Abstract
Objective
To assess early outcomes in the elderly population undergoing coronary revascularisation with and without cardiopulmonary bypass (CPB).
Methods
Meta‐analysis of all retrospective, non‐randomised studies comparing off‐pump coronary artery bypass (OPCAB) versus CPB techniques in the elderly (> 70 years) between 1999 and 2005. Age‐related early outcomes of interest were death, stroke, atrial fibrillation (AF), renal failure and length of stay in hospital. The random effects model was used. Sensitivity and heterogeneity were analysed.
Results
Analysis of 14 non‐randomised studies comprising 4921 patients (OPCAB, 1533 (31.1%) and CPB, 3388 (68.9%)) showed a significantly lower incidence of death in the OPCAB group (odds ratio (OR) 0.48, 95% CI 0.28 to 0.84). This effect was greater in OPCAB octogenarians (OR 0.26, 95% CI 0.12 to 0.57). The pattern of incidence of stroke among the OPCAB octogenarians (OR 0.19, 95% CI 0.07 to 0.56) was similar. The incidence of AF was lower in the OPCAB group (OR 0.77, 95% CI 0.61 to 0.97). The incidence of renal failure did not differ. Length of hospital stay was shorter in the OPCAB group, although with significant heterogeneity.
Conclusions
OPCAB may be associated with lower incidence of death, stroke and AF in the elderly, which may result in shorter length of hospital stay. A large randomised trial would confirm whether the elderly would benefit more from OPCAB surgery.
The elderly constitute a challenging group of patients for cardiac surgery. Most of these patients have significant co‐morbidities; thus, coronary revascularisation is associated with increased risk of death and overall postoperative morbidity, compromising the length of stay and cost required. The past decade heralded improvements in surgical, anaesthetic and perfusion procedures. This progress led to coronary artery bypass grafting (CABG) being regarded as a safe option of treatment in this high risk group.1 Owing to the increased life expectancy in Western countries and a higher incidence of coronary artery disease in the developing world, surgical revascularisation in the elderly is increasing.2 More recently, off‐pump coronary artery bypass (OPCAB) techniques have been developed due to significant improvements in epicardial and apical suction stabilisation devices allowing surgeons to routinely perform multivessel coronary revascularisation by avoiding the invasiveness of cardiopulmonary bypass (CPB).
Advanced age has been shown to be an independent predictor of stroke, mortality, renal failure and atrial fibrillation (AF) after CABG.3,4,5 Our previous work has shown a reduced incidence of stroke and AF after OPCAB.6,7 Since then new studies8,9,10,11,12 have been added to the literature that warrant a re‐evaluation of these age‐related postoperative outcomes in the elderly population undergoing OPCAB or CPB surgery. This study aimed at answering the following questions. Firstly, is OPCAB associated with a lower incidence of mortality, stroke, AF and renal failure (requiring dialysis or haemofiltration) than conventional CABG? Secondly, does length of hospital stay differ between off‐pump and on‐pump groups of elderly patients? Thirdly, how do these differences respond in relation to five‐year increments of age?
PATIENTS AND METHODS
Literature search
Medline literature was searched for all the studies published in the English language between 1999 and 2005 reporting on elderly patients undergoing CABG with emphasis on comparisons between OPCAB and CPB techniques. The following MeSH terms were used: “Aged”, “80 and over”, “Cardiopulmonary bypass”, “Coronary artery bypass/*methods”, “Cerebrovascular accident/etiology/*prevention”, “Mortality”, “Renal failure”, “Comparative study”, “Coronary artery bypass/adverse effects/*methods/mortality”, and “Atrial fibrillation/aetiology”. The articles were also identified by using the function “related articles” in PubMed. All the abstracts, studies and citations scanned were reviewed. Fourteen of 267 studies were selected.
Data extraction
Data were extracted by two reviewers (SP and TA) and in the case of discrepancy the decision was taken by consensus. The following information was extracted from each study: first author, year of publication, study population characteristics, study design (prospective, retrospective or other), inclusion and exclusion criteria, number of patients operated on with each technique, quality of study and postoperative outcome measures discussed below.
The study was performed in line with the recommendations of the proposal for reporting meta‐analysis of observational studies in epidemiology.13 The quality of the non‐randomised studies was assessed by using a modified Newcastle–Ottawa Scale.14 The quality of the studies was evaluated by examining three items: patient selection, comparability of OPCAB and CPB groups and assessment of outcomes. Tables 1 and 2 show this.8,9,10,11,12,15,16,17,18,19,20,21,22,23
Table 1 Checklist for quality assessment and scoring* of non‐randomised studies.
| Selection | |
| 1. | Assignment for treatment: were any criteria reported? (If yes, one star) |
| 2. | Was the reference group (on‐pump coronary artery bypass) representative of the general elderly population for CABG? (If yes, one star; no star if the patients were selected or selection of group was not described.) |
| 3. | Was the treatment group (off‐pump coronary artery bypass) representative of the elderly population for CABG? (If drawn from the same community as the reference group, one star; no star if drawn from a different source or selection of group was not described.) |
| Comparability | |
| 4. | Was the group comparable for variables† 1, 2, 3, 4 and 5? (If yes, two stars; one star was assigned if one of these five characteristics was not reported even if there were no other differences between the two groups and other characteristics had been controlled for. No star was assigned if the two groups differed.) |
| 5. | Was the group comparable for variables† 6, 7, 8 and 9? (If yes, two stars; one star was assigned if one of these four characteristics was not reported even if there were no other differences between the two groups and other characteristics had been controlled for. No star was assigned if the two groups differed.) |
| Outcome assessment | |
| 6. | Was the outcome of interest clearly defined? (If yes, one star for information ascertained by record lineage or interview; no star was assigned if this information was not reported.) |
| 7. | Was follow up adequate? (One star if follow up was >90%.) |
*Studies were graded on an ordinal star scoring scale with higher scores indicating studies of higher quality. A study could be awarded a maximum of one star for each numbered item within the selection and exposure categories, and a maximum of four stars could be given for the comparability of the two groups. The quality of each study was graded as either level 1 (0–5) or level 2 (6–9).
†Comparability variables: 1, age; 2, sex; 3, diabetes; 4, hypertension; 5, ejection fraction; 6, history of vascular disease (cerebrovascular and peripheral); 7, non‐elective operation; 8, unstable angina; 9, repeat operation.
CABG, coronary artery bypass grafting.
Table 2 Assessment of the quality of the studies.
| Author, reference (year) | Selection | Comparability | Outcome assessment | Score | ||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | ||
| Ricci15 (2001) | * | * | * | * | * | * | ****** | |
| Meharwal16 (2002) | * | * | * | ** | ** | * | * | ********* |
| Hirose17 (2001) | * | * | ** | * | * | ****** | ||
| Al‐Ruzzeh18 (2001) | * | * | * | * | * | * | ****** | |
| Koutlas19 (2000) | * | * | * | * | * | ***** | ||
| Demaria20 (2002) | * | * | * | ** | * | * | * | ******** |
| Beauford8 (2003) | * | * | * | ** | * | * | ******* | |
| Hoff21 (2002) | * | * | * | * | * | * | * | ******* |
| Lin9 (2003) | * | * | ** | * | * | ****** | ||
| Boyd22 (1999) | * | * | * | ** | * | * | ******* | |
| Ascione23 (2002) | * | * | * | * | * | ***** | ||
| D'Alfonso10 (2004) | * | * | * | ** | * | * | ******* | |
| Shimokawa11 (2003) | * | * | ** | * | * | ****** | ||
| Deuse12 (2003) | * | * | * | * | * | * | * | ******* |
For the comparability between the two groups, we focused on the following variables that previous multivariate studies have identified as independent predictors of death and stroke: age, sex, diabetes, hypertension, ejection fraction, reoperation, non‐elective priority and history of cerebrovascular disease.24,25Tables 3 and 4 show the distribution of these variables.
Table 3 List of studies comparing OPCAB with CPB in elderly patients.
| Author, reference (year) | OPCAB/CPB | Exclusion criteria* | Matching criteria† | Criteria scoring‡ | Conversion | Definition of elderly (years) | Completeness of revascularisation (mean (SD) grafts/patient) | |
|---|---|---|---|---|---|---|---|---|
| OPCAB | CPB | |||||||
| Ricci15 (2001) | 483/1389 | 1, 3 | 2–4, 7–9, 11, 13–16 | 2 | 3 | >70 | 1.9 | 3.4 |
| Meharwal16 (2002) | 186/389 | 3, 4 | 1–8, 10–12, 14, 15 | 2 | ND | >70 | 2.9 (0.3) | 3.2 (0.4) |
| Hirose17 (2001) | 104/74 | ND | 1–10, 12–15 | 3 | ND | >75 | 2.4 (1.1) | 3.7 (1.0) |
| Al‐Ruzzeh18 (2001) | 56/87 | 2–4 | 1–4, 6–16 | 3 | ND | >75 | 2.71 (0.76) | 2.87 (0.57) |
| Koutlas19 (2000) | 53/220 | 3, 5 | 1–4, 6, 7, 12, 13, 15 | 1 | 3 | >75 | 1.5 (0.1) | 2.5 (0.1) |
| Demaria20 (2002) | 62/63 | ND | 1–11, 13–16 | 3 | ND | >80 | 2.6 (0.8) | 2.9 (0.7) |
| Beauford8 (2003) | 113/29 | ND | 1–4, 8, 9, 11–13, 15, 16 | 2 | ND | >80 | 3.3 (1.0) | ND |
| Hoff21 (2002) | 59/69 | 1, 2 | 1–3, 5, 7, 8, 13, 15, 16 | 1 | 0 | >80 | 2.6 | 3.6 |
| Lin9 (2003) | 12/17 | 3, 5 | 1–4, 6–9, 13, 15, 16 | 2 | ND | >80 | 3.1 (0.3) | 3.0 (0.14) |
| Boyd22 (1999) | 30/70 | ND | 1–3, 5, 6, 8, 13–15 | 1 | 0 | >70 | 1.7 (0.6) | 2.9 (0.9) |
| Ascione23 (2002) | 219/771 | ND | 2–5, 12, 15, 16 | 1 | 2 | >70 | 2.42 (0.84) | 3.01 (0.77) |
| D'Alfonso10 (2004) | 73/41 | ND | 1–4, 6–10, 13–15 | 2 | 3 | >80 | 2.7 (1.0) | 2.5 (0.8) |
| Shimokawa11 (2003) | 25/18 | 3 | 1–4, 7–10, 12–15 | 2 | 0 | >80 | 2.0 (1.0) | 2.8 (0.5) |
| Deuse12 (2003) | 53/66 | ND | 1–3, 6–8 | 1 | 3 | >75 | ND | ND |
*Exclusion criteria: 1, emergency operation; 2, minimally invasive direct coronary artery bypass grafting; 3, coronary grafting in combination with other cardiac surgical procedures; 4, <2 grafts; 5, repeat surgery; 6, catastrophic stage: unstable haemodynamic status or severe ischaemia that could not be stabilised with inotropes or intra‐aortic balloon pump.
†Matching criteria: 1, age; 2, sex; 3, diabetes; 4, hypertension; 5, repeat operation; 6, unstable angina; 7, history of pulmonary disease; 8, left ventricular function; 9, left main disease; 10, three‐vessel disease; 11, haemodynamic instability controlled by inotropes or intra‐aortic balloon pump; 12, non‐elective operation; 13, renal disease; 14, peripheral vascular disease; 15, cerebrovascular disease; 16, previous myocardial infarction.
‡Criteria scoring: 1, matched for 0–9 criteria; 2, matched for 10–13 criteria; 3, matched for 14–16 criteria.
CPB, cardiopulmonary bypass; ND, not documented; OPCAB, off‐pump coronary artery bypass.
Table 4 Distribution of preoperative risk factors between elderly patients in OPCAB and CPB groups.
| Author, reference (year) | Male sex | Hypertension | Diabetes | Unstable angina | Ejection fraction | Urgent/emergency surgery | COPD | CVD | PVD | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OPCAB | CPB | OPCAB | CPB | OPCAB | CPB | OPCAB | CPB | OPCAB | CPB | OPCAB | CPB | OPCAB | CPB | OPCAB | CPB | OPCAB | CPB | |
| Ricci15 (2001) | ND | ND | ND | ND | 101 | 313 | ND | ND | ND | ND | ND | ND | 141 | 373 | 153 | 453 | 94 | 271 |
| Meharwal16 2002 | 156 | 342 | 75 | 159 | 47 | 94 | 67 | 132 | 23* | 66* | 15 | 32 | 30 | 70 | 6 | 8 | 14 | 34 |
| Hirose17 (2001) | 60 | 54 | 65 | 45 | 40 | 28 | 23 | 7 | 7† | 7† | 11 | 7 | 6 | 3 | 24 | 10 | 4 | 6 |
| Al‐Ruzzeh18 (2001) | 44 | 64 | 24 | 46 | 13 | 11 | 28 | 40 | 29‡ | 40‡ | 20 | 32 | ND | ND | 4 | 5 | 2 | 10 |
| Koutlas19 (2000) | 30 | 114 | 42 | 163 | 13 | 66 | ND | ND | 53.9§ | 18.7§ | 36 | 172 | 6 | 18 | 6 | 24 | ND | ND |
| Demaria20 (2002) | ND | ND | ND | ND | ND | ND | 56 | 59 | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND |
| Beauford8 (2003) | 67 | 18 | 92 | 24 | 39 | 12 | ND | ND | 51§ | 49§ | 92 | 18 | ND | ND | 12 | 4 | ND | ND |
| Hoff21 (2002) | 31 | 92 | ND | ND | 18 | 39 | ND | ND | 4* | 8* | ND | ND | 10 | 20 | 6 | 14 | ND | ND |
| Lin9 (2003) | 13 | 8 | 10 | 7 | 6 | 3 | ND | ND | 53.4§ | 42§ | 4 | 3 | 2 | 1 | ND | ND | ND | ND |
| Boyd22 (1999) | 16 | 36 | ND | ND | 4 | 16 | ND | ND | 4† | 2† | 19 | 17 | ND | ND | 3 | 8 | 3 | 10 |
| Ascione23 (2002) | 163 | 558 | 133 | 483 | 28 | 112 | 94 | 398 | ND | ND | 139 | 466 | ND | ND | 35 | 81 | ND | ND |
| D'Alfonso10 (2004) | 49 | 24 | 41 | 17 | 19 | 10 | 23 | 14 | 7¶ | 0¶ | ND | ND | 7 | 1 | 7 | 4 | 6 | 3 |
| Shimokawa11 (2003) | 15 | 10 | 22 | 15 | 8 | 4 | ND | ND | 3† | 5† | 8 | 10 | 6 | 3 | 15 | 9 | 6 | 5 |
| Deuse12 (2003) | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND |
*Ejection fraction ⩽30%; †ejection fraction <40%; ‡ejection fraction <50%; §mean ejection fraction%; ¶ejection fraction <35%.
COPD, chronic obstructive pulmonary disease; CPB, cardiopulmonary bypass; CVD, cardiovascular disease; ND, not documented; OPCAB, off‐pump coronary artery bypass; PVD, peripheral vascular disease.
Inclusion criteria
The following criteria were used to include studies in our analysis: studies comparing OPCAB versus CPB in elderly patients (age > 70 years); where several articles reported on the same patient material, we selected the most recent article or the article with the greatest detail of information; and where studies originated from the same institution and had the same authors, the one that focused on the oldest patient group was used.
Exclusion criteria
The following criteria were used to exclude studies from our analysis: studies in which the surgical technique (whether OPCAB or CPB) could not be defined; studies in which the outcome of comparison of both techniques was not reported or it was not possible to calculate this from the published results; and studies that contained a zero for the outcome of interest in two cells of the cross‐tabulation tables for both OPCAB and CPB groups.
Outcomes of interest and definitions
OPCAB and CPB were compared, with mortality and stroke being the major outcomes of interest. Secondary outcomes of interest were AF, renal failure (requiring dialysis or haemofiltration) and length of stay in hospital (days). Mortality was defined as short‐term or actual 30‐day mortality. We extracted the “mortality” statistics as they appeared in the postoperative outcomes tables of the various studies. Permanent stroke was the major outcome of interest and data on it were extracted if recorded as “stroke” or “permanent stroke”. We ignored other neurological outcomes including transient ischaemic attacks, stupor, impairment (deterioration) of intellectual function and seizures.
Studies mentioning “atrial fibrillation” as a postoperative outcome were identified. We did not focus on any other arrhythmias including supraventricular or ventricular types. The studies used in this meta‐analysis excluded patients with pre‐existing AF. Furthermore, different studies may have had different definitions for AF such as intermittent or persistent. It was not the purpose of this study to distinguish between these. Renal failure was distinguished from renal dysfunction. Our focus was on renal failure requiring dialysis or haemodialysis postoperatively. Different protocols are used to institute renal support on the basis of serum creatinine concentrations. We appreciate that this may have affected the incidence of the outcome of interest. It was not the objective of the study to analyse these different protocols. We were interested in the number of patients who required some form of renal support postoperatively. The length of hospital stay after the procedure was recorded as the number of days spent in the hospital postoperatively.
We did not analyse the different modifications in the operative technique used by different surgeons.
Statistical analysis
The group where CPB was used was regarded as the reference group and that in which OPCAB was used, the treatment group. The Mantel–Haenszel method was used to combine the odds ratio (OR) for the outcomes of interest. We used both fixed and random effect models.
Three strategies were used to quantitatively assess heterogeneity. Firstly, data were reanalysed by using both fixed and random effect models. Secondly, graphical exploration with funnel plots was used to evaluate publication bias.26 Thirdly, sensitivity analysis was undertaken by using subgroup analysis. To do this, the following variables were evaluated: (a) all studies; (b) study size (> 50 patients in each arm); (c) matching criteria score of 3; and (d) higher quality studies (level 2).
To translate these results into benefits to clinical outcome of the OPCAB technique, we calculated the absolute risk reduction and the number needed to treat.
Data were analysed by using the statistical software SPSS V.12.0 for Windows (SPSS Inc, Chicago, Illinois, USA), Intercooled Stata V.7.0 for Windows (StataCorp, College Station, Texas, USA), RevMan V.4.2 (The Cochrane Collaboration, http://www.cc‐ims.net/RevMan) and the Sample Power V. 2.0 (SPSS Inc) for power analysis calculations.
Sample size considerations
Death is a rare categorical outcome and was indeed our major outcome of interest. The incidence of death in the CPB group was about 4% (149 of 3388), allowing us to assume that, to rule out a 50% relative risk reduction (from 4% to 2 %) with a 5% significance level and 90% power, a traditional randomised controlled trial would require 4444 patients. On the basis of a 3:1 ratio (CPB:OPCAB), this equates to 3333:1111.
RESULTS
Selected studies
The previously mentioned criteria identified 17 studies comparing OPCAB versus CPB in the elderly.8,9,10,11,12,15,16,17,18,19,20,21,22,23,27,28,29 We excluded three studies.27,28,29 One study27 overlapped with another one20 that was more informative and focused on octogenarians. The other two studies28,29 included duplicate data and used the same cohort during the same period (January 1995 to May 1999) as the paper15 that had a larger data set and was more recent. Fourteen studies8,9,10,11,12,15,16,17,18,19,20,21,22,23 were selected. These were all non‐randomised retrospective studies dating from 2000–4 and contained 4921 patients, of whom 1533 (31.1%) underwent OPCAB and 3388 (68.9%) CPB. Tables 3 and 4 show further details of these studies.
On review of the data extraction agreement between the two reviewers was 100% and the agreement on quality score of the individual studies was very high (weighted κ = 0.96). Two of 14 studies were ranked at level 119,23 and the remaining studies were classified as level 2.8,9,10,11,12,15,16,17,18,20,21,22,23,24,25,26 Conversion rate was reported in eight studies.10,11,12,15,19,21,22,23 Nine studies were classified as larger and had > 50 patients in each group.12,15,16,17,18,19,20,21,23
Meta‐analysis
The meta‐analysis was performed by stratifying the studies according to patients' ages (> 70 years (group 1), > 75 years (group 2) and > 80 years (group 3)), scoring on the matching criteria, level 1 or 2 studies and the size of the study (larger studies included > 50 patients for each technique and smaller studies comprised ⩽ 50 patients for each technique).
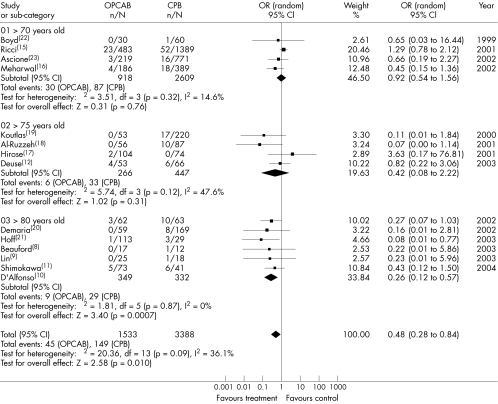
Mortality
Overall mortality was significantly lower in the OPCAB group (OR 0.48, 95% confidence interval (CI) 0.28 to 0.84) with no significant heterogeneity between the studies. One study in group 321 reported a significant difference in mortality between the OPCAB and CPB groups. Furthermore, subgroup analysis of the octogenarians in group 3 comprising 349 of 1533 (22.8%) patients in the OPCAB group and 332 of 3388 (9.8%) patients in the CPB group showed that mortality was significantly lower in the octogenarian OPCAB group (OR 0.26, 95% CI 0.12 to 0.57, χ2 = 1.81, p = 0.87) (fig 1). Level 2 studies indicated a lower mortality in the OPCAB group (OR 0.48, 95% CI 0.26 to 0.89, χ2 = 18.38, p = 0.07).
Figure 1 Comparison between off‐pump coronary artery bypass (OPCAB) and on‐pump cardiopulmonary bypass (CPB) in the elderly: postoperative mortality stratified by age (random effects model). CI, confidence interval; OR, odds ratio.
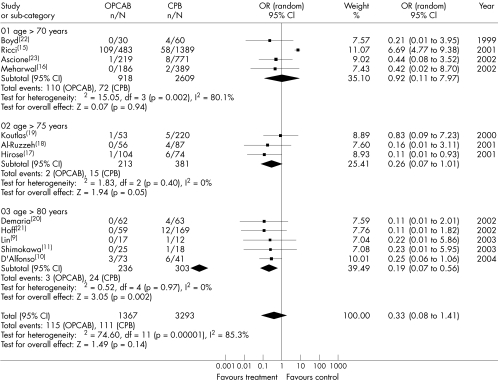
Stroke
Overall, the incidence of stroke tended to be lower in the OPCAB group (OR 0.33, 95% CI 0.08 to 1.41, χ2 = 74.60, p < 0.001). The incidence of stroke in group 1 did not vary significantly between the two techniques. One study in group 225 showed a significant difference in the incidence of stroke between the OPCAB and CPB groups (OR 0.11, 95% CI 0.01 to 0.93). Analysis of group 2, which comprised 213 of 1533 (13.9%) OPCAB patients and 381 of 3388 (11.2%) CPB patients, showed that stroke in the OPCAB group was lower than that in the CPB group (OR 0.26, 95% CI 0.07 to 1.01, χ2 = 1.83, p = 0.40). Furthermore, subgroup analysis of the octogenarians in group 3 showed that 236 of 1533 (15.4%) patients in the OPCAB group and 303 of 3388 (8.9%) patients in the CPB group had had stroke. The octogenarian OPCAB group experienced significantly less stroke (OR 0.19, 95% CI 0.07 to 0.56, χ2 = 0.52, p = 0.97) (fig 2). The results from group 2 and group 3 probably skewed the data more towards benefit in the OPCAB group. Studies with a matching criteria score of 3 showed a significant decrease in stroke after OPCAB (OR 0.12, 95% CI 0.03 to 0.54, χ2 = 0.06, p = 0.97).
Figure 2 Comparison between off‐pump coronary artery bypass (OPCAB) and on‐pump cardiopulmonary bypass (CPB) in the elderly: postoperative stroke stratified by age (random effects model). CI, confidence interval; OR, odds ratio.
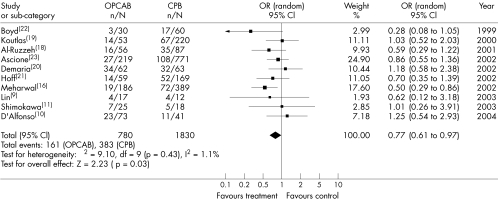
Atrial fibrillation
One of 11 studies showed a significant difference between the two groups in the incidence of AF.15 By using the random effect model we calculated an OR of 0.77 with 95% CI 0.61 to 0.97 and a χ2 of heterogeneity of 9.10 (p = 0.43). This suggests a significant reduction in the incidence of AF in the OPCAB group. Individual group analysis according to age showed no difference in the outcome of AF. Post‐OPCAB AF decreased significantly in level 2 studies and larger studies, as fig 3 shows (OR 0.71, 95% CI 0.52 to 0.96, χ2 = 7.75, p = 0.35 and OR 0.76, 95% CI 0.59 to 0.99, χ2 = 5.34, p = 0.38, respectively). After reanalysis of the data and exclusion of the study by Meharwal et al,16 post‐OPCAB AF was still significantly decreased (OR 0.78, 95% CI 0.63 to 0.97, χ2 = 7.64, p = 0.57).
Figure 3 Comparison between off‐pump coronary artery bypass (OPCAB) and on‐pump cardiopulmonary bypass (CPB) in the elderly: postoperative atrial fibrillation stratified by age (random effects model). CI, confidence interval; OR, odds ratio.
Renal failure
Renal failure (requiring dialysis or haemofiltration) was comparable in both groups. In 28 of 1095 (2.6%) patients in the OPCAB group and 78 of 2757 (2.8%) patients in the CPB group, the incidence of renal failure was lower in the OPCAB group (OR 0.75, 95% CI 0.48 to 1.19, χ2 = 3.39, p = 0.23). Stratification according to age, quality and size of studies did not yield any differences.
Length of hospital stay
There was a tendency towards shorter hospital stay in the OPCAB group (OR −2.09, 95% CI −3.55 to −0.63, χ2 = 62.95, p < 0.001). The three age groups when considered separately did not have any significantly reduced hospital stay for the OPCAB group. The length of post‐OPCAB hospital stay decreased significantly in level 2 studies and studies with a matching criteria score of 2 (OR −2.41, 95% CI −3.94 to −0.89, χ2 = 43.25, p < 0.001 and OR −3.32, 95% CI −6.20 to −0.43, χ2 = 22.49, p < 0.001, respectively).
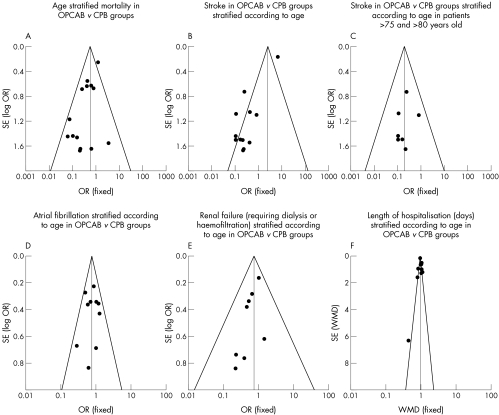
Sensitivity analysis
Sensitivity analysis for mortality did not identify any significant differences in the ORs and heterogeneity by both random and fixed effect models. Figure 4 shows all the funnel plots. The plot in fig 4A for mortality resembles a symmetrical inverted funnel (95% CI) inside which are all studies except one.15 Sensitivity analysis for the incidence of stroke as shown by the funnel plot in fig 4B shows significant heterogeneity among the studies, which was reduced when only groups 2 and 3 were included (fig 4C). The studies looking at the outcomes of AF and renal failure (fig 4D, E) were non‐heterogeneous. Sensitivity analysis for the length of hospital stay showed a heterogeneous group of studies with many studies on the borders of the funnel plot (fig 4F).
Figure 4 Funnel plots for (A) mortality, (B, C) stroke, (D) atrial fibrillation, (E) renal failure and (F) length of hospital stay.
DISCUSSION
Our meta‐analysis shows a lower incidence of postoperative mortality and AF in an elderly population with OPCAB than with CPB techniques. This stratified meta‐analysis identified that, among all the elderly patients, octogenarians are more likely to benefit from OPCAB, as the reduction in the incidence of stroke and death was more prominent. However, the lack of finding a difference in the 70–80‐year‐old groups is probably due to a lack of power of the individual trials considered in this meta‐analysis. The use of meta‐analytical techniques allowed inclusion of a total of 4921 patients (1533 (31.1%) OPCAB and 3388 (68.9%) CPB). A sample group of this size would otherwise be impossible to accumulate in a reasonable length of time in a randomised control trial.
Despite this, we believe that our results highlight an important link between CPB and the incidence of postoperative death, stroke and AF in the elderly. As figs 1–3 show the maximum OR favouring the treatment (OPCAB) group was 0.84 (within 95% CI) for mortality, 0.56 for stroke (in octogenarians) and 0.97 for AF meaning a relative risk reduction of at least 16%, 44% and 3%, respectively. For the studies included in our analysis, the average incidences of death, stroke (octogenarian group) and AF in elderly patients undergoing CPB were 4%, 8% and 21%, respectively. Therefore, a 16% reduction in mortality would translate to an incidence of death with OPCAB of 3.4%. The calculated absolute risk reduction would be 0.6% with OPCAB and the number needed to treat would be 167. This number hypothetically would be less for patients at high risk of death (for example, with diabetes and left ventricular dysfunction).The number needed to treat for stroke and AF was calculated to be 29 and 5, respectively.
Several meta‐analyses30,31,32,33,34 have compared outcomes after OPCAB and CPB. Reston et al30 showed that the OPCAB technique was associated with superior early outcomes in the parameters of operative mortality, stroke, renal failure, AF and length of hospital stay. Recently Wijeysundera et al31 showed that meta‐analysis of randomised controlled trials did not find any significant reduction in early mortality and morbidity, which had previously been shown by observational studies. Another recent meta‐analysis by Cheng et al32 showed no significant benefit of OPCAB versus CPB with regard to mortality, stroke and renal failure. It did, however, show that the OPCAB technique significantly decreased AF. Two more meta‐analyses showed favourable results for OPCAB, although they were based on the analysis of composite end points of mortality, stroke and myocardial infarction. The risk reduction did not reach significance in both cases.33,34
These discrepancies between meta‐analyses may have several reasons: firstly, the different number and design of studies included; secondly, all the above‐mentioned meta‐analyses were based on the general CABG population rather than the elderly group (as the mean age of the patient population in each study was < 70 years); and, thirdly, the patients included in the meta‐analyses of randomised trials most likely had lower operative risks, taking into account the enrolment criteria of the trials. Furthermore, we need to keep in mind that some OPCAB operators may not use the technique regularly and would not have completed the learning curve.35 We must not overlook the benefits of the OPCAB procedure in the elderly, as most of the literature looks at the non‐elderly. Our study is the first that has shown a significant decrease in mortality among the elderly, who may indeed be the true beneficiaries of the OPCAB technique.
Our meta‐analysis suggests that the OPCAB technique may be associated with a reduced risk of stroke in the elderly. The current evidence suggests that avoidance of CPB may reduce the risk of major neurological complications, a finding that would have some impact on the consideration of elderly patients for CABG without adding an economic burden on the healthcare providers.6 The underlying mechanisms highlighting the better outcome of OPCAB with regard to stroke in elderly patients are likely to include less manipulation of the ascending aorta by avoiding cross clamping and aortic cannulation and use of “no‐touch” techniques with T or Y grafts.6 We have shown a significantly lower incidence of AF in the elderly. In the elderly, several mechanisms directly related to the CPB technique may be responsible for the greater incidence of AF than with OPCAB. These have been described previously7 and include regional ischaemia, better subendocardial and interventricular septal blood supply and less myocardial injury in the OPCAB group.
We observed no difference in the incidence of renal failure between the two groups. This finding needs further investigation. In a recent study we have shown that the OPCAB technique may reduce the risk of minor and major renal adverse outcomes postoperatively.36 OPCAB results in decreased complement activation and higher systemic blood pressure, thereby conferring renoprotection.36
The length of hospitalisation was shorter in the OPCAB group. However, this finding must be interpreted cautiously, as there was significant heterogeneity among the different groups. Length of stay is related to different discharge policies applied in different institutions. Practically it is impossible to adjust for these differences in a meta‐analysis. A previous study showed that short‐term hospital stay was less in the OPCAB group.37 The fact that OPCAB has fewer adverse effects associated with it may result in shorter hospital stay, especially among the elderly. This undoubtedly results in an increased cost: benefit ratio and a better quality of life.
Limitations of the study
The findings of this meta‐analysis must be interpreted with caution. Firstly, the design of the study may lack the experimental element of a random allocation to OPCAB or to CPB, and only a few studies included in the meta‐analysis reported the criteria considered by the individual surgeons to allocate patients to the OPCAB or CPB group. Selection bias can also be related to the fact that different surgeons performed the two techniques (OPCAB or CPB) without any adjustment for surgeon‐related morbidity, learning curve and different revascularisation strategies (more extended use of bilateral internal thoracic arteries). Secondly, the two groups were not comparable for all the factors that can alter the outcome of interest, and confounding factors cannot be excluded.
It is worth mentioning that most of the studies included in our meta‐analysis had higher mean numbers of grafts used in the CPB group, which supports the view that revascularisation was more likely to be incomplete in the OPCAB group. It was not possible in our study to evaluate the clinical importance of this observation in the early outcome.
Publication bias can exist when a meta‐analysis relies on previously published studies, because positive results are more likely to be published than negative results. Meta‐analysis is most effective when randomised studies are analysed.38 However, in this case this was not possible, as only observational studies have been performed.
Conclusion
Our study suggests that OPCAB, a less invasive procedure, may reduce mortality, major neurological morbidity and the incidence of AF in the elderly population requiring surgical myocardial revascularisation. Further prospective, multicentre trials are required to confirm the findings of this meta‐analysis.
Abbreviations
AF - atrial fibrillation
CABG - coronary artery bypass grafting
CPB - cardiopulmonary bypass
OPCAB - off‐pump coronary artery bypass
OR - odds ratio
Footnotes
Funding: None declared.
Competing interests: None declared.
References
- 1.Ascione R, Caputo M, Angelini G D. Off‐pump coronary artery bypass grafting: not a flash in the pan. Ann Thorac Surg 200375306–313. [DOI] [PubMed] [Google Scholar]
- 2.Edmunds L H, Jr, Stephenson L W, Edie R N.et al Open‐heart surgery in octogenarians. N Engl J Med 1988319131–136. [DOI] [PubMed] [Google Scholar]
- 3.Mangano C M, Diamondstone L S, Ramsay J G.et al Renal dysfunction after myocardial revascularization risk factors, adverse outcomes, and hospital resource utilization. Ann Intern Med 1998128194–203. [DOI] [PubMed] [Google Scholar]
- 4.Amar D, Zhang H, Leung D H.et al Older age is the strongest predictor of postoperative atrial fibrillation. Anesthesiology 200296352–356. [DOI] [PubMed] [Google Scholar]
- 5.Stamou S C, Dangas G, Dullum M K.et al Beating heart surgery in octogenarians: perioperative outcome and comparison with younger age groups. Ann Thorac Surg 2000691140–1145. [DOI] [PubMed] [Google Scholar]
- 6.Athanasiou T, Al‐Ruzzeh S, Kumar P.et al Off‐pump myocardial revascularization is associated with less incidence of stroke in elderly patients. Ann Thorac Surg 200477745–753. [DOI] [PubMed] [Google Scholar]
- 7.Athanasiou T, Aziz O, Mangoush O.et al Does off‐pump coronary artery bypass reduce the incidence of post‐operative atrial fibrillation? A question revisited. Eur J Cardiothorac Surg 200426701–710. [DOI] [PubMed] [Google Scholar]
- 8.Beauford R B, Goldstein D J, Sardari F F.et al Multivessel off‐pump revascularization in octogenarians: early and midterm outcomes. Ann Thorac Surg 20037612–7 discussion 17. [DOI] [PubMed] [Google Scholar]
- 9.Lin C Y, Hong G J, Lee K C.et al Off‐pump technique in coronary artery bypass grafting in elderly patients. Aust N Z J Surg 200373473–476. [DOI] [PubMed] [Google Scholar]
- 10.D'Alfonso A, Mariani M A, Amerini A.et al Off‐pump coronary surgery improves in‐hospital and early outcomes in octogenarians. Ital Heart J 20045197–204. [PubMed] [Google Scholar]
- 11.Shimokawa T, Minato N, Yamada N.et al Off‐pump coronary artery bypass grafting in octogenarians. Jpn J Thorac Cardiovasc Surg 20035186–90. [DOI] [PubMed] [Google Scholar]
- 12.Deuse T, Detter C, Samuel V.et al Early and midterm results after coronary artery bypass grafting with and without cardiopulmonary bypass: which patient population benefits the most? Heart Surg Forum 2003677–83. [DOI] [PubMed] [Google Scholar]
- 13.Stroup D F, Berlin J A, Morton S C.et al Meta‐analysis of observational studies in epidemiology. JAMA 20002832008–2012. [DOI] [PubMed] [Google Scholar]
- 14.Taggart D P, D'Amico R, Altman D G. Effect of arterial revascularization on survival: a systematic review of studies comparing bilateral and single internal mammary arteries. Lancet 2001358870–875. [DOI] [PubMed] [Google Scholar]
- 15.Ricci M, Karamanoukian H L, Dancona G.et al On‐pump and off‐pump coronary artery bypass grafting in the elderly: predictors of adverse outcome. J Card Surg 200116458–466. [DOI] [PubMed] [Google Scholar]
- 16.Meharwal Z S, Trehan N. Off‐pump coronary artery surgery in the elderly. AsianCardiovasc Thorac Ann200210206–210. [DOI] [PubMed] [Google Scholar]
- 17.Hirose H, Amano A, Takahashi A. Off‐pump coronary artery bypass grafting for elderly patients. Ann Thorac Surg 2001722013–2019. [DOI] [PubMed] [Google Scholar]
- 18.Al‐Ruzzeh S, George S, Yacoub M.et al The clinical outcome of off‐pump coronary artery bypass surgery in the elderly patients. Eur J Cardiothorac Surg 2001201152–1156. [DOI] [PubMed] [Google Scholar]
- 19.Koutlas T C, Elbeery J R, Williams J M.et al Myocardial revascularization in the elderly using beating heart coronary artery bypass surgery. Ann Thorac Surg 2000691042–1047. [DOI] [PubMed] [Google Scholar]
- 20.Demaria R G, Carrier M, Fortier S.et al Reduced mortality and strokes with off‐pump coronary artery bypass grafting surgery in octogenarians. Circulation 2002106(12 Suppl 1)I5–10. [PubMed] [Google Scholar]
- 21.Hoff S J, Ball S K, Coltharp W H.et al Coronary artery bypass in patients 80 years and over: is off‐pump the operation of choice? Ann Thorac Surg 200274S1340–S1343. [DOI] [PubMed] [Google Scholar]
- 22.Boyd W D, Desai N D, Del Rizzo D F.et al Off‐pump surgery decreases postoperative complications and resource utilization in the elderly. Ann Thorac Surg 1999681490–1493. [DOI] [PubMed] [Google Scholar]
- 23.Ascione R, Rees K, Santo K.et al Coronary artery bypass grafting in patients over 70 years old: the influence of age and surgical technique on early and mid‐term clinical outcomes. Eur J Cardiothorac Surg 200222124–128. [DOI] [PubMed] [Google Scholar]
- 24.Ascione R, Reeves B C, Chamberlain M H.et al Predictors of stroke in the modern era of coronary artery bypass grafting: a case control study. Ann Thorac Surg 200274474–480. [DOI] [PubMed] [Google Scholar]
- 25.Kouchoukos N T, Oberman A, Kirklin J W.et al Coronary bypass surgery: analysis of factors affecting hospital mortality. Circulation 198062(Suppl 1)84–89. [PubMed] [Google Scholar]
- 26.Stuck A E, Rubenstein L Z, Wieland D. Bias in meta‐analysis detected by a simple, graphical test: asymmetry detected in funnel plot was probably due to true heterogeneity [letter]. BMJ 1998316469–471. [PMC free article] [PubMed] [Google Scholar]
- 27.Demers P, Cartier R. Multivessel off‐pump coronary artery bypass surgery in the elderly. Eur J Cardiothorac Surg 200120908–912. [DOI] [PubMed] [Google Scholar]
- 28.Ricci M, Karamanoukian H L, Abraham R.et al Stroke in octogenarians undergoing coronary artery surgery with and without cardiopulmonary bypass. Ann Thorac Surg 2000691471–1475. [DOI] [PubMed] [Google Scholar]
- 29.D'Ancona G, Karamanoukian H, Kawaguchi A T.et al Myocardial revascularization of the beating heart in high‐risk patients. J Card Surg 200116132–139. [DOI] [PubMed] [Google Scholar]
- 30.Reston J T, Tregear S J, Turkelson C M. Meta‐analysis of short‐term and mid‐term outcomes following off‐pump coronary artery bypass grafting. Ann Thorac Surg 2003761510–1515. [DOI] [PubMed] [Google Scholar]
- 31.Wijeysundera D N, Beattie W S, Djaiani G.et al Off‐pump coronary artery surgery for reducing mortality and morbidity meta‐analysis of randomized and observational studies. J Am Coll Cardiol 200546872–882. [DOI] [PubMed] [Google Scholar]
- 32.Cheng D C, Bainbridge D, Martin J E.et al Evidence‐Based Perioperative Clinical Outcomes Research Group. Does off‐pump coronary artery bypass reduce mortality, morbidity, and resource utilization when compared with conventional coronary artery bypass? A meta‐analysis of randomized trials. Anesthesiology 2005102188–203. [DOI] [PubMed] [Google Scholar]
- 33.Van der Heijden G J, Nathoe H M, Jansen E W.et al Meta‐analysis on the effect of off‐pump coronary bypass surgery. Eur J Cardiothorac Surg 20042681–84. [DOI] [PubMed] [Google Scholar]
- 34.Parolari A, Alamanni F, Cannata A.et al Off‐pump versus on‐pump coronary artery bypass: meta‐analysis of currently available randomized trials. Ann Thorac Surg 20037637–40. [DOI] [PubMed] [Google Scholar]
- 35.Ngaage D L. Off‐pump coronary artery bypass grafting: the myth, the logic and the science. Eur J Cardiothorac Surg 200 24557–570. [DOI] [PubMed] [Google Scholar]
- 36.Weerasinghe A, Athanasiou T, Al‐Ruzzeh S.et al Functional renal outcome in on‐pump and off‐pump coronary revascularization: a propensity‐based analysis. Ann Thorac Surg 2005791577–1583. [DOI] [PubMed] [Google Scholar]
- 37.Van Dijk D, Nierich A P, Jansen E W.et al Octopus Study Group. Early outcome after off‐pump versus on‐pump coronary bypass surgery: results from a randomized study, Circulation 20011041761–1766. [DOI] [PubMed] [Google Scholar]
- 38.Blettner M, Sauerbrei W, Schlehofer B.et al Traditional reviews, meta‐analyses and pooled analyses in epidemiology. Int J Epidemiol 1999281–9. [DOI] [PubMed] [Google Scholar]