Abstract
Objective
To determine whether rapid access chest pain clinics are clinically effective by comparison of coronary event rates in patients diagnosed with angina with rates in patients diagnosed with non‐cardiac chest pain and the general population.
Design
Multicentre cohort study of consecutive patients with chest pain attending the rapid access chest pain clinics (RACPCs) of six hospitals in England.
Participants
8762 patients diagnosed with either non‐cardiac chest pain (n = 6396) or incident angina without prior myocardial infarction (n = 2366) at first cardiological assessment, followed up for a median of 2.57 (interquartile range 1.96–4.15) years.
Main outcome measures
Primary end point—death due to coronary heart disease (International Classification of Diseases (ICD)10 I20–I25) or acute coronary syndrome (non‐fatal myocardial infarction (ICD10 I21–I23), hospital admission with unstable angina (I24.0, I24.8, I24.9)). Secondary end points—all‐cause mortality (ICD I20), cardiovascular death (ICD10 I00–I99), or non‐fatal myocardial infarction or non‐fatal stroke (I60–I69).
Results
The cumulative probability of the primary end point in patients diagnosed with angina was 16.52% (95% confidence interval (CI) 14.88% to 18.32%) after 3 years compared with 2.73% (95% CI 2.29% to 3.25%) in patients with non‐cardiac chest pain. Coronary standardised mortality ratios for men and women with angina aged <65 years were 3.52 (95% CI 1.98 to 5.07) and 4.39 (95% CI 1.14 to 7.64). Of the 599 patients who had the primary end point, 194 (32.4%) had been diagnosed with non‐cardiac chest pain. These patients were younger, less likely to have typical symptoms, more likely to be south Asian and more likely to have a normal resting electrocardiogram than patients with angina who had the primary end point.
Conclusion
RACPCs are successful in identifying patients with incident angina who are at high coronary risk, but there is a need to reduce misdiagnosis and improve outcomes in patients diagnosed with non‐cardiac chest pain who accounted for nearly one third of cardiac events during follow‐up.
Angina is the most common initial manifestation of coronary heart disease1,2,3 and accounts for an estimated 1% of annual health expenditure in the UK.4 Rapid access chest pain clinics (RACPCs) are now widely established on the basis of the assumption that one‐stop cardiological assessment can successfully identify patients with angina who are considered to be at high risk of adverse cardiovascular outcomes. It is implicit in this that patients diagnosed with non‐cardiac chest pain can be safely excluded from further cardiac investigation and treatment. However, the validity of this assumption is unknown because the prognosis of incident angina and non‐cardiac chest pain in patients with previously undiagnosed symptoms has not been defined. Previous studies have been limited by small size and short periods of follow‐up.5,6,7,8 We have studied the prognosis of a large cohort of patients referred from primary care with chest pain, none of whom had had previous cardiological assessment. Our primary objective was to assess the clinical effectiveness of RACPCs by determining the extent to which diagnoses of angina and non‐cardiac chest pain validate the prognostic assumptions that have led to their widespread introduction in the UK.
Methods
Patients
Consecutive patients attended six RACPCs in which cardiological consultation was provided within 2 weeks of referral from primary care according to the imperatives of the UK National Service Framework for coronary heart disease.9 The purpose of the clinics was to identify patients with angina to initiate appropriate treatment, including secondary prevention with aspirin and β‐blockers, and to carry out cholesterol measurement with a view to starting statin treatment, according to contemporary guidelines.10 Data on 11082 patients were electronically recorded from 2 January 1996 to 31 December 2002 using identical databases, details of which have been reported previously.11 We excluded re‐attendances during the study period (n = 448), patients without chest pain (n = 291), patients diagnosed with acute coronary syndromes on the day of visit (n = 246), patients who reported previously diagnosed coronary heart disease or revascularisation procedure (n = 579), patients for whom a diagnosis was either not entered (n = 132) or not identified as angina or non‐cardiac chest pain (n = 83), those with undefined ethnic group (n = 134), patients with missing data (n = 367) and those who were not traced by the Office for National Statistics12 or the NHS‐wide clearing system13 (n = 40). The remaining 8762 patients with complete data and follow‐up constituted the study group.
Data collection
Clinical data were systematically recorded and included age, sex, ethnicity, clinical descriptors of chest pain (duration of symptoms before attendance, character, site and radiation of chest pain, duration of an episode, precipitating factors and relief with glyceryl trinitrate), smoking status, history of hypertension, diabetes, pulse rate, systolic blood pressure, drugs and follow‐up plan on discharge. Twelve‐lead resting electrocardiograms (ECGs) were recorded as normal or abnormal, respectively, depending on assessment of rhythm, conduction, and the absence or presence of regional ST segment or T wave changes, left‐ventricular hypertrophy and Q waves. Exercise treadmill tests were carried out at the discretion of clinicians in 58% of patients. Reasons for not carrying out an ECG treadmill test were recorded as follows: resting ECG abnormalities or other comorbidities (16%), not indicated (26%), in whom median probability of coronary artery disease was 18.6% (interquartile range (IQR) 8.4–32.4%). Diagnosis of the cause of chest pain, either angina or non‐cardiac chest pain, was based on the clinical assessment of the clinician who recorded it at the end of the consultation.
Follow‐up
Patients were flagged for mortality with the Office for National Statistics (to 25 April 2005), and for hospital admissions and procedures with the NHS‐wide clearing system (to 23 December 2003). Successful matching was achieved in 99.5% of the cohort. Causes of death were defined by the World Health Organization International Classification of Diseases (ICD10 codes). Among patients undergoing hospital admission during the follow‐up period, the primary discharge diagnosis was used to define events.
Main outcome measures
The primary end point was a composite of death due to coronary heart disease (ICD10 I20–I25) or acute coronary syndrome (non‐fatal myocardial infarction (ICD10 I21–I23) and hospital admission with unstable angina (I24.0, I24.8, I24.9)). Secondary end points were all‐cause mortality (ICD I20), cardiovascular death (ICD10 I00–I99) or non‐fatal myocardial infarction (ICD10 121–123) or hospital admission with unstable angina (I24.0, I24.8, I24.9) or non‐fatal stroke (I60–I69).
Ethical approval
Ethical approval was obtained from the multiregional ethics committee (MREC/02/04/095). Permission was given by the National Patient Information Advisory Group14 to link anonymised datasets without individual patient consent.
Statistical analysis
Patients with angina and non‐cardiac chest pain were compared using χ2 and t tests for proportions and distributions, respectively. We calculated Kaplan–Meier product limits for the cumulative probability of reaching an end point and used the log rank test for evidence of a statistically significant difference between the groups. Time was measured from the first clinic visit to the outcome of interest. Cox regression analysis was used to estimate hazard ratios for the effect of angina on outcome in age‐adjusted and fully adjusted models, based on covariates associated (p<0.05) with the outcome of interest. We used STATA V.8.0 for all the analyses.
Standardised mortality ratios
Standardised mortality ratios (SMRs) were calculated as the ratio of observed mortality within the study group to expected mortality based on data available from the Office for National Statistics. SMRs for all‐cause mortality were calculated for each year of the study, taking into account the exact time each patient was in the study and using 1‐year age bands. The reference death rates were for England for the same year, except for 2003 and 2004, for which the death rates were not available and the 2002 death rates were used. The reference death rates for death due to coronary heart disease and other disease groups are given in 10‐year age blocks, so we used linear interpolation to derive death rates for each year of age. SMRs for coronary heart disease and other disease groups were calculated using the same method as for all‐cause mortality.
Results
Patients
Table 1 summarises the baseline characteristics of patients diagnosed with angina or non‐cardiac chest pain.
Table1 Baseline characteristics among consecutive patients diagnosed with angina or non‐cardiac chest pain, in those who did and did not subsequently experience the primary end point.
| Angina group (n = 2366) | Non‐cardiac group (n = 6396) | |||
|---|---|---|---|---|
| With 1 end point*, n = 405 (17%) | Without 1 end point, n = 1961 (83%) | With 1 end point*, n = 194 (3%) | Without 1 end point*, n = 6202 (97%) | |
| Mean (SD) age (years) | 62 (11) | 62 (11) | 56 (11) | 51 (12) |
| Males | 240 (59%) | 1114 (57%) | 111 (57%) | 3129 (50%) |
| Ethnicity, n (%) | ||||
| White | 298 (74%) | 1512 (77%) | 97 (50%) | 3878 (63%) |
| South Asian | 90 (22%) | 371 (19%) | 84 (43%) | 1694 (27%) |
| Black | 17 (4%) | 78 (4%) | 13 (7%) | 630 (10%) |
| Risk factor, n (%) | ||||
| Current smoker | 92 (23%) | 451 (23%) | 52 (27%) | 1500 (24%) |
| Hypertension | 184 (45%) | 930 (47%) | 76 (39%) | 1855 (30%) |
| Diabetes | 78 (19%) | 315 (16%) | 41 (21%) | 484 (8%) |
| Duration of chest pain†, n (%) | ||||
| <4 weeks | 161 (40%) | 773 (39%) | 112 (58%) | 3148 (51%) |
| 1–⩽6 months | 155 (38%) | 769 (39%) | 50 (26%) | 1978 (32%) |
| >6–12 months | 34 (8%) | 132 (7%) | 7 (4%) | 320 (5%) |
| >1 year | 55 (14%) | 287 (15%) | 25 (13%) | 756 (12%) |
| Character of chest pain, n (%) | ||||
| Typical | 304 (75%) | 1390 (71%) | 17 (9%) | 291 (5%) |
| Atypical | 100 (25%) | 562 (29%) | 128 (66%) | 4289 (69%) |
| Non‐specific | 1 (0.3%) | 9 (0.5%) | 49 (25%) | 1622 (26%) |
| Resting ECG, n (%) | ||||
| Normal | 222 (55%) | 1293 (66%) | 160 (82%) | 5616 (91%) |
| Abnormal | 183 (45%) | 668 (34%) | 34 (18%) | 586 (9%) |
| Exercise treadmill test, n (%) | ||||
| Positive | 152 (38%) | 714 (36%) | 2 (1%) | 23 (0.4%) |
| Non‐diagnostic | 28 (7%) | 217 (11%) | 4 (2%) | 116 (2%) |
| Negative | 77 (19%) | 392 (20%) | 99 (51%) | 3257 (53%) |
| Not done, not indicated | 5 (1%) | 31 (2%) | 63 (33%) | 2218 (36%) |
| Not done, other reason | 143 (35%) | 607 (31%) | 26 (13%) | 588 (10%) |
| Mean (SD) systolic blood pressure (mm Hg) | 148 (21) | 147 (21) | 143 (23) | 138 (20) |
| Heart rate (beats/min) | 77 (13) | 76 (12) | 77 (13) | 77 (12) |
| Medication on discharge, n (%) | ||||
| Aspirin | 347 (86%) | 1650 (84%) | 32 (17%) | 608 (10%) |
| β‐blockers | 212 (52%) | 1061 (54%) | 19 (10%) | 473 (8%) |
| Calcium blockers | 167 (41%) | 740 (38%) | 26 (13%) | 411 (7%) |
| Statin | 113 (28%) | 547 (28%) | 14 (7%) | 395 (6%) |
| Cholesterol measured‡ | 312 (83%) | 1476 (82%) | 121 (71%) | 3558 (65%) |
| Disposal§, n (%) | ||||
| Admitted | 0 | 0 | 1 (0.5%) | 12 (0.2%) |
| Cardiac outpatients | 217 (54%) | 1143 (59%) | 29 (15%) | 670 (11%) |
| Angiography | 115 (29%) | 453 (23%) | 0 | 2 (0.03%) |
| Discharged to primary care | 67 (17%) | 342 (18%) | 163 (85%) | 5475 (89%) |
| intervention | ||||
| Angiogram | 237 (59%) | 587 (30%) | 71 (37%) | 84 (1%) |
| PTCA | 68 (17%) | 134 (7%) | 25 (13%) | 8 (0.1%) |
| CABG | 68 (17%) | 161 (8%) | 15 (8%) | 5 (0.1%) |
| PTCA/CABG | 130 (32%) | 289 (15%) | 39 (20%) | 13 (0.2%) |
CABG, coronary artery bypass graft; ECG, electrocardiogram; PTCA, percutaneous transluminal coronary angioplasty.
*1 (Primary) end point—death due to coronary heart disease or acute coronary syndrome.
†Duration of chest pain before attendance at the clinic.
‡Percentage of patients not prescribed a statin but in whom a cholesterol check was recommended (data available for 7810 patients).
§Data available for 8689 patients.
Patients diagnosed with angina were older and more likely to be men than patients diagnosed with non‐cardiac chest pain. Among patients with angina, 58% were referred for further outpatient cardiological assessment, with a total of 35% undergoing angiography during follow‐up, of whom 43% had a revascularisation procedure. Only 18% were referred back to their primary care physician after a single clinic visit compared with 89% of patients with non‐cardiac chest pain.
Prognosis of angina and non‐cardiac chest pain
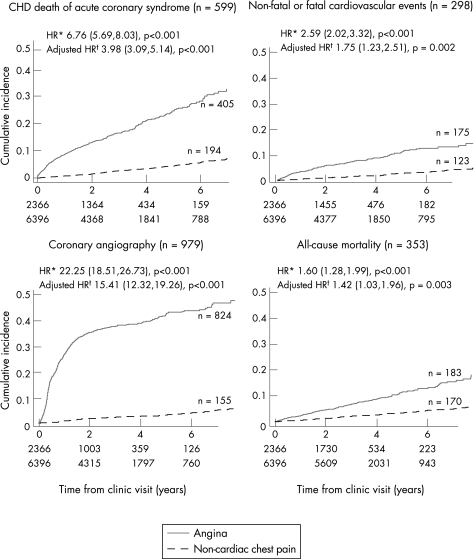
Figure 1 shows the Kaplan–Meier survival curves for patients with and without angina.
Figure 1 Kaplan–Meier survival curves for patients with and without angina. Numbers at risk at beginning of each year of follow‐up are displayed at the bottom of each graph. *Hazard ratio (HR) adjusted for age only. †HR adjusted for sex, age, ethnicity, diabetes, smoking status, heart rate, character of chest pain and resting ECG. CHD, coronary heart disease.
During a median follow‐up of 2.57 (IQR 1.96–4.15) years, all outcomes were more frequent for patients with angina than for patients with non‐cardiac chest pain. In patients with angina, the cumulative probability of the primary end point was 8.62% (95% CI 7.56% to 9.83%) after 1 year, rising to 16.52% (95% CI 14.88% to 18.32%) after 3 years. This compares with cumulative probabilities for the primary end point of 0.83% (95% CI 0.63% to 1.08%) after 1 year and 2.73% (95% CI 2.29% to 3.25%) after 3 years in patients with non‐cardiac chest pain. In the 501 patients with missing baseline data, rates of the primary end point were not significantly different from those in the main cohort.
Predictive accuracy of diagnosis for the primary end point
Among the 599 patients with the primary end point, 194 (32.4%) had been diagnosed with non‐cardiac chest pain. Compared to patients with angina who reached the primary end point (n = 405), those with non‐cardiac chest pain (n = 194) were younger, a higher proportion were south Asians, >80% had normal resting electrocardiograms and a substantially lower proportion had typical symptoms and an abnormal exercise treadmill test. Multivariate associations with the primary end point in patients diagnosed with non‐cardiac chest pain were age, male sex, south Asian ethnicity, diabetes, typical symptoms and abnormal ECG (table 2).
Table 2 Predictors of death due to coronary heart disease or acute coronary syndrome in 6396 patients diagnosed with non‐cardiac chest pain.
| Covariates | CHD death or acute coronary syndrome (n = 194) | |||
|---|---|---|---|---|
| Age‐adjusted* HR (95% CI) | p Value | Adjusted† HR (95% CI) | p Value | |
| Male sex | 1.41 (1.06 to 1.87) | 0.018 | 1.36 (1.02 to 1.81) | 0.033 |
| Age/10‐year increase* | 1.47 (1.32 to 1.65) | <0.000 | 1.46 (1.29 to 1.64) | <0.000 |
| Ethnicity | ||||
| Black v white | 0.63 (0.35 to 1.12) | 0.000 | 0.58 (0.32 to 1.04) | 0.001 |
| SA v white | 1.73 (1.27 to 2.35) | 1.51 (1.10 to 2.08) | ||
| History of hypertension | 1.22 (0.91 to 1.65) | 0.189 | NA | NA |
| Systolic blood pressure | 1.00 (0.99 to 1.01) | 0.747 | NA | NA |
| Current smoking | 1.30 (0.95 to 1.80) | 0.111 | NA | NA |
| Diabetes v none | 2.49 (1.76 to 3.52) | <0.000 | 2.14 (1.49 to 3.09) | 0.000 |
| Symptoms | ||||
| Typical v non‐specific | 2.03 (1.17 to 3.54) | 0.050 | 2.12 (1.21 to 3.70) | 0.040 |
| Atypical v non‐specific | 1.04 (0.75 to 1.45) | 1.07 (0.76 to 1.49) | ||
| Duration of symptoms | 1.01 (0.76 to 1.35) | 0.931 | NA | NA |
| >1 month v ⩽1 month | ||||
| Heart rate, 10 beats/min | 0.97 (0.86 to 1.09) | 0.550 | NA | NA |
| Abnormal ECG result | 1.66 (1.14 to 2.42) | 0.012 | 1.62 (1.10 to 2.36) | 0.0188 |
CHD, coronary heart disease; ECG, electrocardiogram; SA, South Asians.
*Age is univariable.
†Adjusted for all variables in the table apart from history of hypertension, systolic blood pressure, current smoking, duration of symptoms and heart rate.
Comparison with the general population
Table 3 gives the SMRs in patients with angina and non‐cardiac chest pain.
Table 3 Standardised mortality ratios (to April 2004) in patients diagnosed with angina and non‐cardiac chest pain (n = 8762).
| Angina group | Non‐cardiac group | |||||||
|---|---|---|---|---|---|---|---|---|
| Male | Female | Male | Female | |||||
| O/E | SMR (95% CI) | O/E | SMR (95% CI) | O/E | SMR (95% CI) | O/E | SMR (95% CI) | |
| All‐cause mortality | ||||||||
| < 65 | 40/23 | 1.83 (1.26 to 2.39) | 20/11 | 1.78 (1.00 to 2.56) | 54/54 | 1.00 (0.73 to 1.26) | 44/36 | 1.21 (0.85 to 1.57) |
| ⩾65 | 79/91 | 0.87 (0.68 to 1.05) | 45/53 | 0.85 (0.60 to 1.09) | 46/63 | 0.73 (0.52 to 0.94) | 26/51 | 0.51 (0.32 to 0.71) |
| All ages | 119/113 | 1.05 (0.86 to 1.24) | 65/64 | 1.01 (0.76 to 1.25) | 100/117 | 0.85 (0.68 to 1.02) | 70/88 | 0.80 (0.61 to 0.98) |
| CHD (ICD 10 I20–I25) | ||||||||
| <65 | 20/6 | 3.52 (1.98 to 5.07) | 7/2 | 4.39 (1.14 to 7.64) | 15/13 | 1.15 (0.57 to 1.73) | 9/5 | 1.96 (0.68 to 3.24) |
| ⩾65 | 35/27 | 1.62 (1.09 to 2.16) | 18/10 | 1.76 (0.95 to 2.58) | 11/16 | 0.71 (0.29 to 1.12) | 3/10 | 0.31 (0.00 to 0.65) |
| All ages | 55/28 | 2.03 (1.49 to 2.56) | 25/12 | 2.13 (1.29 to 2.96) | 26/26 | 0.92 (0.57 to 1.28) | 12/15 | 0.85 (0.37 to 1.32) |
| Non‐cardiovascular causes | ||||||||
| <65 | 15/14 | 1.04 (0.77 to 1.31) | 10/8 | 1.19 (0.81 to 1.57) | 31/35 | 0.88 (0.72 to 0.83) | 26/28 | 0.92 (0.74 to 1.10) |
| ⩾65 | 33/53 | 0.62 (0.51 to 0.73) | 22/34 | 0.64 (0.50 to 0.78) | 30/36 | 0.83 (0.68 to 0.98) | 18/32 | 0.56 (0.43 to 0. 69) |
| All ages | 48/68 | 0.70 (0.60 to 0.80) | 32/40 | 0.79 (0.65 to 0.93) | 61/75 | 0.81 (0.71 to 0.91) | 48/63 | 0.76 (0.65 to 0.87) |
O, observed mortality; CHD, coronary heart disease; E, expected mortality; ICD, International Classification of Diseases; SMR, standardised mortality rate.
In patients with angina, coronary SMRs were increased in men (3.52 (95% CI 1.98 to 5.07)) and women (4.39 (95% CI 1.14 to 7.64)) <65 years, but not in older patients. In patients with non‐cardiac chest pain, coronary SMRs were lower than in the general population in older patients, but not in men (1.15 (95% CI 0.57 to 1.73)) and women (1.96 (95% CI 0.68 to 3.24)) <65 years.
Discussion
This multicentre study has shown that among patients with undifferentiated chest pain assessed in RACPCs, those diagnosed with angina have a substantially higher risk of death due to coronary heart disease or non‐fatal acute coronary syndrome than patients diagnosed with non‐cardiac chest pain and the general population. The data confirm the prognostic validity of differential diagnosis within RACPCs. Our finding that 32.4% of all events during follow‐up occurred in patients diagnosed with non‐cardiac chest pain highlights the need to reduce misdiagnosis and identify all who might benefit from secondary prevention treatment.
This is the first large, multicentre consecutive series of ambulatory patients with new, undifferentiated chest pain, allowing estimates of prognosis in women and men. Angina was diagnosed in 27% of patients, and in this group cumulative rates of death due to coronary heart disease or acute coronary syndromes were high, estimated at 8.62% after 1 year and 16.52% after 3 years. Our finding of a poor prognosis for patients with incident angina, none of whom had a history of myocardial infarction, emphasises the importance of early diagnosis within RACPCs and contrasts with findings in recent trials of chronic stable angina, ACTION (A CHF Trial Investigating Outcomes of Exercise Training)15 and PEACE (Prevention of Events with Angiotensin‐converting Enzyme Inhibition)16 reporting annual mortalities of 1.5% (95% CI 1.4% to 1.7%) and 1.7% (95% CI 1.5% to 1.9%) compared with 3.1% (95% CI 2.6% to 3.5%) in our registry population. The trialists' conclusions that angina has a good prognosis,15 with risk reduced to normal levels with contemporary treatment,17 may partly reflect the selection bias in the patients they recruited, which comprised stable patients in secondary or tertiary care settings. Similarly, 75% of patients in the Euro Heart survey18 of stable angina had had symptoms for >6 months before their first cardiological assessment and are different from the patients in our study with incident angina, many of whom were within 4 weeks and most within 6 months of symptom onset, suggesting recent plaque instability and predisposition to ischaemic events.19,20 Underuse of secondary prevention drugs may also have contributed to the high event rates we observed, and although rates of aspirin and β‐blocker treatment in patients in our study diagnosed with angina were similar to those reported in the Euro Heart Survey, only 28% were prescribed statins at this first cardiological consultation. This is lower than the entry treatment rates for angina trial participants, many of whom had had prior myocardial infarction and full cardiological investigation over many visits, but exceeds the treatment rates reported for patients with ischaemic heart disease in primary care settings.21 More than 80% of our patients with angina did undergo further cardiological follow‐up and although most probably came to receive statins, it is a limitation of our study that we do not know what proportion remained untreated.
Patients diagnosed with non‐cardiac chest pain in our study had a lower event rate, but accounted for almost one third of all primary end points. This is a cause for concern, because these patients had been assessed for coronary disease in the RACPCs and might therefore be expected to exhibit a distinctly lower coronary mortality than the general population. We found evidence for this in older patients diagnosed with non‐cardiac chest pain, but not in patients aged <65 years for whom SMRs were not significantly different from the general population. Probably most of these patients, who were told they did not have angina, but then had a coronary event, were misdiagnosed at the initial assessment, perhaps because they were younger than patients diagnosed with angina, fewer had typical symptoms and most had normal resting ECGs. Among patients diagnosed with non‐cardiac chest pain, coronary event rates fell below current thresholds for secondary prevention treatment,10 but we identified subgroups in whom hazard ratios for the primary end point were increased by ⩾50%. These included patients with diabetes, for whom secondary prevention treatment is already recommended,22 but also south Asians and patients with ECG abnormalities who might benefit from more aggressive preventive strategies in RACPCs. Although clinical factors signal a heightened risk among subgroups diagnosed with non‐cardiac chest pain, there is now a need for research to identify the methods for improving diagnostic precision. This may entail a better understanding of existing measures—for example, by development and validation of risk scores in this population, as well as consideration of the incremental prognostic or diagnostic value of serological testing23 and non‐invasive coronary imaging.24,25 Unlike myocardial infarction,26 there is no internationally agreed standard for defining the presence or absence of angina.
This is the first large multicentre study to evaluate the effectiveness of RACPCs by examining coronary outcomes in relationship to clinical diagnosis and mortality in the general population. There have been no previous outcome studies of other models of ambulatory chest pain assessment, particularly conventional cardiology outpatient clinics or chest pain assessment units. Our conclusions about the adverse prognosis of angina are consistent with those of a large population‐based outcome study from Finland,27 but are limited to those patients selected for referral by their primary care physicians, and generalisation to chest pain in the community requires caution. Additional limitations relate to ethical constraints that prohibited the documentation of ongoing secondary prevention treatment during follow‐up, and also the inevitable restriction imposed on baseline covariates by the data that was recorded. For example, a reliable history of hyperlipidaemia was unavailable, and we excluded from analysis family history of coronary disease as it was not clear whether it related to history of premature death in first‐degree relatives.
Conclusion
One‐stop cardiological assessment in RACPCs successfully identifies patients with incident angina who are at substantially higher coronary risk than those patients with non‐cardiac chest pain and the general population. However, >70% of patients attending these clinics were diagnosed with non‐cardiac chest pain, and our data have exposed misdiagnosis in a minority who were not appropriately treated. We need to improve the diagnosis and treatment of ambulatory patients when they first present with chest pain, to reduce coronary event rates.
Acknowledgements
We thank and remember the late Dr Sarah Cotter for her help with the statistical analysis and manuscript preparation. We also thank Dr Joanne Morris (Research & Development, Newham University Hospital) for administrative help and Dr Ranjadayalan (Newham University hospital), Dr Myers (Blackburn Royal Infirmary), Dr Best (Burnley General Hospital), Dr Curzen (Manchester Royal Infirmary), Dr Kadr and Dr Koh (Oldchurch hospital) and Dr Culling (Kingston General Hospital), for cooperating in this multicentre study and giving us permission to include their patients, and Mr Roger Stafford, the database manager, for his help.
Abbreviations
ECG - electrocardiogram
RACPCs - rapid access chest pain clinics
SMR - standardised mortality ratio
Footnotes
Funding: This study was funded by the National Health Service (NHS) Service Delivery and Organisation (SDO) research and development programme, to which interim progress reports were submitted. The funding body was not involved in study design or analysis.
Competing interests: None declared.
References
- 1.Kannel W B, Feinleib M. Natural history of angina pectoris in the Framingham study. Prognosis and survival. Am J Cardiol 197229154–163. [DOI] [PubMed] [Google Scholar]
- 2.Sutcliffe S J, Fox K F, Wood D A.et al Incidence of coronary heart disease in a health authority in London: review of a community register. BMJ 200332620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kentsch M, Rodemerk U, Gitt A K.et al Angina intensity is not different in diabetic and non‐diabetic patients with acute myocardial infarction. Z Kardiol 200392817–824. [DOI] [PubMed] [Google Scholar]
- 4.Stewart S, Murphy N, Walker A.et al The current cost of angina pectoris to the National Health Service in the UK. Heart 200389848–853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gandhi M M, Lampe F C, Wood D A. Incidence, clinical characteristics, and short‐term prognosis of angina pectoris. Br Heart J 199573193–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Duncan B, Fulton M, Morrison S L.et al Prognosis of new and worsening angina pectoris. BMJ 19761981–985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davie A P, Caesar D, Caruana L.et al Outcome from a rapid‐assessment chest pain clinic. QJM 199891339–343. [DOI] [PubMed] [Google Scholar]
- 8.Byrne J, Murdoch D, Morrison C.et al An audit of activity and outcome from a daily and a weekly “one stop” rapid assessment chest pain clinic. Postgrad Med J 20027843–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Department of Health National Service Framework for Coronary Heart Disease: modern standards and service models. London: Department of Health, 2000
- 10.British Cardiac Society Joint British recommendations on prevention of coronary heart disease in clinical practice. British Cardiac Society, British Hyperlipidaemia Association, British Hypertension Society, endorsed by the British Diabetic Association. Heart 199880(Suppl 2)S1–29. [PMC free article] [PubMed] [Google Scholar]
- 11.Ray S, Archbold R A, Preston S.et al Computer‐generated correspondence for patients attending an open‐access chest pain clinic. J R Coll Physicians Lond 199832420–421. [PMC free article] [PubMed] [Google Scholar]
- 12.Office for National Statistics A brief history of the ONS. http://www.bized.ac.uk/dataserv/ons/onshistory.htm (accessed 15 Sept 2006)
- 13.Anon NHS‐wide clearing system. http://www.connectingforhealth.nhs.uk/nwcs/ (accessed 15 Sept 2006)
- 14.Anon Patient Information Advisory Group. http://www.advisorybodies.doh.gov.uk/piag/ (accessed 15 Sept 2006)
- 15.Poole‐Wilson P A, Lubsen J, Kirwan B A.et al Effect of long‐acting nifedipine on mortality and cardiovascular morbidity in patients with stable angina requiring treatment (ACTION trial): randomised controlled trial. Lancet 2004364849–857. [DOI] [PubMed] [Google Scholar]
- 16.Braunwald E, Domanski M J, Fowler S E.et al Angiotensin‐converting‐enzyme inhibition in stable coronary artery disease. N Engl J Med 20043512058–2068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pitt B. ACE inhibitors for patients with vascular disease without left ventricular dysfunction—may they rest in PEACE? N Engl J Med 20043512115–2117. [DOI] [PubMed] [Google Scholar]
- 18.Daly C A, Clemens F, Sendon J L.et al The clinical characteristics and investigations planned in patients with stable angina presenting to cardiologists in Europe: from the Euro Heart Survey of Stable Angina. Eur Heart J 200526996–1010. [DOI] [PubMed] [Google Scholar]
- 19.Shah P K. Mechanisms of plaque vulnerability and rupture. J Am Coll Cardiol 200341(Suppl S)15S–22S. [DOI] [PubMed] [Google Scholar]
- 20.Abrams J. Chronic stable angina. N Engl J Med 20053522524–2533. [DOI] [PubMed] [Google Scholar]
- 21.Hippisley‐Cox J, Coupland C. Effect of combinations of drugs on all cause mortality in patients with ischaemic heart disease: nested case‐control analysis. BMJ 20053301059–1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Collins R, Armitage J, Parish S.et al MRC/BHF Heart Protection Study of cholesterol‐lowering with simvastatin in 5963 people with diabetes: a randomised placebo‐controlled trial. Lancet 20033612005–2016. [DOI] [PubMed] [Google Scholar]
- 23.Kragelund C, Gronning B, Kober L.et al N‐terminal pro‐B‐type natriuretic peptide and long‐term mortality in stable coronary heart disease. N Engl J Med 2005352666–675. [DOI] [PubMed] [Google Scholar]
- 24.Mollet N R, Cademartiri F, Nieman K.et al Multislice spiral computed tomography coronary angiography in patients with stable angina pectoris. J Am Coll Cardiol 2004432265–2270. [DOI] [PubMed] [Google Scholar]
- 25.Schmermund A, Denktas A E, Rumberger J A.et al Independent and incremental value of coronary artery calcium for predicting the extent of angiographic coronary artery disease: comparison with cardiac risk factors and radionuclide perfusion imaging. J Am Coll Cardiol 199934777–786. [DOI] [PubMed] [Google Scholar]
- 26.European Society of Cardiology/American College of Cardiology Myocardial infarction redefined—a consensus document of the Joint Committee for the redefinition of myocardial infarction. Eur Heart J 2000211502–1513. [DOI] [PubMed] [Google Scholar]
- 27.Hemingway H, McCallum A, Shipley M.et al Incidence and prognostic implications of stable angina pectoris among women and men. JAMA 20062951404–1411. [DOI] [PubMed] [Google Scholar]