Abstract
Objective
To develop a measure of home and community participation related to the World Health Organization’s International Classification of Functioning, Disability and Health.
Design
Cross-sectional analysis of survey data.
Setting
Nine medical inpatient rehabilitation facilities from 6 states.
Participants
A total of 594 patients of mixed impairment type admitted for inpatient rehabilitation in 2002. Mean age was 74.0 years and 61.4% were women.
Interventions
Not applicable.
Main Outcome Measures
Reliability and validity of the participation instrument.
Results
A 20-item instrument of home and community participation was developed (PAR-PRO). The instrument showed good internal consistency and good Rasch person and item fit statistics. Four subfactors were identified beyond the unidimensional construct of participation including domestic management, socialization, physical vigor, and generative activities. The PAR-PRO total participation score correlated inversely with age (r=−.31, P<.001) but did not differ by sex.
Conclusions
The 20-item PAR-PRO instrument of home and community participation displayed good psychometric characteristics. The instrument shows promise as a broad measure of home and community involvement for persons with disabilities. Further work is needed to support its application for people without disability.
Keywords: Activities of daily living, Consumer participation, Outcome assessment (health care), Rehabilitation
The World Health Organization’s (WHO) conceptual triad of impairment, disability, and handicap1 has been revised2 to reflect an updated perspective on health and related domains. The new taxonomy entitled International Classification of Functioning, Disability and Health (ICF),2 provides a systematic method to classify health-related states in terms of: (1) physiologic structures and function, (2) performance of tasks needed to sustain everyday life, (3) involvement in everyday life situations, and (4) the interaction of these constructs with environmental factors and contexts.
In tandem with the WHO’s updated ICF publication, the Commission of Accreditation of Rehabilitation Facilities (CARF) requires medical rehabilitation programs to collect information that addresses patient impairments, the activities that these people wish to participate in and the goals they wish to achieve, as well as, information about roles and participation in their community.3 To conform to CARF standards, this information should be collected at the beginning of the rehabilitation experience, at the end of the rehabilitation intervention, and at appropriate points in time following service.3 Standardized methods for assessing participation, defined in the ICF as "involvement in a life situation,"2(p are lacking in medical rehabilitation.
The domains of activities and participation in the ICF include learning and applying knowledge, communication, mobility, self-care, domestic life, interpersonal interactions and relationships, major life areas, and community social and civic life. These domains are assessed using 2 qualifiers—performance and capacity. The performance qualifier describes what an individual does in his/her current environment. The capacity qualifier describes a person’s ability to execute a task or an action. Capacity is meant to indicate the highest level of functioning that a person may reach in a given domain at a given moment. The ICF acknowledges that it is “difficult to distinguish between ‘Activities’ and ‘Participation’ on the basis of the domains in the Activities and Participation components.”2(p The ICF notes that within the domains described above “the only possible indicator of participation is coding through performace,”2(p In the development of the PAR-PRO instrument described below, we have been guided by the ICF domains and attempted to operationalize the concept of performance by using reported frequency of participation in activities consistent with the ICF domains.
Two measures of community involvement—the Community Integration Questionnaire (CIQ)4,5 and the Craig Handicap and Reporting Technique (CHART)6—are currently used in medical rehabilitation. The CIQ, a 15-item scale developed for people with traumatic brain injury (TBI), assesses home integration, social roles, and productive activities. The primary application of the CIQ is in patients with TBI,7 though it has been used in patients with burns8 and with brain tumor.9 A revised version of the CIQ with 13 items and a modified scoring system has been proposed.10
The CHART, a 32-item scale developed for people with spinal cord injury (SCI), was designed to meet the WHO1 concept of impairment, disability, and handicap.6 The original scale contained items assessing handicap within 5 WHO domains including physical independence, mobility, occupation, social integration, and economic self-sufficiency.11 Items were later added to reflect the construct of orientation and cognitive independence.12 The CHART has enjoyed wide use in patients with SCI.13,14 More recently, the CHART has been used as a measure of participation across a variety of disability groups, including TBI, multiple sclerosis, stroke, burn, and amputation.15
Both the CIQ and CHART have adequate psychometric characteristics, though each scale has characteristics which potentially limit their use as a general measure of participation that is consistent with the updated ICF and applicable to disabled and nondisabled people. That is, because the CIQ and the CHART were both developed prior to the publication of the ICF their correspondence with the 9 domains of life situations described within the ICF has not been established. The original CIQ, for example, does not assess such ICF domains as learning and applying knowledge, communication, mobility, or self-care.
Several new or revised measures have been introduced in the rehabilitation research literature. These include the Community Integration Questionnaire–2,16 the Community Integration Measure,17 and the Participation Objective, Participation Subjective.18 Each of these measures is new and their psychometric properties and clinical usefulness are being examined.19
The purpose of this article is to describe the development of a new measure of participation (PAR-PRO). The development of the PAR-PRO was guided by the principles, definitions and domains of the ICF and designed for use in both disabled and nondisabled populations. The article first describes how the instrument was developed and then presents initial information on psychometric characteristics based on a multicenter sample of individuals with a mixture of diagnoses undergoing inpatient medical rehabilitation. Our goal in this study was to begin the process of establishing the reliability and validity of the PAR-PRO in a large sample of persons with disabilities.
Methods
Sample and Participants
In 2002, 20 health care facilities subscribing to the Uniform Data System for Medical Rehabilitation (UDSMR) expressed an interest in helping to develop a broad measure of home and community participation. Of these, 9 facilities participated in data collection. The 9 facilities were representative of the national inpatient rehabilitation facilities experience: operating bed sizes ranged from 12 to 60 (mean bed size, 30); 6 of 9 facilities were CARF-accredited; and 7 of 9 were accredited by the Joint Commission on Accreditation of Healthcare Organizations. The facilities were located across diverse regions of the country (eg, California [n=2], Florida, Missouri, North Carolina, Ohio [n=2], and Texas [n=2]). All 9 facilities obtained institutional review approval prior to data collection. Comparison with the entire UDSMR database revealed that the participating facilities were comparable in size, case mix, age ranges, and sex distribution to the larger facility dataset (N>800).
From an initial 627 patient records, 33 were removed from the analysis because of missing data for the participation items. The remaining 594 patient records (on average of 66 records per facility), formed the basis of the current study. Because the primary purpose of the study was to evaluate the psychometric characteristics of a new home and community participation instrument, limited demographic information (sex, age, impairment group) was collected.
Measures
PAR-PRO instrument development
The PAR-PRO participation instrument was developed by a panel with expertise in: (1) clinical areas of medical rehabilitation including physiatry, rehabilitation nursing, physical therapy, occupational therapy, and psychology and neuropsychology; (2) the application of CARF accreditation standards for medical rehabilitation (2 members of the panel were CARF surveyors); and (3) outcomes assessment and instrument development. In the initial phase of development, the ICF was reviewed to clearly understand the scope of the revised classification system, and to begin the process of identifying potential participation items that were consistent with the ICF. Participation is defined in the ICF as "involvement in a life situation" and stands in contrast to "activities" which is defined as "execution of a task or action."2(p According to the ICF, both participation and activities are reflected in 9 domains that are meant to cover the full range of life areas.2 These domains are presented in the first column of table 1. Within each domain, the ICF provides subdomains and sublevels of detail, ending with items reflecting specific behaviors and life situations. Some examples of these lower levels are also shown in the first column of table 1.
Table 1.
PAR-PRO and FIM Instrument Items in Relation to ICF Primary Domains
| ICF Activities and Participation Domains and Subdomain Examples2 | FIM Instrument (F) or Major PAR-PRO (P) Items |
|---|---|
| I. Learning and applying knowledge | |
| Basic learning | Memory (F) |
| Applying knowledge | Problem solving (F) |
| II. General Tasks and Demands | No items developed for this domain |
| Undertaking a single task | |
| Carrying out daily routine | |
| Handling stress and other psychologic demands | |
| III. Communication | |
| Communicating with: receiving spoken messages | Comprehension (F) |
| Communicating with: producing | Expression (F) |
| IV. Mobility | |
| Changing and maintaining body position | Transfer: chair (F), bed (F), tub (F) |
| Walking and moving | Walk/wheelchair (F); stairs (F) |
| Moving around, using transportation | Public transportation (P); Traveling/sightseeing (P); Driving a vehicle (P) |
| V. Self-care | |
| Washing oneself | Bathing (F) |
| Caring for body parts | Grooming (F) |
| Toileting | Bladder (F); Bowel (F); Toileting (F) |
| Dressing | Dress upper (F); Dress lower (F) |
| Eating | Eating (F) |
| VI. Domestic Life | |
| Acquisition of goods and services | Shopping for food, necessities (P) |
| Household tasks | Meal preparation/cooking (P); Light housework (P); Heavy housework (P); Yard work/home maintenance (P) |
| Assisting others | Caregiver activities (P) |
| VII. Interpersonal Interactions and relationships | |
| Particular interpersonal relationships | Socializing inside/outside the home (P); Intimate relationship with significant other (P) |
| VIII. Major Life Areas | |
| Education | School/education (P) |
| Work and employment | Work/employment (P); Volunteer/public service (P) |
| Economic life | Money management/home finances (P) |
| IX. Community, social and civic life | |
| Recreation and leisure | Hobbies/arts & crafts (P); Playing sports/exercising (P); |
| Religion and spirituality | Movies/theater/concerts/sporting events (P); Religious/spiritual activities (P) |
A primary challenge in developing a new measure of participation was to cover as many of the ICF domains as possible within a brief, practical instrument. We did not focus on domains such as self-care or mobility because other assessments, including the FIM instrument, are currently used to evaluate ICF domains associated with activities. The PAR-PRO participation instrument was constructed to complement assessments like the FIM instrument, with participation items designed to cover higher level, more complex life experiences included within the IFC domains of participation, such as domestic life, interpersonal interactions and relationships, and major life areas (education, work). It was anticipated that designing the PAR-PRO participation instrument to complement the FIM instrument would allow for ample coverage of both activities and participation across the 9 ICF domains without increasing the burden of information collected.
A second philosophic decision was made with respect to the breadth and expected application of the PAR-PRO participation instrument. The PAR-PRO participation instrument, designed for use in people with moderate to severe disability, was also meant to be broad enough in scope for use in people without disability. The WHO developed the ICF for use with all people, not just those with disability.
The ICF recommends a single generic scaling approach for coding both activity and participation, based on the degree the individual has a "problem" with the content area (eg, "xxx.0 NO problem"; "xxx.1 MILD problem", etc.).2(p Additional indicators are provided for responses that are "not specified" or "not applicable." The ICF also provides for 2 types of qualifiers: performance and capacity. As noted previously, the performance qualifier describes what the person does in his/her current environment.2
In developing the PAR-PRO participation instrument, greater value was placed on measuring performance as opposed to capacity. This approach most closely matches the current philosophy in medical rehabilitation where measures of functional capacity assess the individual's actual ability to perform the activity. The PAR-PRO participation instrument was designed to measure the frequency a life situation occurs within a defined time period. This format provides information on the person’s participation performance. The information is concrete and relatively free from subjective judgment (ie, the individual either participated in the life situation during the time frame, or did not).
The PAR-PRO participation instrument was also designed to address CARF standards for inpatient rehabilitation which requires data collection at 3 or more points in time: admission, discharge, and at points in time following discharge. The focus of the current study was the collection of participation information at admission. Because it was judged unlikely that individuals just admitted for inpatient medical rehabilitation would have experienced many of the ICF life situations in the weeks immediately prior to admission, individuals were asked to provide information about their typical degree of participation in the year prior to the episode of illness. This pre-illness measurement was set up to provide a benchmark from which to plan for participation activities following discharge.
Instrument Construction
Existing measures with potential relevance to the ICF definition of community participation were reviewed for possible content inclusion. Using information from existing instruments and clinical experience, a list 50 potential items was generated. The list was given to an expert panel who reviewed the ICF and were asked to consider items matching each of the ICF domains, with the additional instruction to ignore ICF domains, subdomains, or sublevels already covered by the FIM instrument. Experts were asked to use their clinical experience to evaluate the relevance of individual items to persons with disability while at the same time considering items with a wide enough range to be appropriate for people without disability. The panel was also asked to develop items that were as free from age, sex, cultural, geographic, and socioeconomic bias as possible. An iterative process among panel members occurred until the list of items was narrowed to 20 items for pilot testing. Table 1 shows the relation of each ICF domain and major subdomain to the FIM and PAR-PRO instrument items.
Once the 20 items were agreed on, item scaling characteristics were developed. To anchor the PAR-PRO participation instrument, all 20 items were scaled using the following coding system: "0 – Did not participate in this life situation"; "1 – Participated monthly (once every 3–4 weeks)"; "2 – Participated bi-weekly (once every 2 weeks)"; "3 – Participated weekly (1–4 days per week)"; and "4 – Participated daily/almost daily (5 or more days per week)."
Data Collection
The 9 facilities participating in data collection were provided with a standard data collection form and a handbook containing standard directions, definitions, and scoring guidelines. Once familiar with the scale, facilities used the 20-item PAR-PRO participation instrument as an interview tool to collect data in a standard fashion from patients receiving inpatient medical rehabilitation.
For the initial assessment, facilities were instructed to interview the patient within the first 3 calendar days of admission to the facility. The patient was asked to provide retrospective information about his/her frequency of participation during the year prior to the hospitalization or episode of illness. Rehabilitation staff collected the information in face-to-face interviews when it was judged (by rehabilitation staff) that the patient had the ability to fully understand the questions and was able to provide reliable and valid responses. Proxy information was used if the patient was judged unable to fully understand the questions. Data collection began in 2002 and continued till April 2003. Data were entered on paper forms, coded into electronic spreadsheets, and later merged into a common database at the UDSMR. Records were not entered into the final database if information was missing for any of the 20 participation items. A copy of the original 20-item instrument is attached as appendix 1.
Statistical Analysis
Test reliability (internal consistency) was assessed by coefficient α20 using the SPSS reliability analysis procedure.21,a Test validity22 was addressed through content and construct validity. Content validity was established via expert panel item selection. Construct validity was examined using Rasch analysis, factor analysis, measurement of internal consistency, and, to a limited extent, by examining subgroups performance (age, sex, impairment groups).
To begin the process of construct validity, we first evaluated the underlying structure of the 20 items in relation to one another, to determine if the items measured a single underlying participation construct. All 20 items, using the 0-to-4 rating scale, were subjected to Rasch analysis using Winsteps, version 3.42.23,b The default rating scale model, with groups equal to 1, was specified; this model assumes that all of the items share the same underlying rating scale structure. The Rasch measurement model was used to provide interval measures from raw scores, based on an ordinal scale to examine item separation reliability and person separation, and to determine the unidimensionality of the participation construct.
Exploratory factor analysis was performed to examine item consistency and the dimensionality of the participation construct using a principal components analysis with varimax rotation. The stopping criterion of extraction of factors with eigenvalues of 1.0 or more was used. Because the patient responses represented ordinal level data, the raw ratings were converted to an interitem polychoric correlation matrix. We used independent sample t tests and 1-way analyses of variance (ANOVAs) to compare subgroups based on sex, age, and impairment status to determine if the PAR-PRO items were able to differentiate on these basic sociodemographic variables. All tests were conducted using an α level of P less than .05.
Results
The final sample included 594 subjects from 9 facilities located in 6 states. The mean age was 74.0 years and 61.4% were women. The ages ranged from 19 to 99 years and were distributed evenly across the 9 facilities. Data on impairment group code was available for 416 patients (70% of total sample), and was similar to the general rehabilitation population24 including orthopedic (31.9%), stroke (25.5%), neurologic (10.3%), brain injury (6%), cardiac and pain (4.8%), arthritis (4.6%), and the remaining rehabilitation impairment categories less than 5%. Fewer than 6% (n=35) of patients required assistance from others (eg, spouse, parent, son or daughter) to answer the 20 participation items.
Rasch Analysis
Because 14 patient records were identified as extreme (all scored as all zero) they were removed from the Rasch analysis. Rasch output for the remaining 580 patient records showed an uneven distribution of item responses over the 5 categories (0–4). More than half (51%) of the responses were scored as "0 – Activity did not occur," while 9% were scored as "1 – Monthly." The measure structure also indicated potential problems with category disordering (increasing measure values on the PAR-PRO instrument did not always imply the respondents had higher category ratings). Original scoring categories of 1 and 2 were combined into a new category of 1, and scoring categories of 3 and 4 were combined into a new category 2; and category 0 remained unchanged. This modification created a new scaling system with 3 levels: 0 equals none (activity did not occur), 1 equals monthly (activity occurred at least once per month but less than weekly), and 2 equals weekly (activity occurred at least once per week). With the modified category scaling system, 51% of the responses used category 0, 21% used category 1, and 28% used category 2. The remaining Rasch analyses use the revised 3-category scaling system.
The Rasch output was next evaluated for evidence of individual response strings that did not fit the overall model. Such people were identified through the use of person fit statistics. The analysis revealed 40 responses with person infit or outfit mean square statistics above the threshold cutoff of 2.0, suggesting that these response strings did not fit the underlying model. The 40 patient records were removed from further Rasch analysis.
With extreme misfitting responses removed, the average infit mean square value for persons was 1.01, and the average outfit mean square value was 1.03, indicating overall infit statistics that were very close to the Rasch theoretical model values of 1.00.25 Similarly, infit and outfit average mean square values for the PAR-PRO participation items were 1.07 and 1.03, respectively, again indicating good overall data fit to the model. The person separation index, a marker of different participation levels, was 1.64, indicating that there were 2.52 distinct person participation strata within this scale. The item separation index, a marker of how successful items are in defining different strata within a measure, was 10.37 indicating that there were 14.2 distinct item participation strata within the scale. Table 2 shows infit and outfit statistics for each individual item, along with information on the level of participation for each item. None of the infit or outfit item statistics were lower than 0.5 or greater than 2.0, indicating that all 20 items fit the underlying model well. The findings suggest that the 20 PAR-PRO participation items fit a unified measure of participation, that there were clearly discernable "participation” levels within this sample, and that there was good separation among items.
Table 2.
Rasch Item Fit Statistics and Measure Frequency Endorsement for PAR-PRO Items, From Least Frequently Endorsed to Most Frequently Endorsed
| PAR-PRO Item | RASCH Measure (logits) | Infit Mean Square | Outfit Mean Square |
|---|---|---|---|
| School/education | 3.89 | 1.50 | 0.74 |
| Volunteer/public service | 1.38 | 1.26 | 1.04 |
| Caregiver activities | 1.38 | 1.47 | 1.21 |
| Public transportation | 1.37 | 1.51 | 1.80 |
| Work/employment | 1.21 | 1.46 | 1.22 |
| Yard work/home maintenance | 0.54 | 0.92 | 0.77 |
| Playing sports/exercising | 0.38 | 1.16 | 1.16 |
| Travel/sightseeing | 0.30 | 0.71 | 0.85 |
| Movies/theater/concerts/sporting events | 0.14 | 0.74 | 0.83 |
| Heavy housework | 0.13 | 0.84 | 0.76 |
| Relationship with significant other | −0.50 | 1.58 | 1.72 |
| Driving a vehicle | −0.75 | 1.18 | 1.11 |
| Hobbies/arts & crafts | −0.87 | 0.95 | 1.07 |
| Religious/spiritual activities | −0.90 | 1.25 | 1.29 |
| Shopping for food/necessities | −0.96 | 0.66 | 0.64 |
| Light housework | −1.04 | 0.59 | 0.56 |
| Money management/home finances | −1.19 | 0.94 | 1.03 |
| Meal preparation/cooking | −1.27 | 0.95 | 0.93 |
| Socializing outside the home | −1.63 | 0.83 | 0.87 |
| Socializing inside the home | −1.65 | 0.92 | 1.03 |
Figure 1 shows the hierarchy for the 20 PAR-PRO participation items; with item frequency on the right and person frequency on the left (each # symbol represents 6 people). Most items were well-separated across the hierarchy, with the exception of heavy housework and attending events. Socializing in one's own home was the most frequently endorsed participation activity, while participating in school was the least frequently endorsed. The person participation frequency range matched well with the range of participation items, with mean item and person frequency endorsement (represented on both sides of the figure as "M") within .77 logits. Items including school, caregiver, public transportation, volunteer, and work exceeded the person frequency endorsement range, which indicates reduced frequency. This likely reflects a relative lack of involvement in vocational or educational aspects of life, an expected finding given the average age of 74.0 years in this sample. Socializing in and outside the home was lower than the range of the most frequently endorsed PAR-PRO items, which suggests the potential for a possible floor effect in people with moderate to severe disability.
Fig 1.
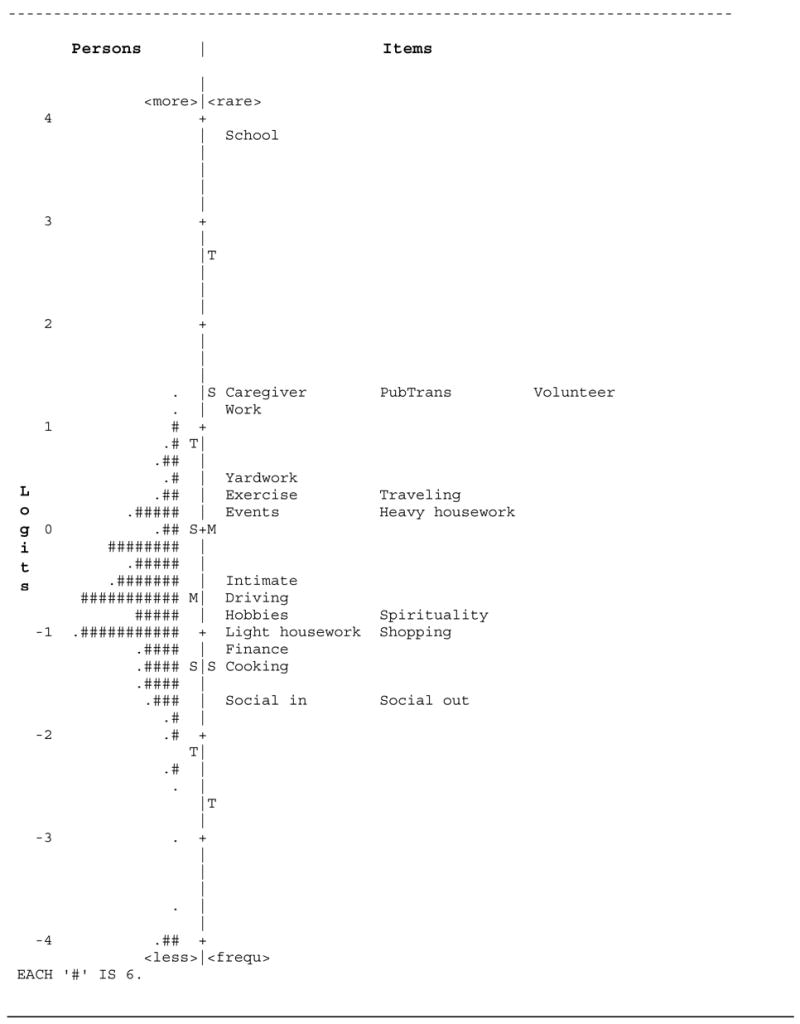
Rasch person and item frequency map, in logits, for the 20 PAR-PRO items. Values reported for both persons and items. Legend: M, mean; S, 1 standard deviation; T, 2 standard deviations.
The Rasch analyses described above were repeated without entering the cases for whom a proxy was the respondent (n=34). Results for these analyses did not reveal substantial differences from the original findings. There was no evidence that proxy provided data had an impact on the frequency or pattern of responses provided. Only the findings for combined patient and proxy data are presented in this report.
Psychometric Characteristics
Coefficient α for the overall sample (N=594) was .77. This indicates good internal consistency, and supports a unidimensional participation construct. Table 3 shows the mean PAR-PRO participation item rating (overall mean ± standard deviation, 15.2±6.4; range, 0–31) which reflects participation prior to illness onset. Pre-illness participation was highest for socialization, meal preparation, and light housework, and lowest for school, volunteer and work activities. This pattern of low participation in so-called "productive activities" is consistent with the age and life role status of the sample.
Table 3.
Total and Individual Mean Score on the 20 PAR-PRO Participation Instrument (N=594)
| PAR-PRO Item | Mean ± SD |
|---|---|
| 1. Work/employment | 0.24±0.64 |
| 2. School/education | 0.04±0.27 |
| 3. Volunteer/public service | 0.21±0.56 |
| 4. Meal preparation/cooking | 1.27±0.82 |
| 5. Light housework | 1.16±0.77 |
| 6. Heavy housework | 0.56±0.78 |
| 7. Caregiver activities | 0.23±0.62 |
| 8. Money management/home finances | 1.24±0.81 |
| 9. Shopping for food, necessities | 1.14±0.79 |
| 10. Yardwork/home maintenance | 0.42±0.73 |
| 11. Hobbies/arts & crafts | 1.07±0.81 |
| 12. Socializing inside the home | 1.44±0.70 |
| 13. Socializing outside of the home | 1.43±0.74 |
| 14. Traveling/sightseeing | 0.41±0.62 |
| 15. Movies/theater/concerts/sporting events | 0.56±0.63 |
| 16. Playing sports/exercising | 0.50±0.79 |
| 17. Religious/spiritual activities | 1.09±0.89 |
| 18. Using public transportation | 0.22±0.56 |
| 19. Driving a vehicle | 1.01±0.98 |
| 20. Intimate relationship with significant other | 0.87±0.97 |
| Total PAR-PRO | 15.19±6.4 |
Abbreviation: SD, standard deviation.
Correlation between age and PAR-PRO total participation rating was −.31 (N=594, P<.001), indicating a significant inverse relationship between age and overall participation. An independent samples t test showed the PAR-PRO total participation score was higher for younger people (=65y; n=119) with a mean score of 17.6, than for older people (=66y; n=475) with a mean score of 14.6 (t592=4.673, P<.001). Subsequent analyses of selected PAR-PRO participation items indicated that younger people were more likely to have participated in work (t592=7.443, P<.001) and school (t592=3.061, P<.002) activities compared with older people, but the 2 groups did not differ in volunteer activities. In contrast to the age effect, the PAR-PRO total participation rating did not differ by sex. The mean rating for men was 14.8±6.2, and for women, 15.4±6.5.
PAR-PRO participation rating comparisons across impairment groups were limited by the small sample size for many of the impairment groups. For the current analysis, only cases with orthopedic (n=133), stroke (n=106), or neurologic disorders (n=43) were considered. A 1-way ANOVA, using Scheffé procedures for analysis of post hoc multiple comparisons was run comparing PAR-PRO total participation ratings among the 3 impairment groups. The 3 groups differed on PAR-PRO total participation rating (F2,281=6.098, P<.003). Orthopedic patients had significantly higher PAR-PRO total participation ratings (mean, 17.1) than patients with stroke (mean, 14.7; P<.008) or neurologic disorders (mean, 14.3; P<.047); the total ratings did not differ between the stroke and neurologic disorders groups. Because age was significantly related to PAR-PRO total participation rating, an analysis of covariance (ANCOVA) was run to compare the 3 impairment groups, with age as a covariant. The ANCOVA results indicated that the impairment groups differed significantly in PAR-PRO total participation rating, even when age differences among the groups were controlled (F2,281=5.22, P<.006).
Table 4 shows a principal component analysis using varimax (orthogonal) rotation with Kaiser normalization. Using the accepted threshold of eigenvalues greater than 1.0, initial exploratory factor analysis revealed 6 distinct factors. The highest (absolute) factor loading for each item is presented underlined and in bold. Loadings with values less than 0.3 are not reported.
Table 4.
Six-Factor Solution* for the PAR-PRO Participation Items
| Item | Factor I | Factor II | Factor III | Factor IV | Factor V | Factor VI |
|---|---|---|---|---|---|---|
| Work | .600 | |||||
| School | .544 | |||||
| Volunteer | .300 | .652 | ||||
| Cooking | .774 | |||||
| Light | .767 | |||||
| Housework | ||||||
| Heavy | .564 | .515 | ||||
| Housework | ||||||
| Caregiver | .552 | |||||
| Finance | .526 | .348 | ||||
| Shopping | .756 | |||||
| Yard work | .381 | .539 | ||||
| Hobbies | .508 | |||||
| Social in | .758 | |||||
| Social out | .817 | |||||
| Travel | .504 | .360 | .318 | |||
| Travel | .440 | .558 | ||||
| Travel | .587 | −.362 | ||||
| Spiritual | .682 | |||||
| Public | −.746 | |||||
| Transportation | ||||||
| Driving | .484 | .394 | .460 | |||
| Intimate | .334 | .629 | ||||
NOTE. Items with factor loadings <.3 suppressed; for each item, the factor loading with the highest absolute value is presented in bold.
Principal component analysis; varimax rotation with Kaiser normalization.
Although 6 potential factors were identified using the eigenvalue criterion, another standard for factor interpretation is to use factors with 3 or more factor loadings.26 Using this approach, factor loadings of 0.5 or greater were identified; though only the first 4 factors are interpretable using this criterion (see table 4). Factor I had highest loadings for items assessing cooking, light housework, and shopping, and lower loadings for heavy housework, and management of money and home finances. This factor appears to reflect participation in "domestic management" activities. Factor II had the highest loadings on items reflecting socialization both outside of and within the home, and lower loadings on items indicating involvement in hobbies and arts and crafts and travel. This factor likely reflects a "socialization" factor. Factor III is less easily interpretable and has weaker loadings than either of the 2 previous factors, but may reflect "physical vigor," with loadings on items reflecting participation in sports/exercise, caregiver activities, and yard work. Factor IV appears to reflect participation in "generative activities," at least to the extent that it indicates participation in work or school activities. The item assessing participation in events such as attending movies or concerts also contributes to this factor.
Factor loadings across these 4 factors were generally moderate and cumulatively these factors accounted for 44.4% of the variance in the data. These findings and those from the Rasch analysis suggest that the PAR-PRO instrument is primarily a unidimensional measure of participation, with weaker subfactors secondary to this primary construct.
Discussion
The 20-item PAR-PRO instrument of home and community participation, using a 3-level scoring system, was found to have good internal consistency, evidence of an underlying unidimensional participation construct, and an adequate range of endorsed frequency. The PAR-PRO participation instrument was shown to have a modest but statistically significant negative relationship with age. Although the PAR-PRO participation instrument was designed to minimize any age bias, it was expected that older individuals would have lower participation than younger people. Previous work using the CIQ in a sample of people with brain injury demonstrated a similar negative relationship between age and community integration.4 Such findings reflect the view that younger people tend to be more involved in activities, especially activities based in the community, than older people. In contrast to the age effect, there were no sex differences on the PAR-PRO total rating. Others have reported overall community participation scores to be similar between men and women.4
A comparison of PAR-PRO participation ratings among different impairment groups showed that people with orthopedic conditions tended to score higher than people with either stroke or neurologic conditions, with and without adjustment for age. One possible interpretation is that people with orthopedic conditions were not as limited in their functional ability as those with stroke or neurologic conditions. This interpretation suggests that the individuals with orthopedic conditions may have been healthier prior to admission for inpatient rehabilitation than those in the other groups. This hypothesis could be evaluated in future studies.
The PAR-PRO participation instrument was designed to reflect a broad, unidimensional participation construct. Rasch analysis and measurement of internal consistency seem to confirm this goal. Factor analysis suggested that subfactors, such as those reflecting domestic management and socialization, may be present. These subfactors should be viewed as tentative and require further research, particularly in younger populations or in populations without disability, to determine if they can be replicated.
A potential floor effect was identified, particularly in the area of social participation. This floor effect may be an artifact of the sample and the relatively older age of most participants (mean, 74y). This is an area that requires further study, specifically an evaluation of the PAR-PRO instrument with a younger sample and with a nondisabled sample. This potential floor effect should be reduced if the PAR-PRO instrument were used along with the FIM instrument. Though, the effectiveness of using both instruments together in people with disability needs to be examined.
No ceiling effect for the PAR-PRO instrument was observed in the current sample. Participation in several areas including involvement in school or educational activities was infrequent in the current sample. These items were retained in the instrument because they may have relevance to people who are younger or at an earlier stage in role participation.
Our goal was to develop an instrument related to the ICF domains of participation that was brief, practical and general enough for broad application. The breadth and complexity of the ICF domains were difficult to operationalize and some specific aspects of the ICF may not be well-represented in the PAR-PRO. For example, within the major life area of work and employment, the ICF has subdomains reflecting apprenticeship, acquiring, keeping and terminating a job, remunerative employment, and nonremunerative employment. We chose to summarize these subdomains with a single item reflecting the frequency that the individual worked in the previous year. Creating broad as opposed to narrow items supports the PAR-PRO's use as a practical general measure of home and community participation, but may limit its application where very specific participation information is required (eg, for use in detailed vocational planning or counseling).
Study Limitations
The results from this initial examination suggest that the PAR-PRO instrument has potential as a brief practical measure of participation as defined in the ICF. We found the items appear to measure a unidimensional construct of participation and demonstrate adequate basic psychometric properties. Substantial additional research is necessary to establish the PAR-PRO as a clinically useful instrument to assess participation. A limitation of this study was the age and nature of the sample. The average age of 74 years is consistent with the population of patients receiving inpatient medical rehabilitation in the United States. The older age of the sample did not allow us to determine patterns for participation for a broad range of persons with disabilities. For example, we need to know more about the participation patterns related to work, school and other activities commonly engaged in by younger persons with and without disabilities. As noted above, the potential floor effect may be an artifact of the sample. Social participation activities may be reported differently by a younger sample. An important next step in research using the PAR-PRO instrument will be to replicate the findings reported here with younger participants. Another limitation and important topic for future research is the impact type of disability or impairment will have on participation. Our ability to analyze participation patterns across different disability sub-groups was limited by the sample size and characteristics (eg, age). It will be important in future research to examine participation patterns in persons with disabilities not well represented in the current sample (eg, persons with SCI or TBI).
We did not find any difference in participation patterns reported by patients versus those reported by a proxy. Our ability to examine this topic was limited, however, by the small number of proxy respondents (n=34). Additional research with a direct focus on the question of the equivalency of patient versus proxy respondent ratings is needed to clarify this issue.
Finally, the usefulness of the PAR-PRO instrument will be substantially enhanced by providing information on the participation patterns of persons without disabilities. Information on response patterns from a large heterogeneous sample of persons without disabilities will help to define the construct of participation and verify the participation subdomains reported in this investigation.
CONCLUSIONS
Patient-centered measures, such as satisfaction and participation, are increasingly being required by accreditation agencies, consumers, and third-party payers, as quality indicators of best practices.2,3 Medical rehabilitation has a history and tradition of focusing on person-based outcomes rather than narrow organ-based measures. Translating the person-based philosophy of medical rehabilitation to address current practice will require the development and testing of new instruments and assessment methods. The PAR-PRO instrument has the potential to help increase our understanding of participation in persons with disabilities and their families. Developing clinically useful measures of participation is an important challenge facing rehabilitation professionals and researchers.
APPENDIX 1: ACCREDITATION ASSESSMENT FORM
Reprinted with permission of UDSMR.
Footnotes
Suppliers
a. SPSS Inc, 233 S Wacker Dr, 11t Fl, Chicago, IL 60606.
b. Winsteps, PO Box 811322, Chicago, IL 60681–1322.
Supported by the American Heart Association (grant no. 0270045N), the National Institute of Child Health and Human Development, National Institutes of Health (NIH) (grant no. K01 HD046682), and National Institute on Aging, NIH (grant no. K02AG019736).
No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit upon the authors or upon any organization with which the authors are associated.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.World Health Organization. International classification of impairments, disabilities and handicaps. Geneva: WHO; 1980. [Google Scholar]
- 2.World Health Organization. International classification of functioning, disability and health. Geneva: WHO; 2001. [Google Scholar]
- 3.Commission of Accreditation of Rehabilitation Facilities. 2003 medical rehabilitation standards manual. Tucson: CARF; 2002. [Google Scholar]
- 4.Willer B, Linn R, Allen K. Community integration and barriers to integration for individuals with brain injury. In: Finlayson MA, Garner SH, editors. Brain injury rehabilitation: clinical considerations. Baltimore: Williams & Wilkins; 1994. pp. 355–75. [Google Scholar]
- 5.Willer B, Ottenbacher KJ, Coad ML. The Community Integration Questionnaire. Am J Phys Med Rehabil. 1994;73:103–11. doi: 10.1097/00002060-199404000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Whiteneck GG, Charlifue SW, Gerhart KA, Overholser JD, Richardson GN. Quantifying handicap: a new measure of long-term rehabilitation outcomes. Arch Phys Med Rehabil. 1992;73:519–26. [PubMed] [Google Scholar]
- 7.Goranson TE, Graves RE, Allison D, La Freniere R. Community integration following multidisciplinary rehabilitation for traumatic brain injury. Brain Inj. 2003;17:759–74. doi: 10.1080/0269905031000088513. [DOI] [PubMed] [Google Scholar]
- 8.Esselman PC, Ptacek JT, Kowalske K, Cromes GF, deLateur BJ, Engrav LH. Community integration after burn injuries. J Burn Care Rehabil. 2001;22:221–7. doi: 10.1097/00004630-200105000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Kaplan CP. Community Integration Questionnaire for patients with brain tumor: a comparative study. Am J Phys Med Rehabil. 2000;79:243–6. doi: 10.1097/00002060-200005000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Sander AM, Fuchs KL, High WM, Jr, Hall KM, Kreutzer JS, Rosenthal M. The Community Integration Questionnaire revisited: an assessment of factor structure and validity. Arch Phys Med Rehabil. 1999;80:1303–8. doi: 10.1016/s0003-9993(99)90034-5. [DOI] [PubMed] [Google Scholar]
- 11.Dittmar SS, Gresham GE. Functional assessment and outcome measures for the rehabilitation health professional. Gaithersburg: Aspen; 1997. p. 205. [Google Scholar]
- 12.Mellick D, Walker N, Brooks CA, Whiteneck G. Incorporating the cognitive independence domain into CHART. J Rehabil Outcomes Meas. 1999;3:2–21. [Google Scholar]
- 13.Putzke JD, Richards JS. Nursing home residence: quality of life among individuals with spinal cord injury. Am J Phys Med Rehabil. 2001;80:404–9. doi: 10.1097/00002060-200106000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Wood-Dauphinee S, Exner G, Bostanci B, et al. SCI Consensus Group. Quality of life in patients with spinal cord injury—basic issues, assessment, and recommendations. Restor Neurol Neurosci. 2002;20:135–49. [PubMed] [Google Scholar]
- 15.Walker N, Mellick D, Brooks CA, Whiteneck GG. Measuring participation across impairment groups using the Craig Handicap Assessment Reporting Technique. Am J Phys Med Rehabil. 2003;82:936–41. doi: 10.1097/01.PHM.0000098041.42394.9A. [DOI] [PubMed] [Google Scholar]
- 16.Johnston MV, Groverover Y, Dijkers M. Community activities hand individuals’ satisfaction with them: quality of life in the first year after traumatic brain injury. Arch Phys Med Rehabil. 2005;86:735–45. doi: 10.1016/j.apmr.2004.10.031. [DOI] [PubMed] [Google Scholar]
- 17.McColl MA, Davies D, Carlson P, Johnston J, Minnes P. The Community Integration Measure: development and preliminary validation. Arch Phys Med Rehabil. 2001;82:429–34. doi: 10.1053/apmr.2001.22195. [DOI] [PubMed] [Google Scholar]
- 18.Brown M, Dijkers MP, Gordon WA, Ashman T, Charatz H, Cheng Z. Participation objective, participation subjective: a measure of participation combining outsider and insider perspectives. J Head Trauma Rehabil. 2004;6:459–81. doi: 10.1097/00001199-200411000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Reistetter TA, Spencer JC, Trujillo L, Abreu BA. Examining the Community Integration Measure (CIM): a replication study with life satisfaction. NeuroRehabilitation. 2005;20:139–48. [PubMed] [Google Scholar]
- 20.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334. [Google Scholar]
- 21.SPSS. SPSS for Windows, release 11.5. Chicago: SPSS; 2002. [Google Scholar]
- 22.Nunnally JC. Psychometric theory. 2. New York: McGraw-Hill; 1978. [Google Scholar]
- 23.Linacre JM. Winsteps version 3.42: Rasch measurement computer program. Chicago: Winsteps; 2003. [Google Scholar]
- 24.Deutsch A, Fielder RC, Granger CV, Russell CF. The Uniform Data System for Medical Rehabilitation: report of patients discharged from comprehensive medical rehabilitation programs in 1999. Am J Phys Med Rehabil. 2002;81:133–42. doi: 10.1097/00002060-200202000-00010. [DOI] [PubMed] [Google Scholar]
- 25.Wright BD, Masters GN. Rating scale analysis: Rasch measurement. Chicago: Mesa Pr; 1982. [Google Scholar]
- 26.Thurstone LL. Multiple factor analysis. Chicago: Univ Chicago Pr; 1947. [Google Scholar]


