Abstract
Objective
To investigate trends in case‐fatality and prognostic impact from recurrent acute myocardial infarction (re‐AMI) during 1985–2002.
Design
Retrospective cohort study using nationwide administrative data from Denmark.
Settings
National registries on hospital admissions and causes of death were linked to identify patients with first AMI, re‐AMI and subsequent prognosis.
Patients
Patients ⩾30 years old with a discharge diagnosis of AMI during 1985–2002 were tracked for first hospital admission for re‐AMI 1 year after discharge.
Main outcome measures
One‐year case‐fatality.
Results
166 472 patients were identified with a first AMI; 14 123 developed re‐AMI. One‐year crude case‐fatality from first AMI/re‐AMI was 39% versus 43% in 1985–1989 and 25% versus 29% in 2000–2002, respectively. In 1985–89, 35 795 patients survived to discharge (71%); of these 2.5% experienced reinfarction within 30 days (early reinfarction) and an additional 9.0% reinfarction within days 31–365 (late re‐AMI). Re‐AMI carried a poor prognosis in 1985–1989 compared to no re‐AMI with age‐ and sex‐adjusted relative risk of 1‐year case‐fatality of 7.5 (95% CI: 6.9 to 8.5) from early re‐AMI and 11.7 (95% CI: 11.0 to 12.4) from late re‐AMI. In 2000–2002, 23 552 patients (86%) survived to discharge; 4.4% had early re‐AMI and 6.6% late re‐AMI. Adjusted relative risk of 1‐year case‐fatality had declined to 2.1 (95% CI: 1.9 to 2.5) from early re‐AMI and 5.6 (95% CI: 5.1 to 6.2) from late re‐AMI compared to patients without reinfarction.
Conclusion
Prognosis after AMI has improved substantially during the latest two decades and extends to patients with re‐AMI.
Keywords: acute myocardial infarction, mortality, prognosis, reinfarction, trends
A recurrent acute myocardial infarction (AMI) is generally considered a serious event in survivors of myocardial infarction, and many studies have demonstrated a high risk of subsequent death.1,2,3,4 During the last two decades the mortality from an AMI has decreased considerably, influenced by multiple factors including improvement in treatment and changes in lifestyle.5,6 Whether the prognosis of a recurrent AMI has changed in a similar manner is largely unknown. A decrease in mortality from recurrent AMI would be anticipated because of the widespread use of secondary prevention and intensified treatment of patients with established coronary artery disease. Further, the increasing use of more sensitive biomarkers and new definitions of an AMI may have changed the prognostic impact of a recurrent AMI in an unknown manner.7
Information about the prognostic implication of a recurrent infarction is important for many reasons. Not only is it important in patient management and counselling, but recurrent AMI is also considered a valid endpoint in clinical trials. Several major new treatment strategies have been introduced based on studies where the clinical benefit was reduction of recurrent AMI.8,9,10 Due to the substantial decline in mortality from a first AMI, it is necessary to know the extent to which this applies to a recurrent AMI. Therefore, we have performed a nationwide register‐based study to follow the trends in mortality after a recurrent AMI from 1985 to 2002.
Methods
This study was based on administrative data from the Danish National Patient Registry, which covers all admissions to Danish hospitals since 1978.11 Briefly, the registry contains basic information about the patient (age and gender), dates of admission and discharge, and all diagnoses during hospital stay. Data for the registry are processed at each hospital discharge and include a primary discharge diagnosis coded according to the International Classification of Diseases (ICD) by the discharging physician. We identified patients aged 30 years or older with a first admission for an AMI during the period 1 January 1985 to 31 December 2002. The population was subsequently tracked for first hospitalisation for recurrent AMI occurring within the first year after discharge. The rationale for the follow‐up duration of 1 year was a clustering of events during the first 6 months and far fewer events after this. Information on survival status was obtained from the Civil Registration System which registers all deaths in Denmark within 2 weeks. One‐year mortality status was available for all patients.
Definitions of a first AMI and a recurrent AMI
A first AMI was defined as first hospital admission recorded in the National Patient Registry on condition that no previous AMI had been recorded in the preceding 7 years. This arbitrary limit was selected because this was the furthest back we were able to trace patients admitted in 1985, and this length of time was applied to all patients in our cohort. To identify the hospitalisations for a first AMI or a first recurrent AMI we used the ICD‐8 code 410 (from 1978 to 1994) and ICD‐10 code I21–22 (from 1994 to 2002). Only primary discharge diagnoses were used. A recurrent AMI was defined as any new admission for AMI within 1 year after discharge following the initial AMI, provided that the interval between the day of admission for first AMI and the day of admission for the recurrent AMI was at least 5 days to avoid misclassification. If a patient experienced more than one reinfarction, only the first was used in analyses.
Validation of the diagnosis of a first and a recurrent AMI
The diagnosis of AMI in the National Hospital Registry has been validated against the Danish Monitoring Trends and Determinants of Cardiovascular Disease (MONICA) Registry where standardised WHO definitions of AMI are used. The positive predictive value was 93.6% and sensitivity was 78% for definite or possible AMI (93% for definite AMI).12 To study the validity of a recurrent AMI diagnosis, we randomly validated 48 diagnoses in two hospitals by a review of the hospital records. To be classified as a definite recurrent AMI, two out of three criteria had to be fulfilled: clinical symptoms together with either significant enzyme/troponin rise or ST‐segment changes. We only chose recent cases between 2000 and 2001 so that we could obtain a complete sample of the records. Of these 48 patients, 40 (83%) were retrospectively found to have a definite recurrent AMI and an additional three had possible reinfarction, leaving 90% with a diagnosis of definite or possible reinfarction. In patients where the diagnosis of a recurrent AMI could not be confirmed, two had angina, one had congestive heart failure and two were incorrectly coded as AMI during revascularisation procedures.
Statistics
The calendar years from 1985 to 2002 were categorised into four pre‐selected periods: 1985–1989, 1990–1994, 1995–1999 and 2000–2002. We chose a shorter interval for the latest period to make a clear cut at year 2000, when the definition of AMI changed according to international guidelines. The remaining periods were divided into equal intervals of 4 years. Due to the frequent use of early reinfarction as the endpoint in recent trials, we investigated trends in mortality from both early and late recurring AMI. A recurrent AMI was categorised as early if it occurred within the first 30 days of the initial AMI (counting from the day of admission) or late if it occurred from day 31 to 365.
Trends in continuous baseline variables were tested by one‐way variance analysis and categorical variables by χ2 test. One‐year case‐fatality plots, stratified by period, were generated separately for the whole AMI population, that is, all patients with first time AMI, and for patients with a recurrent AMI by means of the Kaplan–Meier method and compared by the log‐rank test. Lifetime was calculated as time from admission for either first AMI or recurrent AMI.
A Cox proportional hazard model was used to estimate hazard rates of case‐fatality from first AMI or recurrent AMI during periods with the earliest period (1985–1989) as reference. The model was adjusted for sex and age (10‐year age groups). To compare risk of death within the first year between patients with a recurrent AMI and patients without a recurrent AMI, an extended Cox model was used, in which recurrent AMI served as a time‐dependent variable. In brief, this model switches a patient with recurrent AMI from the initial value of 0 (at the time of the index admission) to a value of 1 at the time of the reinfarction. In this way, the period that patients had survived to the moment of the recurrent AMI was calculated as a survival period without exposure. Patients entered the model from the discharge date of their first AMI (delayed entry) to adjust for any differences in length of hospital stay during periods. Thus, only hospital survivors of the initial admission were included in these analyses.
Hazard ratios were reported as relative risks with 95% confidence intervals (CIs), obtained from the likelihood ratio test. Calculations were made with Statistical Analysis System software, version 8.2 (SAS Institute, Cary, NC).
Ethics
According to Danish law, retrospective register studies do not require ethical approval. The study was approved by the Danish Data Protection Agency.
Results
A total of 168 013 patients had a first AMI between 1985 and 2002. Of these, 1518 patients with an in‐hospital stay exceeding 60 days were excluded and 23 patients were excluded due to missing values. Thus, 166 472 patients (99.1%) were included in the analyses. During the 19‐year follow‐up, 14 123 (8.4%) patients developed a recurrent AMI within the first year after admission for the index AMI.
Demographics of study population and patients with a recurrent AMI
Patients with recurrent AMI were slightly older than patients with first AMI, and age increased by 3 years during the study period. Additionally, more patients with recurrent AMI were male (table 1). Median length of hospital stay decreased by 3 days over the years for patients with first AMI and by 5 days for patients with recurrent AMI. The 1‐year incidence of recurrent AMI did not change significantly with time. However, the incidence of early recurrent AMI increased with periods, while the opposite was true for late recurrent AMI (p<0.001).
Table 1 Demographics in relation to first AMI and recurrent AMI.
| Type of AMI | Period | ||||
|---|---|---|---|---|---|
| 1985–1989 | 1990–1994 | 1995–1999 | 2000–2002 | p Value | |
| First AMI | n = 50 513 | n = 47 721 | n = 40 976 | n = 27 262 | |
| Mean age, year (SD) | 68.2 (11.7) | 68.8 (11.9) | 68.9 (12.6) | 69.6 (13.0) | <0.001 |
| Male sex, % | 65.3 | 64.0 | 63.3 | 62.3 | <0.001 |
| Length of hospital stay, days* | 10 (6–14) | 8 (5–10) | 7 (5–9) | 7 (5–10) | <0.001 |
| Recurrent AMI | n = 4219 | n = 4286 | n = 3010 | n = 2608 | |
| Incidence at 1 year (%) | 8.4 | 9.0 | 7.4 | 9.6 | 0.12 |
| Early recurrent AMI, n (%) | 1014 (2.0) | 1348 (2.8) | 1010 (2.5) | 1044 (3.8) | <0.001 |
| Late recurrent AMI, n (%) | 3205 (6.3) | 2938 (6.1) | 2000 (4.9) | 1564 (5.7) | <0.001 |
| Mean age, year (SD) | 66.9 (11.4) | 68.1 (11.6) | 69.4 (12.3) | 70.1 (12.3) | <0.001 |
| Male sex, % | 67.5 | 67.8 | 69.5 | 70.5 | 0.004 |
| Length of hospital stay, days* | 12 (5–16) | 9 (5–11) | 7 (6–10) | 7 (5–10) | <0.001 |
Recurrent AMI, recurrence within first year after initial AMI; early recurrent AMI, recurrence from 5 to 30 days after first AMI; late recurrent AMI, recurrence from 31 to 365 days after first AMI.
*Values are median (25% and 75% percentiles).
One‐year case‐fatality after admission from first AMI and first recurrent AMI
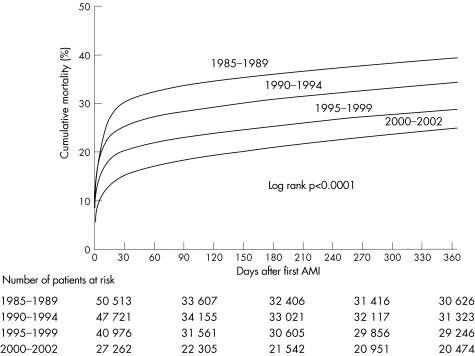
The cumulative 1‐year case‐fatality following a first AMI decreased from 39% in 1985–1989 to 25% in 2000–2002 (fig 1).
Figure 1 Unadjusted cumulative 1‐year case‐fatality after admission from first AMI stratified by period.
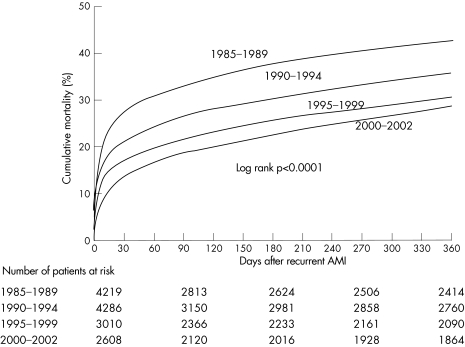
The corresponding 30‐day case‐fatality declined from 30% to 15%. Most of this decline was due to a decrease in in‐hospital case‐fatality from 29% in 1985–1989 to 14% in 2000–2002 (data not shown). A similar decline in case‐fatality was seen in patients with a recurrent AMI. One‐year case‐fatality was 43% in 1985–1989 and 29% in 2000–2002 (fig 2); 30‐day case‐fatality decreased from 28% to 14% in the same periods. The age‐ and sex‐adjusted relative risk of death after first AMI was 0.50 (95% CI: 0.49 to 0.51) in 2000–2002 with years 1985–1989 as reference; the corresponding relative risk after recurrent AMI was 0.48 (95% CI: 0.44 to 0.53).
Figure 2 Unadjusted cumulative 1‐year case‐fatality after admission from first recurrent AMI stratified by period.
One‐year case‐fatality after early and late recurrent AMI
Early occurring recurrent AMIs had a more pronounced reduction in case‐fatality compared to later reinfarctions with crude 1‐year case‐fatality of 46% in 1985–1989, 33% in 1990–1994, 28% in 1995–1999 and 19% in 2000–2002. For late reinfarctions, 1‐year case‐fatality was 42% in 1985–1989, 37% in 1990–1994, 32% in 1995–1999 and 35% in 2000–2002. After age‐ and sex‐adjustment, the relative risk of case‐fatality after early recurrent AMI was 0.33 (95% CI: 0.28 to 0.39) in 2000–2002 compared to 1985–1989; for late recurrent AMI, the corresponding relative risk was 0.58 (95% CI: 0.53 to 0.64). No differences were found in age‐ and sex‐distribution between early and late recurrent AMI.
The prognostic impact of recurrent AMI in hospital survivors of first AMI
Table 2 shows the relative risk of 1‐year case‐fatality associated with recurrent AMI during 1985–2002. The reference group is hospital survivors without reinfarction who survived to the time of reinfarction in the compared group. A recurrent AMI carried a poor prognosis in 1985–1989, but prognosis improved over time. For early recurrent AMIs there was a 72% decrease in relative risk of death; for late recurrent AMIs the risk was reduced by approximately 50%. Note that the exact values of relative risks between groups of recurrent AMIs (early or late) cannot be compared; only the relative reduction in risk is comparable. This is due to the reduced risk of mortality in the reference group with elapsed time from the initial infarction. Patients without a recurrent AMI from 31 to 365 days would be at less risk of dying because they have already survived the critical first month. Therefore, the relative risk of case‐fatality is considerably higher with later recurrent AMIs.
Table 2 Relative risk of sex‐ and age‐adjusted 1‐year case‐fatality mortality after a first AMI among patients with a recurrent AMI compared to hospital survivors without a recurrent AMI during 1985–2002.
| Risk group | Period | |||
|---|---|---|---|---|
| 1985–1989 | 1990–1994 | 1995–1999 | 2000–2002 | |
| No re‐AMI day 5–30* | ||||
| Patients, n | 34 781 | 34 877 | 32 208 | 22 508 |
| Deaths, n | 4752 | 4495 | 3729 | 2899 |
| Re‐AMI day 5–30 | ||||
| Patients, n | 1014 | 1348 | 1010 | 1044 |
| Deaths, n | 462 | 446 | 279 | 203 |
| RR* (95% CI) | 7.5 (6.9 to 8.5) | 4.8 (4.3 to 5.2) | 3.2 (2.8 to 3.6) | 2.1 (1.9 to 2.5) |
| No re‐AMI day 5–365* | ||||
| Patients, n | 30 652 | 31 043 | 29 418 | 20 366 |
| Deaths, n | 2633 | 2667 | 2398 | 1871 |
| Late recurrent AMI day 31–365 | ||||
| Patients, n | 3205 | 2938 | 2000 | 1564 |
| Deaths, n | 1195 | 932 | 541 | 450 |
| RR (95% CI)† | 11.7 (11.0 to 12.4) | 8.5 (8.0 to 9.1) | 6.3 (5.8 to 6.9) | 5.6 (5.1 to 6.2) |
Numbers of deaths in each category of patients during first year are shown.
RR, relative risk; CI, confidence interval.
*Reference group for early recurrent AMI is hospital survivors after first AMI without a recurrent AMI during the first 30 days after index admission; †reference group for late recurrent AMI is hospital survivors who where alive 30 days after admission, and without a recurrent AMI during the first year after admission. Adjustment was made for sex and age.
Discussion
The present study confirms that the prognosis of myocardial infarction has improved considerably during the last two decades and demonstrates that this improvement extends to patients with a recurrent AMI.
One‐year incidence of recurrent AMI
One of the goals in the treatment of patients with AMI is to prevent the occurrence of a new infarction. Apparently, this goal is still elusive as evidenced by the disappointingly steady 1‐year reinfarction rate which remains at approximately 9.6%. With the publication of new criteria for the diagnosis of AMI in Europe and the United States, approximately 26% more patients will be diagnosed as having AMI as compared with the previously used WHO criteria.13 In previous studies the 1‐year incidence of recurrent AMI among patients who have survived the hospital phase of AMI varied from 6–7% in the 1980s1,2,3,14 to approximately 2–4% in 1998–200l after the introduction of modern invasive and non‐invasive therapies.15,16,17 All these studies used the previous WHO definition of AMI. We did not observe any significant increase in the rate of reinfarction over the years, although reinfarction rates were highest in 2000–2002. The higher rates of recurrent AMI in our study compared to others probably reflect the non‐selected character of the study population which included all hospitalised patients with a first AMI in Denmark. By using only primary discharge diagnoses, it is possible that admissions might have been coded as, for instance, primary heart failure or unstable angina. The sensitivity of an AMI diagnosis increased only slightly by adding secondary diagnoses (from 93% to 97% for definite nonfatal AMI, from 65% to 68% for possible nonfatal AMI and from 56% to 72% for fatal definite AMI). However, the majority of diagnoses (86%) were coded as primary AMI.12
Case‐fatality after first and recurrent AMI
The relative decrease in 1‐year case‐fatality was about 50% for both a first and a recurrent AMI during 1985–2002. Notably, not only the trend but also the crude 1‐year case‐fatality of patients with recurrent AMI were remarkably similar to those of patients with first AMI (figs 1 and 2). This paradoxical finding can best be explained by the fact that patients with recurrent AMI are hospital survivors of AMI and therefore represent a selected group of patients. The decrease in crude case‐fatality after a first and recurrent AMI is consistent with findings from other population‐based studies.18,19,20,21,22 Similar, the prognostic impact after a recurrent AMI weakened during the study period. Patients with early reinfarction in 1985–1989 had a 1‐year case‐fatality that was 7.5 times higher than that of patients without reinfarction. In 2000–2002, this ratio had declined to 2.1. A decline, though less pronounced, was also seen in patients with late occurring reinfarctions.
In studies conducted before the 1990s, the relative risk of dying within the first year was around 5–6 in patients with recurrent AMI compared to patients without reinfarction.2,3,4 We found a higher risk of death in this unselected population, which might also have been caused by the limited adjustment for other factors that affect the prognosis after AMI. As no studies in recent years have extended follow‐up to 1 year after reinfarction (occurring within the first year), we are unable to compare our findings from the latest period, but in‐hospital recurrence has been associated with a relative risk of death of 2–4 during the first year after the event.23,24 Only one previous study has specifically investigated the trend in 1‐year mortality from a recurrent AMI.25 Based on an unselected population of 1415 patients with recurrent AMI in 1981–1983 and 1093 patients in 1992–1996, Shotan et al found a reduction in crude 1‐year case‐fatality from 39% in 1981–1983 to 26% in 1992–1996, which is in accordance with our findings.
There are a number of reasons for this change in the prognostic significance of a recurrent AMI. These factors extend from improvement in medical therapy and prophylaxis, and altered patient behaviour through primary care physician referral to emergency rooms, as well as changes in coding practice. New diagnostic criteria and a lower threshold for hospital admission of patients with chest pain may lead to the diagnosis of additional patients with smaller and less serious infarctions. However, in a previous study Abildstrom et al investigated the impact of troponin use in the same population and found that the decline in case‐fatality from a first AMI during 1995–2002 was unaffected by the introduction of troponins.26 This is in accordance with most other studies, which have demonstrated an even higher mortality among the additional patients identified by troponins.27,28 Therefore, it is unlikely that the decline in case‐fatality presented in our paper is simply caused by changes in AMI definitions over the years. It is noteworthy that most of the reduction in case‐fatality was achieved during the early period after recurrent AMI, indicating a more aggressive treatment during hospitalisation and in the early phase after hospitalisation. The health care system in Denmark is comparable to that in other western countries; however, the level of revascularisations was among the lowest in the early 1990s.29 In 1993 a national heart plan was introduced to increase the frequency of invasive procedures and in 2001 rates of revascularisation were comparable to those in the rest of Europe.30 Unfortunately, the use of percutaneous coronary intervention (PCI) was coded infrequently in the National Patient Registry before 1999, but in 2002 the rate of PCI performed during the first week after admission was 21.4% among patients with first AMI who experienced a later reinfarction.
Study strengths and limitations
Administrative registers have the advantage that numbers can become large, and the disadvantage that data are limited. Due to the large population we avoided pooling of data from several years, which allowed us to investigate trends over time. Furthermore, the population was unselected and thus our results are not limited to a certain category of AMI patients. However, this study has some limitations. We had no access to clinical variables or risk factors and therefore no information was provided regarding mechanism of death, pathophysiological explanations of the observed findings, or case severity of first and recurrent AMI. However, the aim of the study was to describe the combined impact of time and diagnostic criteria on the prognostic importance of a recurrent AMI, and in this respect administrative registers are the only option. Other limitations include the use of a 5‐day cut‐point for readmissions. As the length of hospital stay decreased significantly during the study period, this may have introduced bias because fewer reinfarctions would have been identified in early periods. If early reinfarctions where unrecognised due to longer hospitals stay, this would tend to increase case‐fatality in the non‐reinfarction group, and thereby reduce the decline in case‐fatality after reinfarction over the years.
Furthermore, we were unable to register recurrent AMIs occurring during the initial hospitalisation or AMI occurring during revascularisation. Accordingly, periprocedural AMI might appear in our data, but only if the AMI was considered the main medical diagnosis as we only used the primary discharge diagnosis in this study. Finally, different thresholds for hospitalisation of patients with suspected AMI over the years may be a confounding factor.
Conclusion
During the latest two decades the decline in case‐fatality after a recurrent AMI was similar to the decline in case‐fatality after a first AMI. Recurrent AMI remained a significant predictor of death despite changes in AMI diagnostic criteria, but the prognostic impact has weakened over the years indicating a shift towards a better prognosis.
Abbreviations
AMI - acute myocardial infarction
ICD - International Classification of Diseases
PCI - percutaneous coronary intervention
Footnotes
Financial support: This study was supported by a grant from the Danish Heart Foundation (grant number 04‐10‐B76‐A217‐22196).
Competing interest: None.
References
- 1.Dwyer E M, Jr, McMaster P, Greenberg H. Nonfatal cardiac events and recurrent infarction in the year after acute myocardial infarction. J Am Coll Cardiol 19844695–702. [DOI] [PubMed] [Google Scholar]
- 2.Benhorin J, Moss A J, Oakes D. Prognostic significance of nonfatal myocardial reinfarction. Multicenter Diltiazem Postinfarction Trial Research Group. J Am Coll Cardiol 199015253–258. [DOI] [PubMed] [Google Scholar]
- 3.Kornowski R, Goldbourt U, Zion M.et al Predictors and long‐term prognostic significance of recurrent infarction in the year after a first myocardial infarction. SPRINT Study Group. Am J Cardiol 199372883–888. [DOI] [PubMed] [Google Scholar]
- 4.Mueller H S, Forman S A, Menegus M A.et al Prognostic significance of nonfatal reinfarction during 3‐year follow‐up: results of the Thrombolysis in Myocardial Infarction (TIMI) phase II clinical trial. The TIMI Investigators. J Am Coll Cardiol 199526900–907. [DOI] [PubMed] [Google Scholar]
- 5.Capewell S, Livingston B M, MacIntyre K.et al Trends in case‐fatality in 117 718 patients admitted with acute myocardial infarction in Scotland. Eur Heart J 2000211833–1840. [DOI] [PubMed] [Google Scholar]
- 6.Tunstall‐Pedoe H, Kuulasmaa K, Mahonen M.et al Contribution of trends in survival and coronary‐event rates to changes in coronary heart disease mortality: 10‐year results from 37 WHO MONICA project populations. Monitoring Trends and Determinants in Cardiovascular Disease. Lancet 19993531547–1557. [DOI] [PubMed] [Google Scholar]
- 7. Myocardial infarction redefined–a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the Redefinition of Myocardial Infarction. Eur Heart J 2000211502–1513. [DOI] [PubMed] [Google Scholar]
- 8. Invasive compared with non‐invasive treatment in unstable coronary‐artery disease: FRISC II prospective randomised multicentre study. FRagmin and Fast Revascularisation during InStability in Coronary artery disease Investigators. Lancet 1999354708–715. [PubMed] [Google Scholar]
- 9.Yusuf S, Zhao F, Mehta S R.et al Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST‐segment elevation. N Engl J Med 2001345494–502. [DOI] [PubMed] [Google Scholar]
- 10.Andersen H R, Nielsen T T, Rasmussen K.et al A comparison of coronary angioplasty with fibrinolytic therapy in acute myocardial infarction. N Engl J Med 2003349733–742. [DOI] [PubMed] [Google Scholar]
- 11.Andersen T F, Madsen M, Jorgensen J.et al The Danish National Hospital Register. A valuable source of data for modern health sciences. Dan Med Bull 199946263–268. [PubMed] [Google Scholar]
- 12.Madsen M, Davidsen M, Rasmussen S.et al The validity of the diagnosis of acute myocardial infarction in routine statistics: a comparison of mortality and hospital discharge data with the Danish MONICA registry. J Clin Epidemiol 200356124–130. [DOI] [PubMed] [Google Scholar]
- 13.Trevelyan J, Needham E W, Smith S C.et al Impact of the recommendations for the redefinition of myocardial infarction on diagnosis and prognosis in an unselected United Kingdom cohort with suspected cardiac chest pain. Am J Cardiol 200493817–821. [DOI] [PubMed] [Google Scholar]
- 14.Gilpin E, Ricou F, Dittrich H.et al Factors associated with recurrent myocardial infarction within one year after acute myocardial infarction. Am Heart J 1991121457–465. [DOI] [PubMed] [Google Scholar]
- 15.Dangas G, Aymong E D, Mehran R.et al Predictors of and outcomes of early thrombosis following balloon angioplasty versus primary stenting in acute myocardial infarction and usefulness of abciximab (the CADILLAC trial). Am J Cardiol 200494983–988. [DOI] [PubMed] [Google Scholar]
- 16.Fernandez‐Aviles F, Alonso J J, Castro‐Beiras A.et al Routine invasive strategy within 24 hours of thrombolysis versus ischaemia‐guided conservative approach for acute myocardial infarction with ST‐segment elevation (GRACIA‐1): a randomised controlled trial. Lancet 20043641045–1053. [DOI] [PubMed] [Google Scholar]
- 17.Steffenino G, Santoro G M, Maras P.et al In‐hospital and one‐year outcomes of patients with high‐risk acute myocardial infarction treated with thrombolysis or primary coronary angioplasty. Ital Heart J 20045136–145. [PubMed] [Google Scholar]
- 18.Rosamond W D, Chambless L E, Folsom A R.et al Trends in the incidence of myocardial infarction and in mortality due to coronary heart disease, 1987 to 1994. N Engl J Med 1998339861–867. [DOI] [PubMed] [Google Scholar]
- 19.McGovern P G, Jacobs D R, Jr, Shahar E.et al Trends in acute coronary heart disease mortality, morbidity, and medical care from 1985 through 1997: the Minnesota heart survey. Circulation 200110419–24. [DOI] [PubMed] [Google Scholar]
- 20.Marques‐Vidal P, Ruidavets J B, Cambou J P.et al Incidence, recurrence, and case fatality rates for myocardial infarction in southwestern France, 1985 to 1993. Heart 200084171–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Messner T, Lundberg V, Bostrom S.et al Trends in event rates of first and recurrent, fatal and non‐fatal acute myocardial infarction, and 28‐day case fatality in the Northern Sweden MONICA area 1985–98. Scand J Public Health 20036151–59. [DOI] [PubMed] [Google Scholar]
- 22.Salomaa V, Miettinen H, Kuulasmaa K.et al Decline of coronary heart disease mortality in Finland during 1983 to 1992: roles of incidence, recurrence, and case‐fatality. The FINMONICA MI Register Study. Circulation 1996943130–3137. [DOI] [PubMed] [Google Scholar]
- 23.Hudson M P, Granger C B, Topol E J.et al Early reinfarction after fibrinolysis: experience from the global utilization of streptokinase and tissue plasminogen activator (alteplase) for occluded coronary arteries (GUSTO I) and global use of strategies to open occluded coronary arteries (GUSTO III) trials. Circulation 20011041229–1235. [DOI] [PubMed] [Google Scholar]
- 24.Gibson C M, Karha J, Murphy S A.et al Early and long‐term clinical outcomes associated with reinfarction following fibrinolytic administration in the Thrombolysis in Myocardial Infarction trials. J Am Coll Cardiol 2003427–16. [DOI] [PubMed] [Google Scholar]
- 25.Shotan A, Gottlieb S, Goldbourt U.et al Prognosis of patients with a recurrent acute myocardial infarction before and in the reperfusion era‐‐a national study. Am Heart J 2001141478–484. [DOI] [PubMed] [Google Scholar]
- 26.Abildstrom S Z, Rasmussen S, Madsen M. Changes in hospitalization rate and mortality after acute myocardial infarction in Denmark after diagnostic criteria and methods changed. Eur Heart J 200426990–995. [DOI] [PubMed] [Google Scholar]
- 27.Pell J P, Simpson E, Rodger J C.et al Impact of changing diagnostic criteria on incidence, management, and outcome of acute myocardial infarction: retrospective cohort study. BMJ 2003326134–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Meier M A, Al‐Badr W H, Cooper J V.et al The new definition of myocardial infarction: diagnostic and prognostic implications in patients with acute coronary syndromes. Arch Intern Med 20021621585–1589. [DOI] [PubMed] [Google Scholar]
- 29. Technological change around the world: evidence from heart attack care. Health Aff (Millwood) 20012025–42. [DOI] [PubMed] [Google Scholar]
- 30.Togni M, Balmer F, Pfiffner D.et al Percutaneous coronary interventions in Europe 1992–2001. Eur Heart J 2004251208–1213. [DOI] [PubMed] [Google Scholar]