Abstract
Spirochaetes are organisms that can infect the colon of people with normal or compromised immune systems. Infected patients can present with a variety of gastrointestinal symptoms, including diarrhoea and rectal bleeding. However, some report a lack of association between specific symptoms and the presence of spirochaetes. It is therefore unclear whether the spirochaetes colonising the colon are true pathogens. Diagnosis is typically made by histological examination, with the biopsy specimen showing a band‐like growth of spirochaetes adherent to the colonic luminal surface, giving an accentuated brush‐border appearance. A course of metronidazole can eliminate the spirochaetes, but treatment might not lead to improvement of symptoms. Owing to the lack of a definite association between symptoms and the presence of spirochaetes, observation without specific antibiotic treatment can be pursued in most patients.
Spirochaetes are long and tightly coiled bacteria that cause diseases in humans. Treponema pallidum and Borrellia burgdorferi are among the best‐known spirochaetes, responsible for syphilis and Lyme's disease, respectively. In addition, species of spirochaetes can infect the human gastrointestinal tract, in the setting of either a normal or compromised immune system. Colonic spirochaetosis is a disease caused by the Gram‐negative bacteria Brachyspira aalborgi and Brachyspira pilosicoli. Infected patients can present with a variety of gastrointestinal symptoms, including diarrhoea and rectal bleeding. This paper describes a case of colonic spirochaetosis in an immunocompetent host. The purpose of this report is to raise awareness that spirochaetosis is a possible but rare cause of diarrhoea and haematochezia in humans, common presenting symptoms that are associated with several gastrointestinal diseases.
Case report
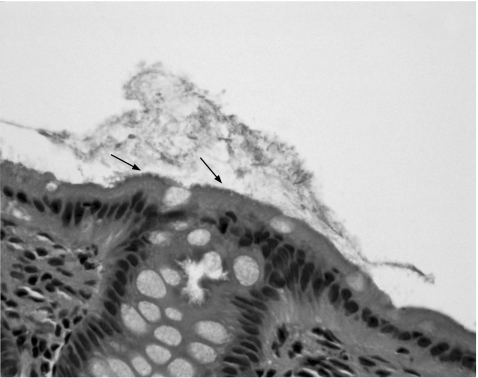
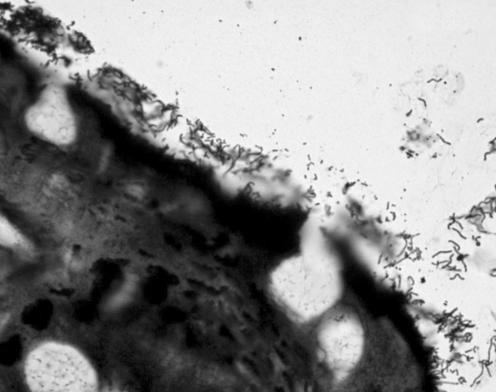
A 35‐year‐old man presented to the clinic with a 5‐day history of intermittent haematochezia and several weeks of loose stools associated with lower abdominal cramping pain. He had had similar symptoms 2 years previously. Colonoscopy at that time showed normal‐appearing mucosa and internal haemorrhoids. He had since been asymptomatic until the current episode. The patient denied any associated weight changes, nausea or vomiting, fever or chills. There was no additional notable medical history. He was not taking any treatment. Family history was negative for gastrointestinal illness. Personal history was notable for active tobacco use, but he denied any history of alcohol or illicit drug use, or anal intercourse. Examination showed a well‐nourished, well‐developed man with no remarkable findings on physical examination. Laboratory results included haemoglobin 18 (14–18) g/dl, haematocrit 51.9% (42–52%), platelet count 276 000/μl (140 000–400 000/μl) and leucocytes 7100/μl (4800–10 800/μl). Serum electrolytes, albumin, liver enzymes and creatinine were in established normal limits. Stool samples for leucocytes, culture, ova and parasites, cryptosporidium, and Clostridium difficile toxin tested negative. Colonoscopy was carried out and again showed normal‐appearing mucosa. Because of the persistence in loose stools, random biopsy specimens were obtained in the descending and sigmoid colon and in the rectum. Histological examination was remarkable for a basophilic apical border on the colonic epithelium, with no associated inflammation (fig 1). Warthin–Starry staining showed the basophilic luminal border to be spirochaetes (fig 2). A diagnosis of colonic spirochaetosis was made. The patient had been in a long‐term heterosexual relationship and denied any history of receptive anal intercourse. Further laboratory investigations included a negative HIV test, non‐reactive serum rapid plasma reagin and microhaemagluttination test for T pallidum, negative leptospira serology and Lyme enzyme immunoassay. The patient was treated with single‐dose penicillin G benzathine 2.4 million units intramuscularly. One month later, the patient presented to the urgent care clinic with persistent bloody diarrhoea. A trial of mesalamine was started, and the patient subsequently had resolution of his symptoms. The patient moved out of the area and was lost to follow‐up.
Figure 1 Haematoxylin and eosin staining (×40) of the patient's colonic mucosa with a basophilic apical border (arrows).
Figure 2 Warthin–Starry staining (×100) of the patient's colonic mucosa, showing the numerous spirochaetes on the luminal surface.
Discussion
The prevalence of spirochaetosis varies from 2.5% to 16% in Western countries and is considerably higher in the developing world.1,2 Spirochaetosis affects up to 5% of healthy people and up to 30% of homosexual men without evidence of immunodeficiency.3,4 Sexual contact and a history of oral–anal contact has been suggested as a route of infection in homosexual adults.5 The incidence of colorectal spirochaetosis ranges from 1% to 10%.3,6 It is unclear whether the spirochaetes colonising the colon are true pathogens.3 Some report a lack of association between specific gastrointestinal symptoms and an absence of mucosal inflammation despite the presence of spirochaetes.6 This observation to some degree parallels Helicobacter pylori infection of the upper gastrointestinal tract, as not all infected people manifest ulcerative disease, inflammation or clinical symptoms. The spirochaetes in some cases can develop from being enteric commensal organisms to opportunist pathogens,7 owing to factors such as increased virulence of the associated microorganism or to diminished host defence, leading to an inflammatory response of the host. Several cases of diarrhoea,6,8 invasive colitis and hepatitis,9 and rectal bleeding10 have been reported; thus, patients with spirochaetosis may present with these symptoms.4 Spirochaetosis has also been associated with appendicitis, but in most cases, spirochaetosis is an incidental finding with no clear clinical correlates.11
Colonic spirochaetosis is a disease caused by the Gram‐negative bacteria Brachyspira aalborgi and Brachyspira pilosicoli. Brachyspira pilosicoli induces disease in both humans and animals, whereas Brachyspira aalborgi affects only humans and higher primates. Neither Brachyspira pilosicoli nor Brachyspira aalborgi has been well characterised in terms of basic cellular functions, pathogenicity or genetics.12 The literature to date suggests that human intestinal spirochaetes are heterogeneous, and further refinements in classification are required. A close phenotypic similarity between human isolates and non‐pathogenic porcine intestinal spirochaetes has been shown.13 No common organism has been cultured in a large number of cases of spirochaetosis, but a sequence specific to Brachyspira aalborgi was detected by polymerase chain reaction in 62.5% of patients with spirochaetosis.14
Spirochaetes are difficult to grow in culture media and are not detected by routine examination of stool,15 so diagnosis usually requires a biopsy specimen of the colon. Typical histological findings on the biopsy specimen including a band‐like growth of spirochaetes adherent to the colonic luminal surface, giving an accentuated brush‐border appearance. Special stains including Giemsa, periodic acid‐Schiff and silver stains are used to visualise the organisms,7 although most cases can be identified readily on sections satined with haematoxylin and eosin. Spirochaetes can colonise or infect the proximal or distal colon. The absence of spirochaetes on a rectal biopsy specimen, for example, does not rule out more proximal infection.11
Treatment with metronidazole has been shown to eliminate the spirochaetes.16,17 However, treatment might not lead to improvement of symptoms. In most cases, the patient can be observed without antibiotic treatment. Depending on the severity of the presenting symptoms and the clinical findings, a therapeutic trial may be undertaken.18 Our patient was treated originally with penicillin G, which is not the antibiotic of choice for spirochaetosis, so it is not surprising that he continued to have symptoms after receiving penicillin. The relevance of mesalamine is unclear in our patients. Mesalamine can reduce colonic inflammation and improve diarrhoea in inflammatory bowel disease, and we postulate that this happened in our patient. Longer follow‐up was not available, so it is difficult to ascertain whether the patient's symptoms truly responded to treatment with mesalamine.
Footnotes
Competing interests: None declared.
References
- 1.Lindboe C F. The prevalence of human intestinal spirochetosis in Norway. Anim Health Res Rev 20012117–119. [PubMed] [Google Scholar]
- 2.Delladetsima K, Markaki S, Papadimitriou K.et al Intestinal spirochaetosis. Light and electron microscopic study. Pathol Res Pract 1987182780–782. [DOI] [PubMed] [Google Scholar]
- 3.Nielsen R H, Orholm M, Pederson J O.et al Colorectal spirochetosis. Clinical significance of the infestation. Gastroenterology 19838562–67. [PubMed] [Google Scholar]
- 4.Surawicz C M, Roberts P L, Rompalo A.et al Intestinal spirochetosis in homosexual men. Am J Med 198782587–592. [DOI] [PubMed] [Google Scholar]
- 5.Law C H L, Griersen J M, Stevens S M B. Rectal spirochetosis in homosexual men: the association with sexual practices, HIV infection and enteric flora. Genitourin Med 19947026–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee F D, Kraszewski A, Gordon J.et al Intestinal spirochetosis. Gut 197112126–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alsaigh N, Fogt F. Intestinal spirochetosis: clinicopathological features with review of the literature. Colorectal Dis 2002497–100. [DOI] [PubMed] [Google Scholar]
- 8.Crucioli V, Busutill A. Human intestinal spirochetosis. Scand J Gastroenterol 198116177–179. [PubMed] [Google Scholar]
- 9.Kostman J R, Patel M, Catalano E.et al Invasive colitis and hepatitis due to previously uncharacterized spirochetes in patients with advanced human immunodeficiency virus infection. Clin Infect Dis 1995211159–1165. [DOI] [PubMed] [Google Scholar]
- 10.Douglas J G, Crucioli V. Spirochetosis: a remediable cause of diarrhea and rectal bleeding? BMJ 19812831362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Henrik‐Nielsen R, Lundbeck F A, Teglbjaerg P S.et al Intestinal spirochetosis of the vermiform appendix. Gastroenterology 198588971–977. [DOI] [PubMed] [Google Scholar]
- 12.Smith J L. Colonic spirochetosis in animals and humans. J Food Prot 2005681525–1534. [DOI] [PubMed] [Google Scholar]
- 13.Tompkins D S, Foulkes S J, Godwin P G R.et al Isolation and characterisation of intestinal spirochaetes. J Clin Pathol 198639535–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mikosza A S, La T, Brooke C J.et al Amplification from fixed tissue indicates frequent involvement of Brachyspira aalborgi in human intestinal spirochetosis. J Clin Microbiol 1999372093–2098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Orenstein J M, Dieterich D T. The histopathology of 103 consecutive colonoscopy biopsies from 82 symptomatic patients with acquired immunodeficiency syndrome: original and look‐back diagnosis. Arch Pathol Lab Med 20011251042–1046. [DOI] [PubMed] [Google Scholar]
- 16.Lo T C N, Heading R C, Gilmour H M. Intestinal spirochaetosis. Postgrad Med J 199470134–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gebbers J ‐ O, Ferguson D J P, Mason C.et al Spirochetosis of the human rectum associated with an intraepithelial mast cell and IgE plasma cell response. Gut 198728588–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van Mook W, Koek G H, Van der Ven A.et al Human intestinal spirochetosis: any clinical significance? Eur J Gastroenterol Hepatol 20041683–87. [DOI] [PubMed] [Google Scholar]