Patients with ST‐elevation myocardial infarction (STEMI) and prior coronary artery bypass grafting (CABG) constitute a subgroup at high risk for morbidity and mortality compared with patients with STEMI without prior CABG. Primary percutaneous coronary intervention (PCI) has become the preferred treatment for patients with STEMI. It has been shown that, in patients with STEMI with prior CABG treated with primary PCI, treatment of a saphenous vein graft (SVG) is a more important predictor of outcome than a history of CABG alone.1,2,3 Primary PCI for SVG occlusion is associated with poor procedural results and poor short‐ and long‐term outcomes.3 The time to occurrence of STEMI due to SVG occlusion after CABG is unknown. Furthermore, it is unclear whether time from CABG affects the outcome of mechanical reperfusion for SVG occlusion. We evaluated the time from CABG to occurrence of STEMI due to SVG occlusion. Moreover, immediate angiographic outcome and 1‐year mortality stratified to graft age after primary PCI for SVG occlusion were studied.
Methods
Between January 1997 and March 2005, 3038 consecutive and unselected patients were treated for STEMI with primary PCI. A total of 37 (1.2%) patients were admitted with STEMI due to SVG occlusion and represent the study population. PCI was performed using standard techniques. All patients were treated with heparin and aspirin before PCI. The use of abciximab was left to the operators' discretion. Follow‐up information was obtained 1 year after the initial event by written questionnaire sent to all patients. If necessary, outpatients' reports were reviewed and general practitioners were contacted by telephone. Baseline clinical and angiographic data were collected prospectively in a dedicated database. After exact determination of SVG age in all patients, we stratified the patients for time from CABG to STEMI due to SVG occlusion into two groups: group 1 <10 years and group 2 >10 years. Left ventricular function was determined by echocardiography within 1 week after primary PCI. Statistical analysis was performed using SPSS V.12.0. Differences in variables (clinical, angiographic and outcome) were tested by the χ2 test. Significance was defined as p <0.05.
Results
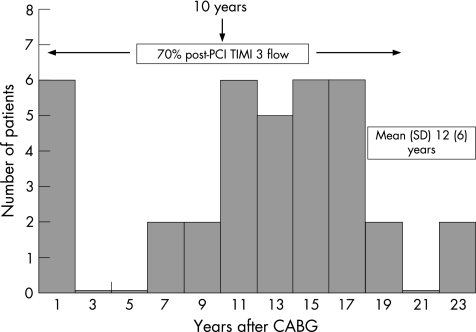
The mean (SD) time from CABG to the index STEMI in patients treated with primary PCI for SVG occlusion was 12 (6) years. From the 37 patients with STEMI due to an SVG occlusion, 27 (73%) patients presented >10 years after CABG. A total of ten (27%) patients had an acute SVG occlusion <10 years after CABG, of which six occurred within 1 year after CABG (fig 1). There were no differences in clinical and angiographic characteristics between patients presenting <10 years after CABG and patients presenting >10 years after CABG (table 1). Abciximab was used during PCI in 65% of all patients. The incidence of post‐PCI TIMI (thrombolysis in myocardial infarction) 3 flow was comparable in both groups (70% vs 70%, p = 0.98). The overall 1‐year mortality was 19%. In all, one (10%) patient died in group 1 compared with six (22%) patients in group 2 (p = 0.4).
Figure 1 ST‐elevation myocardial infarction due to saphenous vein graft (SVG) occlusion according to SVG age. CABG, coronary artery bypass grafting; PCI, percutaneous coronary intervention; TIMI, thrombolysis in myocardial infarction.
Table 1 Characteristics and outcome of 37 patients with ST‐elevation myocardial infarction due to saphenous vein graft occlusion treated with primary percutaneous coronary intervention.
| Saphenous vein graft age | ||||
|---|---|---|---|---|
| <10 years (n = 10) | >10 years (n = 27) | p Value | ||
| n (%) | n (%) | |||
| Clinical | ||||
| Age >60 years | 9 (90) | 21 (78) | NS | |
| Men | 9 (90) | 25 (93) | NS | |
| Hypertension | 3 (30) | 8 (30) | NS | |
| Smoker | 0 (0) | 7 (26) | NS | |
| Diabetes mellitus | 3 (30) | 5 (19) | NS | |
| Dyslipidaemia | 5 (50) | 12 (44) | NS | |
| Family history | 0 (0) | 6 (22) | NS | |
| Aspirin | 8 (80) | 23 (85) | NS | |
| β‐blocker | 5 (50) | 17 (63) | NS | |
| Previous MI | 6 (60) | 16 (59) | NS | |
| Previous PCI | 4 (40) | 11 (41) | NS | |
| Shock | 3 (30) | 7 (26) | NS | |
| Angiographic | ||||
| Three‐vessel disease | 8 (80) | 22 (82) | NS | |
| Pre‐PCI TIMI 0 | 7 (70) | 20 (74) | NS | |
| Abciximab | 8 (80) | 16 (59) | NS | |
| Thrombosuction | 4 (40) | 8 (30) | NS | |
| Distal protection device | 0 (0) | 3 (11) | NS | |
| IABP | 4 (40) | 6 (22) | NS | |
| Outcome | ||||
| Post‐PCI TIMI 3 | 7 (70) | 19 (70) | NS | |
| LVEF <40%* | 6 (75) | 15 (68) | NS | |
| 1‐year mortality | 1 (10) | 6 (22) | NS | |
| 1‐year mortality | ||||
IABP, intra‐aortic balloon counterpulsation; LVEF, left ventricular ejection fraction; MI, myocardial infarction; NS, not significant; PCI, percutaneous coronary intervention; STEMI, ST‐elevation myocardial infarction; SVG, saphenous vein graft; TIMI, thrombolysis in myocardial infarction.
*Measured in 30 patients.
Discussion
This study reports two novel findings on primary PCI for STEMI due to SVG occlusion. Firstly, our data show that patients with STEMI due to SVG occlusion present either “early” or “late”. Of the patients presenting <10 years after CABG, most of the acute SVG occlusions occur within the first year after CABG. As a second finding, we report equal angiographic success rates and comparable 1‐year mortality in patients treated with primary PCI for acute SVG occlusion with regard to time from bypass surgery. No difference in outcome was observed in patients presenting either <10 or >10 years after CABG. Thus, time from CABG does not affect outcome in patients with prior CABG treated with primary PCI for STEMI due to SVG occlusion.
The patient characteristics in our study of primary PCI for STEMI due to SVG occlusion are consistent with other studies. It has been described that angiographic outcome and 1‐year mortality are worse after primary PCI for acute SVG occlusion compared with primary PCI for acute native coronary artery occlusion.1,2,3 Patients with acute SVG occlusion have a higher baseline risk profile with more advanced age, more previous myocardial infarction and more severe coronary artery disease. In our study, 25–30% of patients presented in shock and the rate of TIMI 3 flow after primary PCI for SVG occlusion was 70%, which is in agreement with prior studies.
The mechanism of early graft failure (<1 year) is mainly graft thrombosis and/or intimal hyperplasia, whereas in late graft failure this is progressive atherosclerosis, often with superimposed thrombus.4 Occlusion of a leads SVG to stasis and thrombus formation. As a result, the large thrombotic burden markedly complicates the recanalisation of an occluded SVG. Thus, regardless of graft age, mechanical reperfusion is often complicated by distal embolisation and no reflow, which is associated with a higher short‐ and long‐term mortality.1,2,3 In elective patients with PCI treated for SVG disease, the Saphenous vein‐graft Angiopathy Free of Emboli Randomized Trial showed significant improvement of angiographic outcome (TIMI 3 flow and no reflow), resulting in a reduction in myocardial infarctions, with the use of a distal embolic protection device compared with standard techniques.5 Interestingly, a substudy of this trial showed that SVG age was not a predictor of clinical outcome, as in our study on patients with STEMI. Whether the beneficial effects of such devices also apply for patients with STEMI due to SVG occlusion is unclear.
Although the absolute number of patients in this study is relatively small, it represents one of the largest single‐centre cohorts. Other reports often consider pooled data over a longer period of time.
In conclusion, patients with STEMI due to SVG occlusion present either “early” or “late” after CABG. For the patients presenting <10 years after CABG, most of the acute SVG occlusions occur within 1 year after CABG. Most patients with STEMI due to SVG occlusion present >10 years after CABG. Although different mechanisms may play a role, outcome is comparable between patients with STEMI due to SVG occlusion <10 years and >10 years after CABG treated with primary PCI, with an equal angiographic success rate and a non‐significantly different 1‐year mortality.
Abbreviations
CABG - coronary artery bypass grafting
PCI - percutaneous coronary intervention
SVG - saphenous vein graft
STEMI - ST‐elevation myocardial infarction
TIMI - thrombolysis in myocardial infarction
Footnotes
Competing interests: None.
References
- 1.Al Suwaidi J, Velianou J L, Berger P B.et al Primary percutaneous coronary interventions in patients with acute myocardial infarction and prior coronary artery bypass grafting. Am Heart J 2001142452–459. [DOI] [PubMed] [Google Scholar]
- 2.Nguyen T T, O'Neill W W, Grines C L.et al One‐year survival in patients with acute myocardial infarction and a saphenous vein graft culprit treated with primary angioplasty. Am J Cardiol 2003911250–1254. [DOI] [PubMed] [Google Scholar]
- 3.Brodie B R, VerSteeg D S, Brodie M M.et al Poor long‐term patient and graft survival after primary percutaneous coronary intervention for acute myocardial infarction due to saphenous vein graft occlusion. Catheter Cardiovasc Interv 200565504–509. [DOI] [PubMed] [Google Scholar]
- 4.Motwani J G, Topol E J. Aortocoronary saphenous vein graft disease: pathogenesis, predisposition, and prevention. Circulation 199897916–931. [DOI] [PubMed] [Google Scholar]
- 5.Baim D S, Wahr D, George B.et al Randomized trial of a distal embolic protection device during percutaneous intervention of saphenous vein aorto‐coronary bypass grafts. Circulation 20021051285–1290. [PubMed] [Google Scholar]