coronary heart disease from 1981 onwards. Linkage to subsequent admissions and death records permits examination of fatal and non‐fatal events in specific patient groups over a prolonged period. Coding is essentially complete and accuracy exceeds 90%.11,18
We were thus recently able to analyse hospitalisation trends between 1990 and 2000. While first admissions for AMI fell by 30%, admissions for angina and chest pain more than doubled.22 In this present study, we have analysed short‐ and long‐term outcome and prognostic factors in this large population‐based cohort of unselected patients with a first emergency admission for suspected acute coronary syndrome between 1990 and 2000 in Scotland.
METHODS
Definitions
When using the Scottish Record Linkage System,7,16,19 we identified all “first” emergency hospitalisations with a “principal” discharge diagnosis (coded in the first position) of AMI (International classification of diseases, 9th revision (ICD‐9) 410 (acute AMI) or corresponding ICD‐10 codes I21 or I22) or “hospitalised angina” (ICD‐9 411 (other acute or subacute forms of ischaemic heart disease) or 413 (angina pectoris), or corresponding ICD‐10 codes I20 or I24.9) in Scotland between 1 January 1990 and 31 December 2000. This specification of all first emergency admissions for angina served as our crude proxy for unstable angina. We defined a first event as no prior hospitalisation with coronary heart disease of chest pain (ICD‐9 410–414 or 786.5, and ICD‐10 I20–25 or R07) in the previous 10 years.
Co‐morbidity was defined as any concomitant diagnosis or as any principle diagnosis in a prior admission within five years of the index admission, categorised as diabetes (ICD‐9 code 250); respiratory disease (480–496); cancer (140–208); cerebrovascular disease (430–438); peripheral vascular disease (440–443); essential hypertension (401); renal disease (463); or atrial fibrillation (427.3). (ICD‐10 codes E10–E14, J10–J18, J 40–J47, C00–C99, I60–I69, G45, I70–I78, I10–I13, N17–N19 and I48, respectively). All 32 acute care hospitals in Scotland were included in the analysis, of which eight were university hospitals and six had catheterisation facilities.
We used postcode sectors to allocate Carstairs deprivation categories on the basis of four variables from the 1991 census, namely male unemployment, overcrowding, social class and car ownership.
Survival analyses
All cases were followed to 31 December 2001, a minimum follow up of one year. Flagging of subsequent admissions and deaths provided “time to event”. Primary cause of death was categorised by ICD code.
Crude case fatality was calculated for follow‐up periods from 30 days to five years by using the actuarial life table method. This takes account of different lengths of follow up. Mortality up to one month was first analysed. We used a logistic regression model to quantify the independent effects on survival of age, sex, socioeconomic deprivation, year of admission and co‐morbidity (respiratory disease, diabetes, cancer, cerebrovascular disease, peripheral arterial disease, hypertension, heart failure, atrial fibrillation and renal failure). Men and women were considered separately in the models because sex was a significant predictor of outcome and because of an interaction previously seen between age and sex in short‐term outcome after an AMI.20 All variables were entered simultaneously into the models. Each model was subject to the Hosmer–Lemeshow goodness‐of‐fit test and all were non‐significant. To examine the independent effect of these factors on longer‐term survival, all variables from patients surviving ⩾ 30 days were entered simultaneously into Cox proportional hazard models. The assumption of constant proportional hazard was met for these models. For each variable entered into a model, the lowest class was set at unity.
Non‐fatal events
After the first, index admission, all subsequent admissions for non‐fatal events were identified. These were for non‐fatal AMI, stroke, heart failure, angina, angioplasty and CABG surgery. Age‐ and sex‐specific event rates were calculated for patients with an index AMI admission or angina admission. Cox proportional hazard models were then used to adjust for the effects of age, sex, year of admission, deprivation and co‐morbidity on the risk of each subsequent non‐fatal event in the two groups. All variables were entered simultaneously. The assumption of constant hazard was met for these models. Significance was accepted at p < 0.05. All analyses were undertaken with SPSS (V.11.5; SPSS Inc, Chicago, Illinois, USA).
RESULTS
Between 1990 and 2000, 133 429 individual patients had a first emergency admission for suspected acute coronary syndrome: 96 026 with AMI (72%) and 37 403 with angina (28%). This paper considers only the patients with AMI or angina.
Patients with angina were slightly younger than those with AMI, the median age of men being 64 versus 65 years, respectively (and of women, 69 v 73 years, respectively) (table 1).
Table 1 Baseline characteristics of patients with a first emergency admission for acute myocardial infarction (n = 96 026) or angina (n = 37 403), 1990–2000.
| Acute myocardial infarction | Angina | |||
|---|---|---|---|---|
| Men | Women | Men | Women | |
| Total 1990–2000 | 55 999 (58%) | 40 027 (42%) | 18 880 (49%) | 18 523 (51%) |
| Mean age (years) (median) | 65 (65) | 72 (73) | 64 (64) | 68 (69) |
| Age group (years) | ||||
| <55 | 12 332 (22%) | 3 121 (8%) | 4 550 (24%) | 3 026 (16%) |
| 55–64 | 14 530 (26%) | 6 476 (16%) | 5 175 (27%) | 4 101 (22%) |
| 65–74 | 16 493 (30%) | 11 992 (30%) | 5 366 (28%) | 5 318 (29%) |
| 75–84 | 10 332 (19%) | 12 781 (32%) | 3 172 (17%) | 4 596 (25%) |
| ⩾85 | 2 312 (4%) | 5 657 (14%) | 617 (3%) | 1 482 (8%) |
| Deprivation categories | ||||
| I (most affluent) | 9 517 (17%) | 6 529 (16%) | 2 852 (15%) | 2 632 (14%) |
| II | 11 084 (20%) | 7 670 (19%) | 3 471 (18%) | 3 298 (18%) |
| III | 11 028 (20%) | 7 955 (20%) | 3 690 (20%) | 3 658 (20%) |
| IV | 11 148 (20%) | 8 288 (21%) | 3 901 (21%) | 4 008 (22%) |
| V (most deprived) | 11 405 (20%) | 8 743 (22%) | 4 202 (22%) | 4 483 (24%) |
| Prior admission and co‐morbidities | ||||
| Diabetes | 4 112 (7%) | 3 537 (9%) | 1 516 (8%) | 1 462 (8%) |
| Malignancy | 2 660 (5%) | 2 229 (6%) | 1 210 (6%) | 1 180 (6%) |
| Respiratory disease | 4 954 (9%) | 3 872 (10%) | 1 895 (10%) | 1 823 (10%) |
| CVD | 3 225 (6%) | 2 840 (7%) | 1 161 (6%) | 907 (5%) |
| PVD | 3 677 (7%) | 2 487 (6%) | 1 466 (8%) | 1 085 (6%) |
| Hypertension | 4 687 (8%) | 4 336 (11%) | 2 384 (13%) | 2 989 (16%) |
| Atrial fibrillation | 2 946 (5%) | 2 708 (7%) | 1 157 (6%) | 1 323 (7%) |
| Heart failure | 7 500 (13%) | 7 297 (18%) | 1 305 (7%) | 1 575 (9%) |
| Renal failure | 1 274 (2%) | 1 241 (3%) | 339 (2%) | 316 (2%) |
CVD, cardiovascular disease; PVD, peripheral vascular disease.
Cause of death
Within five years of their first admission with AMI, 39 449 (41.1%) patients died. The principal causes of death were AMI (37.8%), other coronary disease (2.7%), other cardiovascular disease (40.6%), cancer (13.6%) and all other causes (5.3%).
The proportions were similar in the 8153 (21.8%) patients who died within five years of their first emergency admission with angina: AMI (28.4%), other coronary heart disease (4.3%), other cardiovascular disease (30.9%), cancer (17.7%) and all other causes (18.7%).
Univariate analyses
Short‐term case fatality
Crude short‐term case fatality within one month was high in patients with AMI (15.7% in men and 25.7% in women) but low for emergency admissions with angina (2.0% in men and 1.8% in women).
Longer‐term case fatality
After exclusion of deaths within 30 days, longer‐term crude case fatality at one, five and 10 years in men with angina was 6.5%, 23.9% and 39.8%, respectively (6.4%, 23.5% and 41.5% in women). This was very similar to the 6.4%, 21.6% and 36.0%, respectively, seen in men after a first admission for AMI (and 8.9%, 26.0% and 40.6%, respectively, in women). Age‐specific case‐fatality rates were likewise very similar in patients after AMI or angina.
Death rates in AMI and angina groups compared with the general population
The five‐year case‐fatality rate in men was 25.8% for angina and 37.3% for AMI. The five‐year mortality for a 64‐year‐old man in Scotland (mean age of angina group) was only 15.3%. Likewise, in women the five‐year mortality in the general population was lower (13.2% in a 68‐year‐old and 17.9% in a 72‐year‐old) than that of patients with either angina (25.2%) or AMI (51.7%).
Multivariate analyses
Short‐term case fatality: age, co‐morbidity and sex effects
After adjustment for other factors by logistic regression, short‐term case fatality in both patient groups roughly doubled for each decade of increasing age and increased by up to twofold, with a wide range of co‐morbidities including cancer, respiratory disease, renal disease and peripheral vascular disease (table 2).
Table 2 Factors influencing short‐term and long‐term case fatality in emergency admissions of patients with AMI or angina: multivariate analyses of risk of death*.
| Short‐term case fatality | Long‐term case fatality | ||||
|---|---|---|---|---|---|
| AMI | Angina | AMI | Angina | ||
| Sex | Men | 1.00 | 1.00 | 1.00 | 1.00 |
| Women | 1.22 | 0.71 | 0.93 | 0.71 | |
| 95% CI | 1.18 to 1.27 | 0.60 to 0.82 | 0.90 to 0.96 | 0.67 to 0.76 | |
| Age (years) | <55 | 1.00 | 1.00 | 1.00 | 1.00 |
| 55–64 | 2.31 | 2.52 | 2.01 | 2.48 | |
| 95% CI | 2.10 to 2.55 | 1.63 to 3.88 | 1.85 to 2.18 | 2.13 to 2.88 | |
| 65–74 | 5.08 | 4.25 | 3.89 | 5.07 | |
| 95% CI | 4.64 to 5.55 | 2.82 to 6.39 | 3.61 to 4.20 | 4.40 to 5.83 | |
| 75–84 | 9.79 | 9.77 | 7. 29 | 10.19 | |
| 95% CI | 8.95 to 10.70 | 6.54 to 14.58 | 6.76 to 7.87 | 8.86 to 11.73 | |
| ⩾85 | 15.86 | 13.16 | 12.69 | 17.02 | |
| 95% CI | 14.39 to 17.48 | 8.52 to 20.33 | 11.66 to 13.82 | 14.54 to 19.92 | |
| Deprivation | I (most affluent) | 1.00 | 1.00 | 1.00 | 1.00 |
| II | 1.11 | 1.08 | 1.07 | 0.99 | |
| 95% CI | 1.05 to 1.17 | 0.85 to 1.38 | 1.02 to 1.13 | 0.89 to 1.09 | |
| III | 1.11 | 0.91 | 1.08 | 1.05 | |
| 95% CI | 1.05 to 1.17 | 0.71 to 1.17 | 1.03 to 1.14 | 0.96 to 1.16 | |
| IV | 1.11 | 1.00 | 1.13 | 1.06 | |
| 95% CI | 1.05 to 1.17 | 0.78 to 1.28 | 1.07 to 1.19 | 0.97 to 1.17 | |
| V (most deprived) | 1.09 | 1.00 | 1.22 | 1.14 | |
| 95% CI | 1.03 to 1.15 | 0.78 to 1.28 | 1.16 to 1.29 | 1.04 to 1.25 | |
| Co‐morbidity | Diabetes | 1.17 | 1.24 | 1.53 | 1.59 |
| 95% CI | 1.10 to 1.24 | 0.97 to 1.59 | 1.45 to 1.61 | 1.44 to 1.75 | |
| Cancer | 1.67 | 1.50 | 1.79 | 1.70 | |
| 95% CI | 1.56 to 1.78 | 1.18 to 1.90 | 1.68 to 1.90 | 1.55 to 1.87 | |
| Respiratory disease | 1.28 | 1.06 | 1.41 | 1.41 | |
| 95% CI | 1.21 to 1.35 | 0.85 to 1.33 | 1.34 to 1.48 | 1.29 to 1.53 | |
| CVD | 1.72 | 1.69 | 1.72 | 1.61 | |
| 95% CI | 1.62 to 1.82 | 1.33 to 2.16 | 1.63 to 1.82 | 1.46 to 1.78 | |
| PVD | 1.25 | 1.26 | 1.43 | 1.46 | |
| 95% CI | 1.18 to 1.34 | 0.99 to 1.60 | 1.35 to 1.51 | 1.33 to 1.60 | |
| Hypertension | 0.74 | 0.69 | 1.02 | 0.92 | |
| 95% CI | 0.69 to 0.78 | 0.54 to 0.88 | 0.96 to 1.08 | 0.84 to 1.01 | |
| Heart failure | 1.26 | 1.95 | 1.83 | 1.75 | |
| 95% CI | 1.20 to 1.31 | 1.60 to 2.37 | 1.76 to 1.90 | 1.61 to 1.90 | |
| Atrial fibrillation | 0.73 | 0.79 | 1.28 | 1.19 | |
| 95% CI | 0.68 to 0.78 | 0.61 to 1.03 | 1.21 to 1.35 | 1.08 to 1.31 | |
| Renal disease | 2.80 | 2.19 | 1.87 | 2.35 | |
| 95% CI | 2.56 to 3.05 | 1.56 to 3.07 | 1.70 to 2.06 | 1.99 to 2.76 | |
*All risk values reported come from multivariate analyses of logistic regression models. The values are thus independent, being adjusted for all other variables.
AMI, acute myocardial infarction; CVD, cardiovascular disease; PVD, peripheral vascular disease.
Adjusted short‐term case fatality after AMI was 22% higher in women than in men (95% CI 18% to 27%) but 29% (95% CI 18% to 40%) lower after angina (table 2).
Longer‐term case fatality: age, co‐morbidity and sex effects
Adjusted case fatality over five and 10 years also doubled for each decade of increasing age and increased almost twofold, with a wide range of co‐morbidities (table 2 shows five‐year data).
Compared with men, in women adjusted case fatality was 29% (95% CI 24% to 33%) lower after angina but only 7% (95% CI 4% to 10%) lower after AMI (table 2).
Socioeconomic effects
A modest 9% adverse socioeconomic gradient was seen in short‐term case fatality after AMI but not angina (table 2). This gradient increased over the longer term to a 22% (95% CI 16% to 29%) excess case fatality in the most deprived quintile compared with the most affluent after AMI and a 14% (95% CI 4% to 25%) excess in patients with angina (table 2).
Comparison of survival after AMI and angina
After adjustment for other factors, short‐term case fatality in patients with angina was just 8% of that seen in patients with AMI (table 3). Furthermore, after exclusion of deaths in the first month, longer‐term case fatality in male patients with angina was consistently 92% of that in patients with AMI. In women, however, longer‐term case fatality in patients with angina was lower, just 72–76% of that in patients with AMI (table 3).
Table 3 Adjusted short‐term and longer‐term case‐fatality rates in patients with a first emergency admission for angina compared with a first admission for AMI, 1990–2000: logistic regression and Cox multivariate analysis*.
| Men | Women | All | ||||
|---|---|---|---|---|---|---|
| Risk of death | 95% CI | Risk of death | 95% CI | Risk of death | 95% CI | |
| Case fatality at 30 days (logistic regression) | ||||||
| AMI | 1.00 | 1.00 | 1.00 | |||
| Angina | 0.11 | 0.10 to 0.12 | 0.06 | 0.05 to 0.07 | 0.08 | 0.07 to 0.09 |
| Case fatality from 30 days to 5 years (Cox model) | ||||||
| AMI | 1.00 | 1.00 | 1.00 | |||
| Angina | 0.92 | 0.88 to 0.97 | 0.72 | 0.69 to 0.75 | 0.81 | 0.79 to 0.84 |
| Case fatality from 30 days to 10 years (Cox model) | ||||||
| AMI | 1.00 | 1.00 | 1.00 | |||
| Angina | 0.92 | 0.86 to 0.98 | 0.76 | 0.70 to 0.81 | 0.83 | 0.79 to 0.88 |
*All the hazard values reported come from multivariate analyses of logistic regression and Cox models. The values are thus independent, being adjusted for all other variables.
AMI, acute myocardial infarction.
Subsequent non‐fatal events
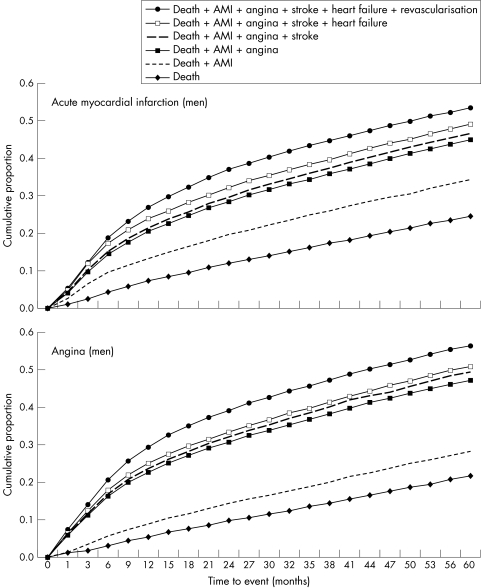
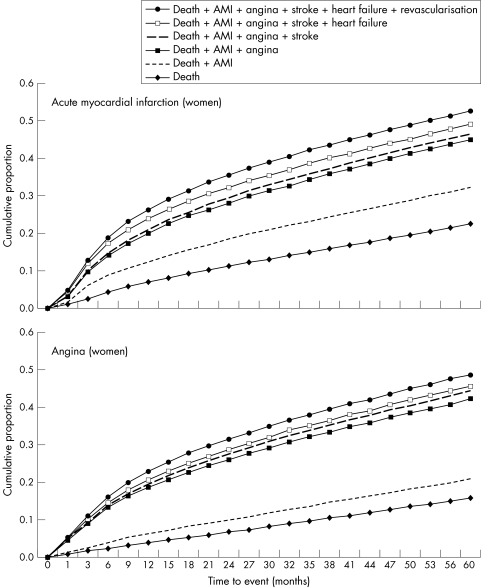
Within five years of the first admission, almost half the men experienced a fatal or non‐fatal event: death, AMI, angina admission, stroke, heart failure, angioplasty or CABG surgery. After AMI, age‐adjusted event rates in women were as high as in men (52.6% v 53.6%) and almost as high after angina (48.8% v 56.3%) (figs 1 and 2).
Figure 1 Probability of a fatal or non‐fatal event in men after a first admission for acute coronary syndrome, Scotland, 1990–2000 (adjusted for age, excluding deaths up to 30 days).
Figure 2 Probability of a fatal or non‐fatal event in women after a first admission for acute coronary syndrome, Scotland, 1990–2000 (adjusted for age, excluding deaths up to 30 days).
After AMI
Within five years of the first admission, 15 406 (16.1%) of the surviving men experienced one or more non‐fatal cardiovascular events. These comprised 9.9% AMI, 1.9% stroke, 3.2% heart failure, 7.2% CABG and 3.1% angioplasty (and in women: 6.3%, 4.1%, 2.7%, 3.0% and 1.9%, respectively). These events were not mutually exclusive; thus, some patients experienced multiple events.
After a first emergency angina admission
Within five years of the first admission, 6715 (18.0%) of the surviving men experienced a non‐fatal cardiovascular event: 6.6% AMI, 4.7% stroke, 1.7% heart failure, 10.1% CABG and 5.1% angioplasty (and in women 5.1%, 5.1%, 1.8%, 4.2% and 3.0%, respectively).
Subsequent revascularisation
Revascularisation within five years was about twice as likely in men as in women (3.6% v 2.2% for CABG and 7.9% v 3.4% for angioplasty).
Revascularisation rates also showed a substantial negative age gradient and a consistent sex inequality. After an AMI, CABG surgery rates within five years decreased from 11.5% in men aged under 55 years to 0.8% in those aged 75–84 years (8.5% v 0.2% in women); corresponding rates after angina decreased from 10.5% to 2.6% in men (from 3.5% to 0.9% in women).
A similar age gradient was seen for angioplasty within five years after AMI, decreasing from 7.0% in men aged less than 55 years to 0.5% in men aged 75–84 years (8.1% to 0.3%, respectively, in women). Corresponding rates after angina decreased from 7.7% to 1.3% in men (from 5.0% to 0.6% in women).
Subsequent fatal and non‐fatal events: multivariate analyses
After adjustment for other factors, fatal and non‐fatal event rates were greatly increased by age (threefold after AMI and fourfold after angina, aged < 55 v aged >85 years) (table 4). Rates were also increased up to 60% by different co‐morbidities. However, socioeconomic deprivation had an adverse effect of only 8% after angina and 15% after AMI (table 4).
Table 4 Factors influencing fatal plus non‐fatal event rates from 30 days to five years following a first emergency admission for AMI or angina (multivariate analyses, excludes deaths at 30 days*).
| AMI | Angina | ||||
|---|---|---|---|---|---|
| Hazard | 95% CI | Hazard | 95% CI | ||
| Sex | Men | 1.00 | 1.00 | ||
| Women | 0.89 | 0.87 to 0.92 | 0.66 | 0.63 to 0.69 | |
| Age (years) | <55 | 1.00 | 1.00 | ||
| 55–64 | 1.13 | 1.08 to 1.18 | 1.59 | 1.47 to 1.72 | |
| 65–74 | 1.37 | 1.31 to 1.43 | 1.99 | 1.85 to 2.15 | |
| 75–84 | 2.00 | 1.91 to 2.09 | 2.74 | 2.54 to 2.96 | |
| ⩾85 | 3.03 | 2.86 to 3.21 | 4.15 | 3.74 to 4.60 | |
| Deprivation | I (most affluent) | 1.00 | 1.00 | ||
| II | 1.04 | 0.99 to 1.08 | 1.04 | 0.96 to 1.12 | |
| III | 1.04 | 1.00 to 1.09 | 1.05 | 0.98 to 1.14 | |
| IV | 1.06 | 1.01 to 1.10 | 1.02 | 0.95 to 1.10 | |
| V (most deprived) | 1.15 | 1.10 to 1.20 | 1.08 | 1.00 to 1.16 | |
| Co‐morbidity | Diabetes | 1.32 | 1.26 to 1.38 | 1.41 | 1.30 to 1.53 |
| Cancer | 1.48 | 1.39 to 1.56 | 1.35 | 1.24 to 1.47 | |
| Respiratory disease | 1.27 | 1.21 to 1.32 | 1.20 | 1.12 to 1.29 | |
| CVD | 1.52 | 1.45 to 1.60 | 1.44 | 1.32 to 1.57 | |
| PVD | 1.27 | 1.21 to 1.34 | 1.21 | 1.12 to 1.31 | |
| Hypertension | 1.07 | 1.02 to 1.12 | 1.01 | 0.94 to 1.08 | |
| Heart failure | 1.51 | 1.46 to 1.57 | 1.42 | 1.32 to 1.53 | |
| Atrial fibrillation | 1.22 | 1.16 to 1.29 | 1.04 | 0.95 to 1.13 | |
| Renal disease | 1.62 | 1.48 to 1.77 | 1.68 | 1.44 to 1.97 | |
*All the hazard values reported come from multivariate analyses of logistic regression and Cox models. The values are thus independent, being adjusted for all other variables.
AMI, acute myocardial infarction; CVD, cardiovascular disease; PVD, peripheral vascular disease.
After adjustment for age and other factors, risk of fatal plus non‐fatal event rates was 34% (95% CI 31% to 37%) lower in women than in men after a first admission for angina but only 11% (95% CI 8% to 13%) lower after an AMI admission (table 4).
DISCUSSION
This paper describes clinical outcomes in a large unselected cohort of patients after a first emergency admission with suspected acute coronary syndrome. Short‐term case fatality after a diagnosis of AMI was high, as elsewhere.5,10,11,15 However, short‐term case fatality was only 2% for emergency admissions with angina (our proxy for unstable angina when using this database). These data therefore support the current clinical priority of rapidly triaging such patients.4,5,16,17
After exclusion of initial deaths, longer‐term case fatality after a first emergency admission was almost as high for angina as for AMI, about 4–5% a year. These novel and important findings suggest that long‐term risk is substantial in all emergency admissions with coronary heart disease, not just AMI survivors. Non‐fatal event rates were also high. We suggest that these findings perhaps highlight the importance of secondary preventative strategies for all patients with acute coronary syndromes.
Short‐term and long‐term case fatality in all groups with suspected acute coronary syndromes roughly doubled with each increasing decade of age and was further increased by co‐morbidity. This is consistent with earlier studies14,15,21 and endorses the recommended prioritisation of older and sicker patients.14,16,17
As in the smaller Canadian series,15 deprivation consistently increased longer‐term case fatality in all patient groups with suspected acute coronary syndromes, rising by about 20% from the most affluent to the most deprived quintiles. Although lower use of secondary prevention drugs may partly explain this gradient, other factors may also be important, such as diet and smoking.15,21,22 These modest deprivation gradients contrast with the consistently reported threefold variations in disease incidence.22
Risk of subsequent non‐fatal events
Within five years of their first admission, about one fifth of the surviving patients experienced a non‐fatal cardiovascular event (principally AMI, but also stroke, angina, heart failure or revascularisation). This is consistent with the 10–15% rates reported after just 12 months for trial and registry patients.12,14,23 Interestingly, while a further, non‐fatal myocardial infarction was more common in myocardial infarction survivors than in angina survivors, the opposite was seen for stroke. This merits further research.
After adjustment for other factors, cardiovascular event rates increased threefold with age, by up to 60% with different co‐morbidities and by up to 15% with greater deprivation. We suggest that this may strengthen the case for equally aggressive secondary prevention, irrespective of age and class.4,5,6,22
Inequalities in revascularisation after a first admission for acute coronary syndrome
Revascularisation rates were generally low, much as may be expected in the 1990s. Revascularisation was twice as likely in men as in women of the same age. Clinical justification appears difficult. Revascularisation rates also showed a substantial age gradient. After an AMI, CABG surgery within five years was about 15 times less likely in men aged 75–84 years than in men aged under 55 years. Even larger age gradients were seen in women. This therefore provides yet more evidence of the substantial age and sex biases reported in North America, Europe and elsewhere.15,24,25
The probability of CABG surgery within five years of AMI was about twice as high as angioplasty between 1990 and 2000. However, this ratio is now close to unity.2,3,26
Our study captured essentially all hospital and fatal events in the Scottish population of 5.1 million and is thus cautiously generalisable to similar populations elsewhere. However, the study has some potential limitations. While statistics on routine death certification of coronary heart disease in Britain appear reliable up to the age of 65, they may be overestimated in older groups by up to 20%.27 However, any such inflation is unlikely to have changed substantially between 1990 and 2000. The definition of a first admission, “no previous admission recorded in 1981 or thereafter”, may have included some long‐term survivors with a prior admission, albeit less than 5%.11,22 Our proxy for unstable angina, “emergency admission with angina”, may have captured milder cases of angina in our analysis. This may have resulted in an underestimation of the case fatality of patients admitted with angina. However, this may have been balanced by some overestimation of case fatality because these data come from the pre‐troponin era and probably include some patients with actual myocardial infarction. There were no data on severity of cardiovascular disease, so it was not possible to take this into account when looking at the potential effects of age, sex and socioeconomic status on variations in rates for deaths, events or revascularisation. Furthermore, some misclassification is possible—for example, some patients with angina dying in hospital may have been recoded as having myocardial infarction. However, our findings are generally consistent with smaller series from clinical disease registers.12,13,14,15 Furthermore, coding is essentially complete and accuracy exceeds 90%.11,18 We were able to identify only those patients with non‐fatal events actually admitted to hospital but this probably included the great majority of significant events. If the true total was even higher, this further emphasises the substantial event rates in these patients.
In conclusion, after a first emergency admission for acute coronary syndrome, the long‐term prognosis is almost as poor for angina as for AMI. Within five years, half the patients may expect a fatal or non‐fatal event. These data may strengthen the case for aggressive secondary prevention for all patients admitted with acute coronary syndrome.
ACKNOWLEDGEMENTS
We thank the British Heart Foundation for funding Kate MacIntyre and Niamh Murphy, and the Registrar General for Scotland for providing mortality data. We are grateful to colleagues in Edinburgh and Glasgow for advice and support, particularly Jill Pell for comments on an early draft.
Abbreviations
AMI - acute myocardial infarction
CABG - coronary artery bypass graft
ICD - International classification of diseases
Footnotes
Competing interests: None declared.
NM and KM were funded by the British Heart Foundation. SS was supported by the Australian National Heart Foundation.
Author contributions: SC developed and co‐ordinated this study, contributed to the analyses and interpretation, and drafted and finalised the report. KM and NM analysed the data, and contributed to the interpretation and report drafting. SS, JC and JM each contributed to the study design, analyses, interpretation and report drafting. SF and AF extracted the data and contributed to the design, analyses and writing. JB and AR contributed to the data analysis, design and drafting. All investigators contributed to the final paper.
References
- 1.Capewell S, McMurray J J V. “Chest Pain‐Please Admit”: is there an alternative? A rapid cardiological assessment service may prevent unnecessary admissions. BMJ 2000320951–952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.British Heart Foundation British Heart Foundation Statistics Website. Hospitalisations. http://www.heartstats.org/datapage.asp?id = 842 (accessed 14 Jun 2005)
- 3.Davie A P, Caesar D, Caruana L.et al Outcome from a rapid‐assessment chest pain clinic: closing Pandora's box? QJM 199891339–343. [DOI] [PubMed] [Google Scholar]
- 4.Braunwald E. Application of current guidelines to the management of unstable angina and non‐ST‐elevation myocardial infarction. Circulation 2003108(16 Suppl 1)III28–III37. [DOI] [PubMed] [Google Scholar]
- 5.Department of Health National Service Framework for Coronary Heart Disease. London: Department of Health, 2000, http://www.dh.gov.uk/PublicationsAndStatistics/Publications/PublicationsPolicyAndGuidance/PublicationsPolicyAndGuidanceArticle/fs/en?CONTENT_ID = 4105281&chk = HmsiOz (accessed 14 Jun 2005)
- 6.Scottish Intercollegiate Guidelines Network Secondary prevention of coronary heart disease following myocardial infarction. SIGN publication no 41. Edinburgh: SIGN, 2000, http://www.sign.ac.uk/guidelines/fulltext/41/index.html (accessed 14 Jun 2005)
- 7.Sigurdsson E, Sigfusson N, Agnarsson U.et al Long‐term prognosis of different forms of coronary heart disease: the Reykjavik Study. Int J Epidemiol 19952458–68. [DOI] [PubMed] [Google Scholar]
- 8.Lim L L, Kinlay S, Fisher J D.et al Can ECG changes predict the long‐term outcome in patients admitted to hospital for suspected acute myocardial infarction? Cardiology 199788460–467. [DOI] [PubMed] [Google Scholar]
- 9.Lampe F C, Morris R W, Whincup P H.et al Is the prevalence of coronary heart disease falling in British men? Heart 200186499–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rose G, McCartney P, Reid D D. Self‐administration of a questionnaire on chest pain and intermittent claudication. Br J Prev Soc Med 19773142–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Capewell S, Livingston B M, MacIntyre K.et al Trends in case‐fatality in 117 718 patients admitted with acute myocardial infarction in Scotland. Eur Heart J 2000211833–1840. [DOI] [PubMed] [Google Scholar]
- 12.Tonkin A M, Colquhoun D, Emberson J.et al Effects of pravastatin in 3260 patients with unstable angina: results from the LIPID study. Lancet 20003551871–1875. [DOI] [PubMed] [Google Scholar]
- 13.Lee H S, Cross S J, Rawles J M.et al Patients with suspected myocardial infarction who present with ST depression. Lancet 19933421204–1207. [DOI] [PubMed] [Google Scholar]
- 14.Collinson J, Flather M D, Fox K A.et al Clinical outcomes, risk stratification and practice patterns of unstable angina and myocardial infarction without ST elevation: Prospective Registry of Acute Ischaemic Syndromes in the UK (PRAIS‐UK). Eur Heart J 2000211450–1457. [DOI] [PubMed] [Google Scholar]
- 15.Chang W C, Kaul P, Westerhout C M.et al Impact of sex on long‐term mortality from acute myocardial infarction vs unstable angina. Arch Intern Med 20031632476–2484. [DOI] [PubMed] [Google Scholar]
- 16.Bertrand M E, Simoons M L, Fox K A A.et al Management of acute coronary syndromes in patients presenting without persistent ST segment elevation. Heart J 2002231809–1840. [DOI] [PubMed] [Google Scholar]
- 17.Van de Werf F, Ardissino D, Betriu A.et al Management of acute myocardial infarction in patients presenting with ST‐segment elevation. The Task Force on the Management of Acute Myocardial Infarction of the European Society of Cardiology. Eur Heart J 20032428–66. [DOI] [PubMed] [Google Scholar]
- 18.Kendrick S, Clarke J. The Scottish Record Linkage System. Health Bull 19935172–79. [PubMed] [Google Scholar]
- 19.Goldacre M J, Simmons H, Henderson J.et al Trends in episode based and person based rates of admission to hospital in the Oxford record linkage study area. BMJ 1988296583–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.MacIntyre K, Stewart S, Capewell S.et al Gender and survival: a population‐based study of 201,114 men and women following a first acute myocardial infarction. J Am Coll Cardiol 200138729–735. [DOI] [PubMed] [Google Scholar]
- 21.Murphy N F, MacIntyre K, Capewell S.et al Hospital discharge rates for suspected acute coronary syndromes between 1990 and 2000: population based analysis. BMJ 20043281413–1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Capewell S, Macintyre K, Chalmers J W.et al Age, sex and social trends in out‐of‐hospital cardiac deaths in Scotland 1986–1995: a retrospective cohort study. Lancet 20013581213–1217. [DOI] [PubMed] [Google Scholar]
- 23.Lloyd‐Jones D M, Camargo C A, Allen L A.et al Predictors of long‐term mortality after hospitalization for primary unstable angina pectoris and non‐ST‐elevation myocardial infarction. Am J Cardiol 2003921155–1159. [DOI] [PubMed] [Google Scholar]
- 24.Bowling A. Ageism in cardiology. BMJ 19993191353–1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Morris R W, Whincup P H, Papacosta O.et al Inequalities in coronary revascularisation during the 1990s: prospective study in older British men. Heart 200490(Suppl II)039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Scottish Health Statistics Coronary Heart Disease. Operations and activity. http://www.isdscotland.org/isd/info3.jsp?pContentID = 2851&p_applic = CCC&p_service = Content.show& (accessed 14 Jun 2004)
- 27.Norris R M. Fatality outside hospital from acute coronary events in three British health districts, 1994–5. United Kingdom Heart Attack Study Collaborative Group. BMJ 19983161065–1070. [PMC free article] [PubMed] [Google Scholar]