Atherosclerosis has been demonstrated in autopsy studies to have its origins in childhood.1 In the young, there is a correlation between the intensity of exposure to risk factors such as cigarette smoking, hypertension, dyslipidaemia and diabetes mellitus and the extent and severity of arterial fatty streaks or raised plaques (fig 1).
Figure 1 Fatty streaks and raised plaques are seen in childhood and correlate with the intensity of exposure to risk factors.
An important current trend that may increase the future burden of coronary heart disease (CHD) is a significant increase in the prevalence of childhood obesity.2 In obesity, many of the risk factors for CHD are clustered together. Moreover, these risk factors usually persist or track into adulthood, so that their effect on the cardiovascular system may be present and influential for several decades.
To reduce the future burden of CHD, we need to define prevention and intervention strategies that decrease the prevalence of cardiovascular risk factors in children and young adults and thereby hope to retard atherogenic processes. The purpose of this article is to review the evidence for the importance of the childhood risk factors for adult cardiovascular disease and to outline the evidence for the efficacy of primary prevention in young people.
DETECTING EARLY ARTERIAL ABNORMALITIES
Studies on the impact of risk factors in childhood and on the effect of potentially beneficial interventions have been facilitated by the development of a number of non‐invasive diagnostic techniques that can detect “atherosclerosis” at a preclinical stage (or at least the changes in arterial structure and/or function indicative of vascular damage). For example, the arterial endothelium plays a key role in atherogenesis, and clinical evaluation of the function of the endothelium is now possible through the assessment of nitric oxide‐mediated vasodilatation produced by sheer stress (flow mediated dilatation (FMD)). FMD can be measured accurately and reproducibly by ultrasound. Impaired FMD has also been demonstrated in children at high risk of future CHD.3 Measuring the velocity of the arterial pulse wave non‐invasively might also be a valuable indicator of vascular “stiffness”, and thus subsequent risk, in children.
Intima media thickness (IMT), measured by ultrasound of the carotid arteries or aorta, is a structural change in the vasculature that also appears to have value as a surrogate marker of atherosclerosis. IMT is correlated with the number of cardiovascular risk factors present and it relates to the severity and extent of coronary artery disease. IMT predicts the likelihood of cardiovascular events in asymptomatic adults and increased IMT has also been demonstrated in children with known cardiovascular risk factors.4,5 The number of risk factors present in males during late childhood and adolescence directly relates to the IMT in young adulthood, even after adjusting for contemporaneous risk factors.5
Inflammation plays an important role in the pathogenesis of atherosclerosis. C‐reactive protein (CRP) is elevated in adults with unstable angina and myocardial infarction. A moderately elevated high sensitivity CRP is also an independent risk factor for CHD in healthy adult populations. CRP is raised in children at risk of premature CHD and thus may be a useful marker in such high‐risk children. Other circulating acute‐phase reactants and soluble adhesion molecules (such as ICAM—1, for example) have been measured in adults to provide a measure of the risk of future cardiovascular events; some may prove to be useful as clinical markers in children.
CHILDHOOD OBESITY AND ATHEROSCLEROSIS
The prevalence of obesity in childhood varies between countries and also according to ethnicity and socioeconomic status. In most developed and many transitional countries the prevalence of childhood overweight and obesity is high and increasing significantly. For example, in the United States as part of the National Health and Nutrition Examination Survey (NHANES) among children aged 6–19 years in 1999 to 2002, 31.0% were at risk for overweight or obesity and 16.0% were overweight.
Obesity is associated with a number of cardiovascular risk factors such as hypertension, dyslipidaemia and diabetes mellitus. Analysis of data from the Framingham Heart Study, with a 26 year follow‐up period, indicated that increasing weight was associated with greater rates of CHD, independent of other risk factors. The effect of weight on CHD was greatest among the younger members of the cohort.6
Childhood and adolescent obesity is associated with an increased all‐cause adult mortality and case–control studies of the effect of obesity measured in adolescence on future cardiovascular mortality have also shown a positive relationship. However, an analysis of a large cohort of Aberdeen children born in the 1950s with a mean age of 4.9 years did not show an association between body mass index (BMI) and future risk of CHD. These findings may indicate that BMI in early childhood is less predictive of future risk compared with BMI in adolescence. Alternatively, absolute BMI in early childhood may not be as important a determinant of risk as the rate of weight gain over time.
The Bogalusa Heart and PDAY autopsy studies of the young have confirmed that increasing BMI and a thick panniculus adiposus (a marker of the presence of visceral fat) are associated with more extensive atherosclerosis, independent of the other standard risk factors.1 Obesity in the young is also associated with preclinical abnormalities of arterial structure and function. For example, impaired endothelial function and arterial stiffness as well as increased IMT have been demonstrated in obese children.7,8 BMI measured in childhood is significantly associated with carotid IMT, measured in adulthood.5,9
Abbreviations
ARIC: Atherosclerosis Risk In Communities
apo(a): apolipoprotein a
BMI: body mass index
CHD: coronary heart disease
CRP: C‐reactive protein
DCCT: Diabetes Control and Complications Trial
DM: diabetes mellitus
EDIC: Epidemiology of Diabetes Interventions and Complications
ETS: environmental tobacco smoke
FELIC: Fate of Early Lesions in Children
FH: familial hypercholesterolaemia
FMD: flow mediated dilatation
HDL: high density lipoprotein
IMT: intima media thickness
LBW: low birth weight
LDL: low density lipoprotein
Lp(a): lipoprotein (a)
MS: metabolic syndrome
NHANES: National Health and Nutrition Examination Survey
OSA: obstructive sleep apnoea
SSCS: side‐stream cigarette smoke
As obese children and adolescents are likely to become obese adults, any association between childhood obesity and CHD may primarily reflect adult obesity. Evidence for the importance of both childhood and adult obesity on CHD risk comes from the Bogalusa Heart study where IMT was elevated only in obese young adults who had been obese children (and not in obese children who become normal weight adults nor in thin children who become obese adults). This suggests the importance of treatment of obesity at all ages for reducing the risk of CHD.
Obesity is the most important determinant of the clustering of risk factors defined as the metabolic syndrome (MS). Other components of the MS include hyperinsulinaemia, hypertension and hyperlipidaemia. In the United States as many as 4% of all adolescents and 30–50% of overweight children may fulfil the diagnosis, depending upon the criteria used and the racial group studied. The MS in childhood tracks into adulthood and the fewer the number of risk variables of MS that are present in childhood, the lower the risk is of MS persisting into adulthood. Insulin resistance, a central component of MS, is associated with increased blood pressure, atherogenic dyslipidaemia (raised triglycerides, small low density lipoprotein (LDL) particles and low high density lipoprotein (HDL) cholesterol) and a pro‐inflammatory and pro‐thrombotic state.
Obesity may also mediate cardiovascular risk through an association with obstructive sleep apnoea (OSA). OSA in children is associated with an increased left ventricular mass index, which in adults is a strong predictor of CHD, stroke and sudden death. The long term significance of the relationship between childhood obesity, OSA and future CHD risk still needs to be explored.
The main strategies for prevention and treatment of overweight and obesity in childhood are dietary modification and increased physical activity. Detailed guidelines and goals for primary prevention and treatment have been outlined in a recent American Heart Association Scientific Statement.2 In overweight and obese children, physical activity of moderate intensity undertaken regularly reduces total body and visceral adiposity, lowers triglycerides and increases HDL values, and improves some aspects of the MS.
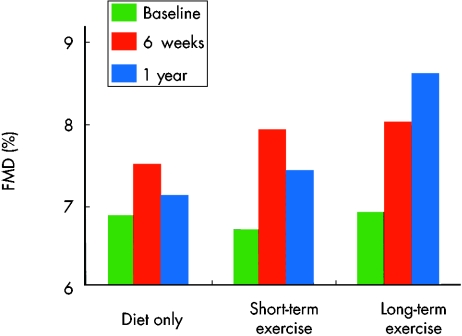
Exercise is known to have beneficial effects on endothelial function and evidence now exists for the direct benefits of diet and exercise on arterial structure and function in overweight and obese children.7 Woo et al found that in overweight and obese 9–12‐year‐olds, six weeks of dietary modification alone or diet plus a supervised structured exercise programme were both associated with increased FMD. However, the changes were significantly greater after diet plus exercise compared with diet alone. Exercise and diet continued for one year resulted in further improvement in FMD and a regression of IMT. In contrast, although some benefit continued to exist at one year, the FMD returned toward baseline in those subjects who ceased exercise. At one year, diet alone also induced a small but significant reduction in IMT (fig 2).
Figure 2 In overweight and obese children, six weeks of dietary modification plus a supervised structured exercise programme produced the maximal improvement in flow mediated dilatation (FMD). Exercise and diet continued for one year resulted in further improvement compared with those who ceased exercise.7
CIGARETTE SMOKING AND EXPOSURE TO ENVIRONMENTAL TOBACCO SMOKE
The onset of smoking is usually in adolescence (over 20% of US, UK and Australian adolescents smoke cigarettes on a daily basis) and recent studies have highlighted the importance of preventing smoking and exposure to environmental tobacco smoke (ETS) in children and adolescents. For example, in autopsy studies of the young, exposure to cigarette smoking is strongly correlated with the extent of atherosclerosis.1 In the Atherosclerosis Risk In Communities (ARIC) study, current adult smokers and past smokers had respectively a 50% and 25% increased rate of progression of carotid IMT compared with those who had never smoked.10 IMT progression was independently associated with the number of pack‐years of exposure, but after controlling for exposure the progression rates of current and past smokers did not differ. This suggests that some of the adverse effects of smoking are cumulative. Raitakari et al showed that carotid IMT in adulthood is significantly associated both with smoking in childhood and with adult smoking status.9 Smoking in the young itself is associated with an increased IMT.
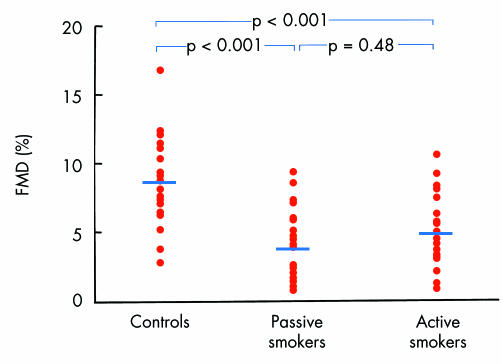
ETS, consisting of both side‐stream cigarette smoke (SSCS) from the burning cigarette and exhaled mainstream smoke, contains over 4000 chemicals. SSCS has a higher concentration of these chemicals than inhaled smoke because it is not filtered and burns at a lower temperature and hence is incompletely combusted. ETS exposure has a variety of physiological and biochemical effects in the young. For example, both active smoking and ETS exposure adversely effect endothelial function in the young, in a dose dependent way (fig 3).11 This endothelial dysfunction associated with passive smoking appears to be at least partially reversible. In the ARIC study, exposure to ETS was associated with a 20% increase in IMT progression, relative to those not exposed.10 Exposure to passive smoking results in lower HDL cholesterol in children and adolescents.
Figure 3 Both active and passive smoking impair flow mediated dilatation (FMD) in the young.11
Evidence exists for the effectiveness of motivational strategies directed at parents to reduce exposure of infants and young children to cigarette smoke. For example, in a randomised trial of motivational intervention (a 30–45 minute motivational interview session between parents of young infants and a trained health educator and four follow‐up telephone counselling calls) compared with self help, Emmons et al found that the motivational intervention strategy was superior in reducing childhood exposure to passive smoke, independent of smoking cessation.
Children should be encouraged to actively avoid ETS and to not start smoking. Adolescents in particular may be motivated by wishing to avoid the short‐term effects of smoking, such as bad breath, smell and nicotine stains on the fingers. Teenagers who have been regular smokers and who have a physical dependency may require nicotine replacement therapy in order to quit.
DYSLIPIDAEMIA
A strong positive association between total and LDL cholesterol and CHD has been established in a number of major epidemiological studies. Lower levels of HDL cholesterol are also associated with increased CHD risk. Cholesterol concentrations track over time so that those children with high LDL are likely to become adults with high LDL.
Autopsy studies of young adults have demonstrated that the extent of atherosclerosis in the aorta and coronary arteries is strongly associated with serum triglycerides and LDL and weakly negatively related to HDL.1 Even maternal hypercholesterolaemia is associated with enhanced fatty streak formation in human fetal arteries.12 The Fate of Early Lesions in Children (FELIC) study (autopsies of 156 normocholesterolaemic 1‐ to 13‐year‐olds who died of trauma or other causes) demonstrated that children whose mothers were hypercholesterolaemic in pregnancy had a greater rate of progression of atherosclerosis than children born to normocholesterolaemic mothers.12 As the placenta is impermeable to LDL particles, maternal hypercholesterolaemia does not result in fetal hypercholesterolaemia. However, animal models implicate a pathogenic role of lipid peroxidation end products, which increase in offspring in proportion to the maternal cholesterol concentrations. One effect of the lipid peroxidation end products in promoting atherosclerosis is an alteration in arterial gene expression that persists long after the fetal exposure to hypercholesterolaemia.
Whether increasing cholesterol values in the young over the “normal range” are correlated with an increased risk of future CHD remains controversial. Cholesterol concentrations in young men have been linked to overall mortality. Leeson et al found that higher childhood LDL cholesterol was associated with arterial stiffness.13 However, in a population based study of 9‐ to 11‐year‐olds, the same authors did not find an association between cholesterol concentrations and endothelial function. To clarify the risk of childhood cholesterol on future CHD, large long‐term prospective cohort studies may be required.
In the meantime, a population‐based strategy to maintain lower blood cholesterol concentrations in all children is recommended. A low fat diet has been shown to be safe and efficacious in children with hypercholesterolaemia and such a strategy would have the effect of lowering blood cholesterol in the whole population over the long term.
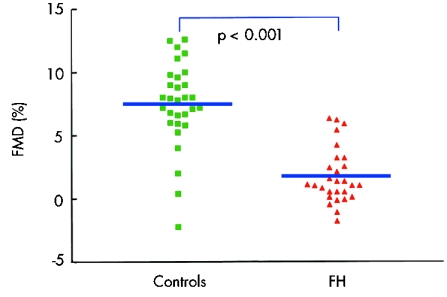
In conjunction with a population approach, dyslipidaemia should be looked for in children whose families have a history of premature CHD or hypercholesterolaemia. For example, familial hypercholesterolaemia (FH) is a relatively common genetic defect resulting from a mutation of the LDL receptor, with a prevalence of 1 in 500. The diagnosis of FH is based on family history, the presence of tissue deposits of cholesterol, and LDL values. Confirmation by DNA sequencing is available in some centres. Children with FH have impaired endothelial function, a thickened IMT and a fivefold greater rate of increase in IMT than controls (fig 4). Young adults with FH have a high risk of premature CHD.
Figure 4 Impaired flow mediated dilatation (FMD) can be demonstrated in children with familial hypercholesterolaemia (FH).3
A limited number of controlled trials of statins indicate that they are safe and effective in children over the short term (for example, de Jongh et al14). However, concerns still exist about their effect on child growth and development in the longer term. Recommended age and LDL cutoffs for the use of drug treatment of hypercholesterolaemia are therefore somewhat arbitrary. In addition to the presence of a family history of premature CHD, the rate of change of IMT may be important in risk stratification.
Lipoprotein (a) (Lp(a)) has many features in common with LDL but uniquely contains apolipoprotein a (apo(a)), a hydrophilic, carbohydrate‐rich protein covalently linked to apoB‐100. Plasma concentrations of Lp(a) are genetically determined and are only affected to a minor extent by age, sex and environmental factors. Most but not all previous studies have shown that an elevated Lp(a) is an independent risk factor for CHD. The role of Lp(a) in the onset of atherosclerosis in childhood is uncertain. Weigman et al have shown that elevated Lp(a) in children with FH predicts a kindred with the highest CHD risk.15 However, Raitakari et al demonstrated that Lp(a) concentrations were not correlated with the early functional changes of arterial endothelial and smooth muscle function or the early structural changes of IMT. Moreover, in the PDAY autopsy study, neither Lp(a) nor apo(a) size were strongly correlated with extent of atherosclerosis.
DIABETES MELLITUS
The incidence of type 1 diabetes mellitus (DM) shows a large worldwide variation (from 0.6 per 100 000 in Korea and Mexico to 35.3 per 100 000 in Finland) and is increasing in many regions. In autopsy studies of children there is a positive association between early atherosclerosis and the diabetic state; there is also a synergistic effect of high glucose and higher cholesterol. Children and young adults with type 1 DM have been shown to have impaired brachial artery FMD. The degree of impairment relates to the duration of diabetes and the LDL values. Young type 1 diabetics also have an increased aortic and carotid IMT compared with controls. Important determinants of IMT in type 1 DM may include LDL cholesterol and systolic blood pressure, or age and duration of diabetes.
The beneficial effects of intensive diabetic therapy on microvascular disease were demonstrated in the Diabetes Control and Complications Trial (DCCT). During the DCCT, intensive treatment improved the lipoprotein profile but also caused weight gain. Long term follow‐up of this cohort under the Epidemiology of Diabetes Interventions and Complications (EDIC) study has shown, in the intensively treated group, major reductions in the risk of cardiovascular events and in the rate of progression of carotid IMT, which were correlated with reduction in the HbA1c value during the DCCT.16 Progression of carotid IMT was associated with age, the EDIC baseline systolic blood pressure, smoking, the ratio of LDL to HDL cholesterol, urinary albumin excretion rate, and the mean HbA1c value during the DCCT. Within the EDIC study, those of the DCCT cohort who were adolescents at the time of recruitment have had fewer microvascular complications. In this group, the incidence of macrovascular complications has not been reported separately. However, intensive treatment in adolescents in combination with avoidance of hypertension, dyslipidaemia and smoking will almost certainly have a beneficial effect on reducing CHD risk.
In pre‐pubertal children with type 1 DM, the risk of developing microvascular disease is lower and the risk of the deleterious effects of hypoglycaemia may be higher. As a result, there is possibly less benefit of intensive treatment in younger children.
The prevalence of type 2 DM in childhood is increasing rapidly and has recently been estimated at between 2–50 per 1000 in various populations.17 Type 2 DM is associated with lower HDL and higher triglyceride values and more abundant small, dense LDL particles. A number of studies have shown a significant reduction in rates of CHD in adults with type 2 DM treated with statins or fibrates. Whether children and adolescents with type 2 DM gain a benefit from drug treatment for dyslipidaemia requires further study.
HYPERTENSION
Hypertension may begin in childhood and track into adulthood. As blood pressure is positively correlated with BMI in children, the prevalence of hypertension in childhood is likely to rise. Paradis et al have recently reported a high‐normal or elevated blood pressure in 30% of boys and 17% of girls aged 16 years. The increased carotid IMT and left ventricular hypertrophy observed in children and adolescents with essential hypertension are also correlated with BMI.
Weight loss and improved cardiovascular conditioning would thus be expected to lower blood pressure in children, although the evidence for this is limited. In adolescents weight loss decreases blood pressure, decreases the sensitivity to salt, and improves other risk factors. In adults, salt restriction will lower blood pressure and as most children in developed countries have a diet higher in salt than is required, moderation in the use of dietary salt is recommended. A diet that emphasises fruits, vegetables and low fat dairy products—the so‐called DASH diet—will reduce blood pressure in normo‐ and hypertensive adults, independent of weight loss. A prospective study on the effects of the DASH diet on blood pressure in children has not been performed; however, children in the Framingham Children's Study, initially 3–6 years of age at enrolment, who consumed more fruits and vegetables (four or more servings per day) or more dairy products (two or more servings per day) during the preschool years had smaller yearly increments in systolic blood pressure throughout childhood and a lower systolic blood pressure in early adolescence.18
A recent meta‐analysis of 12 randomised trials with a total of 1266 children and adolescents concluded that physical activity leads to a small but significant reduction in blood pressure.
Secondary causes of hypertension should be sought in children and adolescents who have substantial blood pressure elevation (consistently > 99th centile). Indications for pharmacological treatment of hypertension in children include secondary hypertension, evidence of target organ effects such as left ventricular hypertrophy, and failure of non‐pharmacological treatment. Although data from randomised trials are limited, several classes of medications have had a long history of safety and efficacy in children—for example diuretics, β blockers, angiotensin‐converting enzyme inhibitors, and calcium channel blockers.
GENETICS AND CARDIOVASCULAR RISK
A relatively small number of single gene defects have been identified that confer an increased risk of CHD—for example, the LDL receptor mutations of FH, mutations of apoB in familial defective apolipoprotein B, the ABCA‐1 mutation of Tangier's disease, and the cystathionine‐β synthase mutation of homocystinuria. However, the risk of CHD is modified by many genes each with small attributable effects. An understanding of the genetic basis of atherosclerosis has come from the identification of candidate genes and by the examination of gene polymorphisms and their associations in large predominantly adult populations. For example, common variations of apolipoprotein E (apoE), hepatic lipase, apoAI‐CIII‐AIV‐AV, apo(a) and paraoxonase‐1 (PON1) among others are associated with significant but small variations in CHD risk. With the identification of hundreds of thousands of genetic variations, particularly single nucleotide polymorphisms, throughout the human genome, it has become possible to perform whole genome‐association studies. The therapeutic implications of such genomic information have not yet been clearly established.
Childhood risk factors of cardiovascular disease: key points
The extent and severity of atherosclerosis in childhood is associated with the presence of risk factors such as hypertension, cigarette smoking, dyslipidaemia, obesity and diabetes mellitus
Early changes in arterial structure and function, indicative of vascular damage, may be detected in high‐risk children by non‐invasive diagnostic techniques
In overweight and obese children, improvements in arterial structure and function are best achieved by a programme of diet plus exercise
Both active and passive smoking in children and adolescents are associated with adverse changes in arterial structure and function
Statins have been shown to be safe and effective for use in children with hyperlipidaemia over the short term, although long‐term studies are required
In adolescents with type 1 diabetes mellitus, improved glycaemic control in conjunction with a reduction of exposure to other cardiovascular risk factors is likely to reduce the risk of future coronary heart disease (CHD)
A diet rich in fruit, vegetables and low fat dairy products, in addition to minimisation of salt intake, is likely to have a beneficial impact on hypertension in childhood
Intrauterine influences may be important in the development of future CHD, including the effects of fetal undernutrition and maternal hypercholesterolaemia
Children who are first‐degree relatives of subjects with premature clinical atherosclerosis have been shown to have reduced endothelial function and increased IMT. In future, this group may be the target of particular intervention strategies based upon their genotype (polymorphisms that confer increased CHD risk) and phenotype (presence of functional and structural arterial changes indicative of early arterial damage).
OTHER “AT RISK” GROUPS OF CHILDREN
Aortic coarctation
Children who have coarctation of the aorta are at a higher risk of future CHD, even after successful operative repair.19 Survivors of successful coarctation surgery have impaired arterial endothelial and smooth muscle function in the arteries proximal to the coarctation segment and increased IMT. Age at the time of initial operation, postoperative systolic blood pressure, and a residual pressure gradient appear to be important predictors of arterial structure and function and survival.
Low birth weight
A number of studies have found an inverse relationship between birth weight and CHD. More recently, low birth weight (LBW) and thinness during the first two years of life when followed by rapid weight has been shown to be associated with insulin resistance and coronary events in adult life. Skilton et al found an inverse correlation between LBW and aortic IMT in newborns, suggesting that the effects of LBW may be present from very early in life.20 The mechanism linking LBW to CHD requires further study. One effect of fetal undernutrition may be to switch on a “thrifty” metabolic setting that, in adult life, favours the development of metabolic syndrome and CHD.
CONCLUSIONS
Atherosclerosis begins in childhood and there currently is an increasing prevalence of children in both developed and developing nations with cardiovascular risk factors. It is now possible to detect early evidence of arterial disease. Major gains will likely accrue from public health strategies targeting overweight, exercise and cigarette smoking. Individualised atheroprotective strategies in childhood, however, will initially focus on the highest risk children such as those with familial hyperlipidaemia, diabetes, hypertension and obesity. In the future, genotype and phenotype information may allow the targeting of interventions in childhood that might prevent clinical vascular events in adult life.
Additional references appear on the Heart website—http://www.heartjnl.com/supplemental
Additional references appear on the Heart website—http://www.heartjnl.com/supplemental
Supplementary Material
Footnotes
In compliance with EBAC/EACCME guidelines, all authors participating in Education in Heart have disclosed potential conflicts of interest that might cause a bias in the article
Additional references appear on the Heart website—http://www.heartjnl.com/supplemental
References
- 1.Berenson G S, Srinivasan S R, Bao W.et al Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. N Engl J Med 19983381650–1656.This large autopsy series demonstrates that as the number of risk factors present in the young increases, the extent of atherosclerosis in the aorta and coronary arteries also increases. [DOI] [PubMed] [Google Scholar]
- 2.Daniels S R, Arnett D K, Eckel R H.et al Overweight in children and adolescents: pathophysiology, consequences, prevention, and treatment. Circulation 20051111999–2012. [DOI] [PubMed] [Google Scholar]
- 3.Celermajer D S, Sorensen K E, Gooch V M.et al Non‐invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet 19923401111–1115.Describes the technique of measuring FMD with high‐resolution ultrasound and determines the presence of impaired FMD in adults with established CHD or in both adults and children with risk factors. [DOI] [PubMed] [Google Scholar]
- 4.O'Leary D H, Polak J F, Kronmal R A.et al Carotid‐artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative Research Group. N Engl J Med 199934014–22. [DOI] [PubMed] [Google Scholar]
- 5.Davis P H, Dawson J D, Riley W A.et al Carotid intimal‐medial thickness is related to cardiovascular risk factors measured from childhood through middle age: the Muscatine study. Circulation 20011042815–2819.This study of a cohort of young adults, followed from childhood, demonstrates that the carotid IMT measured in adulthood is associated with risk factors present both in adults and in children. [DOI] [PubMed] [Google Scholar]
- 6.Hubert H B, Feinleib M F, McNamara P M.et al Obesity as an independent risk factor of cardiovascular disease: a 26‐year follow‐up of participants in the Framingham Heart Study. Circulation 198367968–977.This analysis of the Framingham cohort found that over a 26‐year period, obesity was a predictor of cardiovascular disease, independent of other risk factors. [DOI] [PubMed] [Google Scholar]
- 7.Woo K S, Chook P, Yu C W.et al Effects of diet and exercise on obesity‐related vascular dysfunction in children. Circulation 20041091981–1986. [DOI] [PubMed] [Google Scholar]
- 8.Tounian P, Aggoun Y, Dubern B.et al Presence of increased stiffness of the common carotid artery and endothelial dysfunction in severely obese children: a prospective study. Lancet 20013581400–1404.Initial demonstration of the impaired endothelial function and arterial stiffness present in overweight and obese children. [DOI] [PubMed] [Google Scholar]
- 9.Raitakari O T, Juonala M, Kähönen M.et al Cardiovascular risk factors in childhood and carotid artery intima‐media thickness in adulthood: the cardiovascular risk in young Finns study. JAMA 20032902277–2283. [DOI] [PubMed] [Google Scholar]
- 10.Howard G, Wagenknecht L E, Burke G L.et al Cigarette smoking and progression of atherosclerosis: the Atherosclerosis Risk in Communities (ARIC) study. JAMA 1998279119–124. [DOI] [PubMed] [Google Scholar]
- 11.Celermajer D S, Adams M R, Clarkson P.et al Passive smoking and impaired endothelium‐dependent arterial dilatation in healthy young adults. N Engl J Med 1996334150–154.This study of healthy young adults, whose only risk factor was exposure to cigarette smoke, demonstrates that passive smoking is associated with a dose dependent impairment of endothelial function. [DOI] [PubMed] [Google Scholar]
- 12.Napoli C, Glass C K, Wiztum J L.et al Influence of maternal hypercholesterolaemia during pregnancy on progression of early atherosclerotic lesions in childhood: Fate of Early Lesions in Children (FELIC) study. Lancet 19993541234–1241.This autopsy study demonstrated that children exposed to maternal hypercholesterolaemia during pregnancy had a more rapid rate of progression of atherosclerosis and suggests the potential for the fetal environment to affect future CHD risk. [DOI] [PubMed] [Google Scholar]
- 13.Leeson C P, Whincup P H, Cook D G.et al Cholesterol and arterial distensibility in the first decade of life: a population‐based study. Circulation 20001011533–1538. [DOI] [PubMed] [Google Scholar]
- 14.de Jongh S, Ose L, Szamosi T et a l. Efficacy and safety of statin therapy in children with familial hypercholesterolemia: a randomized, double‐blind, placebo‐controlled trial with simvastatin. Circulation 20021062231–2237. [DOI] [PubMed] [Google Scholar]
- 15.Wiegman A, Rodenburg J, de Jongh S.et al Family history and cardiovascular risk in familial hypercholesterolaemia: data in more than 1000 children. Circulation 20031071473–1478. [DOI] [PubMed] [Google Scholar]
- 16.Nathan D M, Lachin J, Cleary P.et al for the Diabetes Control and Complications Trial. Epidemiology of Diabetes Interventions and Complications Research Group. Intensive diabetes therapy and carotid intima‐media thickness in type 1 diabetes mellitus. N Engl J Med 20033482294–2303.This long term follow‐up study of the DCCT cohort demonstrates that intensive metabolic control of type 1 diabetes is associated with a reduction in the rate of cardiovascular events. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.De Ferranti S D, Gauvreau K, Ludwig D S.et al Prevalence of the metabolic syndrome in American adolescents: findings from the Third National Health and Nutrition Examination Survey. Circulation 20041102494–2497. [DOI] [PubMed] [Google Scholar]
- 18.Moore L L, Singer M R, Bradlee M L.et al Intake of fruits, vegetables, and dairy products in early childhood and subsequent blood pressure change. Epidemiology 2005164–11. [DOI] [PubMed] [Google Scholar]
- 19.Cohen M, Fuster V, Steele P M.et al Coarctation of the aorta: long term follow‐up and prediction of outcome after surgical correction. Circulation 198980840–845. [DOI] [PubMed] [Google Scholar]
- 20.Skilton M R, Evans N, Griffiths K A.et al Aortic wall thickness in newborns with intrauterine growth restriction. Lancet 20053651484–1486. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.