Abstract
This study was designed to replicate and extend previous research on posttreatment responding by identifying trajectories of change on the basis of an empirical classification strategy and to examine predictors of those change trajectories identified. Treatment response was examined for 232 adolescents who received outpatient family and/or cognitive behavioral interventions for substance use disorders who participated in one of two randomized controlled trials evaluating family and cognitive behaviors interventions in an outpatient treatment setting. Cluster analysis was used to identify, empirically, homogeneous groups of individuals who display common internally consistent patterns of change over the course of treatment.
1. Introduction
Controlled clinical trials evaluating treatments for adolescent substance use disorders have yielded consistent empirical support for the efficacy of family and cognitive behavioral interventions (Dennis et al., 2004; Kaminer & Burleson, 1999; Kaminer, Burleson, Blitz, Sussman, & Rounsaville, 1998; Liddle et al., 2001; Waldron et al., 2001; Wagner, Brown, Myers, Monti, & Waldron, 1999). Across studies, however, reductions in adolescent substance use vary widely and substantial individual variability in patterns of change has been found. Moreover, fewer than half of treated youth maintain abstinence during the year following treatment. Relapse rates reported in the literature have ranged as high as 93%, with evidence that only 7-8% of treated adolescents maintain abstinence over extended follow-up periods (Brown, Vik, & Creamer, 1989; Brown, D’Amico, McCarthy, & Taper, 2001; Brown, Myers, Mott, & Vik, 1994; Catalano et al., 1991; Friedman, Glickman, & Morrissey, 1990; Godley et al., 2001; McKay & Buka, 1994; Spear, Ciesla, & Skala, 1999; Waldron et al., 2001; Winters, 1999). Such high rates of relapse for adolescent substance abuse treatment are particularly disappointing in light of significant and clinically meaningful reductions in substance use from pre- to post treatment (Deas & Thomas, 2001; Ozechowski & Liddle, 2000; Stanton & Shadish, 1997; Waldron, 1997; Waldron & Kaminer, 2004; Williams & Chang, 2000). These variable outcomes underscore the need for greater understanding of different patterns of treatment responding among adolescents with substance use disorders. To the extent that we can identify individual change profiles shared by subgroups of individuals and we can identify predictors of such profiles, our understanding of how to modify and fit existing treatments to specific groups of adolescents could be enhanced (Deas, Riggs, Langenbucher, Goldman, & Brown, 2000; Winters, 1999).
The present study was designed to examine individual differences in profiles of change that are likely to occur over the course of adolescent substance abuse treatment, building on previous research on patterns of change across the course of treatment that has begun to emerge in the literature (Waldron, Turner, & Ozechowski, in press). For example, Spear and her colleagues (1999) examined post-treatment drug use for 113 adolescents who had participated in a 28-day residential drug abuse treatment program. They found that 19% of youth were either abstinent or had only isolated incidents of use at a 12-month post-treatment follow-up, while 20% were using 1-3 times per month and 61% had returned to using at baseline levels of 1 or more times per week. Unfortunately, the investigators did not differentiate among levels of relapse or patterns of change over time.
In another study, Maisto and his colleagues (2001) examined diagnostic status and post-treatment functioning of 131 youth treated for alcohol abuse and dependence. These investigators classified youth as abstainers, drinkers without diagnosis, drinkers diagnosed as alcohol abusers, and drinkers diagnosed as alcohol dependent. Using this diagnostic taxonomy, they were able to differentiate between nonproblem and problem use. They showed that more that half of the youth in their sample were no longer met criteria for an alcohol diagnosis 12 months after treatment. Within this group, only one third was abstaining. Thus, a sizable proportion of youth who previously met criteria for alcohol use disorders were now drinking, but at nonproblem levels. As in the Spear et al. (1999) study, these findings support the notion that treatment response varies across individuals. In neither study, however, were trajectories of change across the follow-up period not examined.
Taking a somewhat different approach, Brown and her colleagues (2001) classified 162 adolescents treated for alcohol use disorders into categories conceptually derived to represent patterns of treatment response over a 4-year period. They classified the substance use of almost all of the youth (98%) into five operationally defined, mutually exclusive categories: abstainers (10%), users with 1-7 occasions per month (8%), slow improvers or those who failed to abstain initially, but significantly reduced their use or became abstinent (10%), youth who initially improved but became worse or relapsed over time (27%), and continuous heavy users with 18-25 use episodes per month (48%). Their findings highlight the variability in substance use over time and further underscore the disadvantages inherent in a “one size fits all” approach to intervention.
Across the three studies, generally consistent patterns of improvement and maintenance of treatment gains and patterns of relapse were observed. Important issues raised by these studies, however, is whether or not the different categorizations of post-treatment responding are valid and whether or not the response patterns are distinct. Youth in each of the three studies were classified conceptually on an a priori basis rather than the classification being empirically driven. Possibly, the differences between subgroups could have been produced by a limited number of individuals in each subgroup. Thus, while these three studies set the stage for further investigation of differential treatment response, one of the next steps in this research progression, and the goal of the present study, is to examine an empirically based classification of profiles of change.
The research described above also highlights the need for a better understanding of pre- and post-treatment predictors of different patterns of treatment responding, especially those associated with trajectories reflecting treatment failure, in order to inform the tailoring of treatments to particular profiles of change (Latimer et al., 2000a; Wagner et al., 1999). Brown and her colleagues (2001) suggested that differing profiles of post-treatment transitions in use reflect both pretreatment risks for substance use and post-treatment environmental and developmental factors. Risk and protective factors associated with overall treatment outcome include pretreatment substance use, deviant behavior, peer influence, family relationships, and type and intensity of treatment (Broome, Joe, & Simpson, 2001; Brown et al., 1989; Coatsworth et al., 2001; Crowley et al., 1998; Dobkin et al., 1998; Latimer et al., 2000a; Latimer et al., 2000b; Orwin, Ellis, Williams, & Maranda, 2000). These variables may predict different trajectories of change as well. If so, specific treatment regimens or selected intervention strategies that target protective factors predictive of better outcomes and that anticipate risks as they emerge over time could be offered to subgroups of youth who appear to be on different trajectories of recovery.
The purpose of this study was two-fold: (1) to replicate and extend previous research on post-treatment responding by identifying trajectories of change on the basis of an empirical classification strategy and (2) to examine predictors of those change trajectories identified. The study represents an extension of our previous work (Waldron et al., in press) using cluster analysis with a larger sample of youth to classify treatment response. Cluster analysis is an approach used to identify, empirically, relatively small number of distinct, homogeneous groups of individuals who display common internally consistent patterns of change over the course of treatment. Based on findings from previous studies and from our previous cluster analysis research (Waldron et al., in press), we examined several key adolescent problem behaviors, including depression, delinquency, aggression, as hypothesized predictors of adolescent change profiles. Treatment response was examined for adolescents who had substance use disorders, and the samples were pooled across two clinical trials in which adolescents received family and/or cognitive behavioral interventions in an outpatient treatment setting.
2. Method
2.1. Participants
The current examination is based on data collected two randomized clinical trials of drug abuse treatment efficacy conducted at the Center for Family and Adolescent Research in Albuquerque, New Mexico. Findings from the first trial were based on 129 adolescents (96 boys, 24 girls), aged 13-18 years (M=15.6; SD=1.1), who received individual-, group-, or family-based outpatient treatment for marijuana abuse and dependence. Baseline levels of substance use, based on percent days of use during the previous three months was 56.85 for marijuana, 6.38 for alcohol, 62.84 for tobacco, and 59.95 for percent days on which any substance (excluding tobacco) was used. The Preliminary findings from this study have been previously reported in the literature (Waldron et al., 2001). The second trial replicated the procedure in the earlier study, but targeted 117 adolescents (92 boys, 25 girls), aged 13-19 (M=16.3; SD=1.3), who had an alcohol use disorder. In this study, percent days of baseline substance use during the previous three months was 46.87 for marijuana, 17.65 for alcohol, 61.18 for tobacco, and 54.50 for percent days on which any substance (excluding tobacco) was used. The final sample for this study consisted of 237 adolescents, with 45% Hispanic American, 41% Anglo American, 6% Native American, and 8% of mixed or other ethnicities. Waldron et al. (2001) study provides a more detailed description of the recruitment procedures and inclusion/exclusion criteria used in both trials.
2.2. Procedure
All adolescents referred to the center, with their families, completed an intake interview to identify clinical concerns and to determine study eligibility. Eligible families were then scheduled for a pretreatment assessment. Consent/assent for participation was obtained at the beginning of the assessment session. The assessment battery was approximately 4-5 hours long. After the initial assessment, adolescents were randomly assigned to one of four treatment conditions: Functional Family Therapy (FFT), individual cognitive behavioral therapy (CBT), a combined or integrated treatment condition that involved both combination of FFT and CBT, or a psycho-educational group (see Waldron et al., 2001 for a detailed description of the interventions). The only difference between the interventions across the two clinical trials was in the combined treatment condition. In the first trial, youth in the combined condition received 24 sessions, compared to 12 sessions in each of the other interventions. In the second trial, all interventions were 14 sessions in length. For both studies, follow-up assessments were conducted at post-treatment and two additional follow-up assessments, one occurring at 7-8 months and one occurring at 18-19 months following the initiation of treatment. Families were compensated up to $390 for completing the 4 assessment sessions across both studies.
2.3. Measures
2.3.1. Substance use
The primary substance use measure was percent days of marijuana use, obtained for all adolescents and parents using the timeline follow back interview method (TLFB; Sobell & Sobell, 1982; 1995). For all participants, substance use at pretreatment was examined for the previous 90-day period. At the post-treatment and first follow-up assessment, the calendar period for the TLFB interview extended back to the date of the last assessment. For the second follow-up, substance use was obtained for the last 90 days because of the long lag time between the two follow-up assessments. Additional measures from the TLFB provided estimates of alcohol use, tobacco use, and all substances used (excluding tobacco).
2.3.2. Other measures
Collateral reports, urine drug screens, and other measures were obtained to examine convergent validity of the TLFB. Collateral TLFB reports, a method well established in the addictions field (Needle, McCubbin, Lorence, & Hochhauser, 1983; Sobell & Sobell, 1982; 1995), were obtained from parents and siblings of the target adolescent. In addition, adolescents provided urine specimens at the project site, with a nine-panel screen used for the urinalyses. The screens were carried out by immunoassay (e.g., EMIT, ADX) and all positive screens were confirmed by gas chromatography/mass spectroscopy (GC/MS). These auxiliary substance use measures have been used to examine convergence with self-report data collected from adolescents on the TLFB (see Waldron et al., 2001).
Other measures obtained across the two trials were used to identify predictors of trajectories of change on the primary dependent measure of substance use. These measures included adolescent problem behaviors assessed through parent and youth report. Measures of adolescent behavior were obtained using the parent-report Child Behavior Checklist (CBCL) questionnaire and the Youth Self Report (YSR), the youth-report version of this questionnaire (Achenbach & Edelbrock, 1982. These instruments provide standardized formats for assessing child behavior across a range of problem areas. These scales have been widely used in previous research and have well-documented psychometric properties. In addition, the Beck Depression Inventory (BDI; Beck, Ward, Mendelson, Mock, & Erlbaugh, 1961) was used to assess the occurrence and severity of depressive symptoms. Reliability and validity of the BDI have been established in hundreds of studies with adults and adolescents (Beck, Steer, & Garbin, 1988; Roberts, Lewinsohn, & Seeley, 1991).
2.4. Estimating Incomplete Data for Trajectory Analysis
An important problem in assessing change trajectories arises when some of the research participants have not provided complete data across all assessment points.1 In this study, clients who completed all or part of the intake assessment but did not return for the first treatment session were regarded as not having begun treatment. Outcomes for clients who attended one or more treatment sessions were included in the analyses.
We used multiple imputation procedures to estimate missing scores (Schafer, 1997; Schafer & Graham, 2002). Briefly, multiple imputation is an iterative procedure that simulates values for missing data based on non-missing data. In multiple imputation, estimates for missing scores are initially obtained via maximum likelihood regression. The regression coefficients are then used as starting values for obtaining new and more precise estimates in the subsequent imputation. Each imputation yields a complete data set free of missing values. This iterative estimation procedure continues until differences between sets of missing data estimates become trivial (usually 5-10 iterations). Once the estimation process is complete, the data analysis is conducted separately on each imputed data set yielding a separate set of parameter estimates for each data set. The parameter estimates across imputations are then collapsed into a single set of parameter estimates. Standard errors for each estimate are computed based on the between-imputation variability. The multiple imputation procedures were implemented using PROC MI and PROC MIANALYZE of SAS version 8.
2.5. Cluster Analysis Procedures
Cluster analysis permits the classification of individuals who are assessed on a common set of dependent measures into similar appearing groups (Aldenderfer & Blashfield, 1984; Everitt, 2001). Generally speaking, cluster analysis is a family of procedures for identifying homogenous subgroups of individuals based on response patterns across a set of variables. This procedure has been widely used across many research disciplines to create classification systems or taxonomies. In adolescent research, cluster analysis has been used to identify longitudinal patterns in the development of high-risk behavior (Gorman-Smith, Tolan, Loeber, & Henry, 1998; Wills, McNamara, Vaccaro, & Kirkey, 1996), as well as in response to clinical intervention (Hanish & Tolan, 2001). An important goal of the procedures is to create these groups such that the members within a group have very similar response profiles on the dependent measures while the groups are distinct from each other in response profiles. One of the major challenges in cluster analysis is to establish the number of groups that are needed in order to provide an optimal classification of individuals into homogeneous groups. If the number of groups is too small, then each group will be composed of heterogeneous rather than homogeneous profiles. Alternatively, if the number of groups is too large, the sample sizes in each group may be very small and unreliable so that the classification can not be replicated in other samples.
Cluster analysis often involves two procedures called hierarchical clustering and k-means clustering. The hierarchical clustering procedure is useful as a preliminary step in determining the number of clusters that may be required to establish homogeneous groups of individuals. The first step in a hierarchical cluster procedure is to create a “proximity” matrix that represents the similarity of each individual to all other individuals. One commonly used index is called Euclidean distances, and it is created for each pair of individuals. The distances between the individuals on each dependent measure are squared and added together. Next, the square root of this value is calculated.2
The next step in hierarchical clustering is to insert these between pair distances into a “proximity” matrix where both the rows and columns represent all of the individuals, and the cell entries represent the Euclidean distance between the individual represented by the row and the individual represented by the column. This matrix is similar to a mileage chart which represents all possible distances between pairs of cities. We can then rearrange the rows and columns so that the adjacent columns have individuals with the smallest distance to each other. We can continue this sorting strategy so that all similar individuals appear in adjacent columns and rows. Suppose that several homogeneous groups exist in our proximity matrix. All of the individuals in each homogeneous group would appear in adjacent columns and adjacent rows. The typical distance score among pairs in the first group would be small while the distance scores with anyone outside of the group would be large.
Typically the second analysis phase builds on the first phase and it is called the k-means cluster procedure. In this procedure, the investigator starts with an assumption about the number (k) of clusters that are appropriate for the classification task. Sometimes, investigators can use the results of the hierarchical clustering criteria, but they also may have theoretical or practical reasons for selecting a specific number of groups to estimate. The k-means procedures can be viewed as a variant of analysis of variance procedures in which the program tries to sort individuals into “k” groups so as to minimize the within cluster variance across all dependent variables and to maximize the between group variance across all measures. The program keeps rearranging each person’s group membership so that the within group variance is minimized by the specific allocation of individuals to groups. A descriptive index that reflects the effectiveness of the sorting procedure is an “F” test computed from the ratio of the within to between cell variances. When the procedure is successful, all of the members of each group will have similar response profiles across the dependent variables, and these response profiles will be different from those obtained for other groups.
Morral, Iguchi, Belding, and Lamb (1997) provide a valuable set of guidelines for evaluating cluster solutions involving treatment response data. According to Morral et al. (1997), the first criterion for evaluating cluster solutions is cluster size. If the investigator’s choice of k is too small, then each group will be composed of heterogeneous profiles, and this heterogeneity will inflate the within cell variability. The investigator may want to evaluate this possibility by repeating the clustering procedure using k+1 groups instead of k groups. If the k+1 solution creates more homogeneous groups, the within group error group will be substantially smaller for the k+1 groups solution as compared to k groups solution. After determining that the correct number of groups has been achieved, a convenient procedure for describing each cluster is to calculate the means and standard deviations of each cluster on each dependent variable. If the investigator has chosen too large a value for k, the number of individuals within a cluster may be very small, yielding unreliable clusters. The investigator can evaluate this hypothesis by estimating a solution with k-1 groups. If the within group error terms do not substantially increase, and the number of individuals per group is greater than 10, then the k-1 solution may be more appropriate and reliable than the k solution. A second evaluation criterion utilized by Morral et al. (1997) is face validity. That is, differences between cluster profiles should be readily interpretable on theoretical and clinical grounds without any “tortuous reasoning (p. 675).” A third evaluation criterion is discriminability, which means that cases assigned to separate clusters should have significantly different responses on variables theoretically related to cluster membership.
Once an appropriate cluster solution has been achieved, a convenient technique for describing each cluster is to calculate the means and standard deviations of each cluster on each dependent variable. However, the discriminability of cluster solutions can be assessed using a variety of standard techniques for studying differences between groups (e.g., t-tests, MANOVA) for predicting the probability of group membership (e.g., discriminant function analysis, logistic regression).
3. Results
As in Waldron et al. (in press), the various treatment interventions for the combined sample produced different average or group-level profiles of change similar to those found in Waldron et al. (2001). Overall, significant reductions in substance use from pre- to post-treatment were found for marijuana and alcohol use and overall substance use (excluding tobacco), but not for tobacco use. However, the findings revealed substantial heterogeneity of treatment outcomes and variability in change profiles both within and between profiles. We will now focus upon analyses examining the individual variability in these change profiles and predictor variables that discriminate the profiles.
3.1. Individual Profiles of Change
For cluster analysis to identify individual differences in patterns or profiles of change in substance use, a hierarchical clustering procedure with the four marijuana use assessment points as dependent variables (i.e., baseline, post-treatment, and follow-ups 1 and 2) was initially performed. The hierarchical solution suggested that 3, 4, or 5 group solutions might provide good classification profiles for the substance use. Based on theory and on prior studies (e.g., Brown et al., 2001; Latimer et al., 2000b; Maisto et al., 2001), we initially chose a four groups solution in our k-means procedure: continuous low use, gradual improvement, continuous heavy use, and gradual deterioration. Although prior research did not use cluster analysis procedures, the investigations provided a theoretical rationale for expecting four profiles of change, rather than the three- or five-cluster solutions.
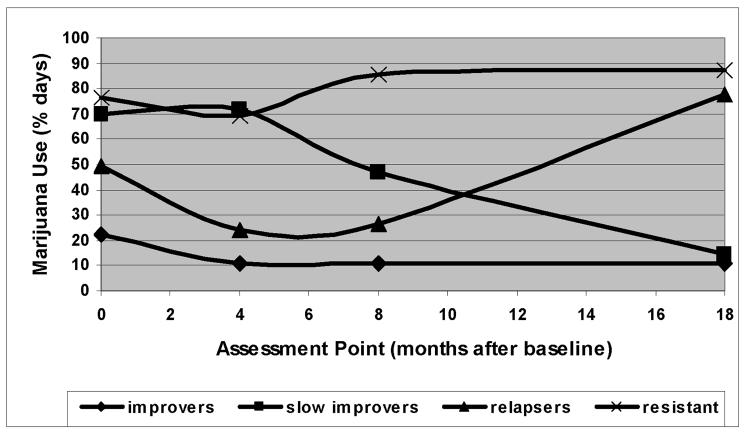
Using the reasoning of Morral et al. (1997) to evaluate our proposed solution, we determined that each of our clusters was of a sufficient size (at least 15 individuals) to provide a reliable estimate of the cluster. Moreover, the cluster groups made theoretical sense and were consistent with prior classification solutions. Our initial four group cluster analysis (see Figure 1) provided evidence of change profiles in marijuana use that are somewhat similar to profiles previously described: continuous heavy use (24.8%), rapid improvement and continuous low use (36.8%), rapid improvement followed by deterioration (24.8%), and gradual improvement (13.7%). These proportions were very similar to those found in the smaller sample of Waldron et al. (in press).
Figure 1.
Comparison of four clusters groupings for marijuana use.
A third criterion for evaluating a cluster solution is discriminability of the clusters. One method for evaluating group discrimination is to use a repeated measures analysis of variance (ANOVA) with cluster group membership as the independent variable and the four time points as dependent variables. Overall, marijuana was the predominant drug of abuse, even among youth with a co-occurring alcohol use disorder. Not surprisingly, then, strong discrimination was found for marijuana use alone (see Figure 1). The repeated measure ANOVA with cluster group membership as the independent variable and marijuana use at the four time points as dependent variables revealed a significant effect (F(3,227) = 424.65, p < .000, eta 2 = 0.85). The Time main effect was not significant: F(3,681) = 1.04, p <.38, eta 2 =0.005. The Time × Cluster interaction was statistically significant, F(9,681) = 38.98, p < .000, eta 2 =0.34.
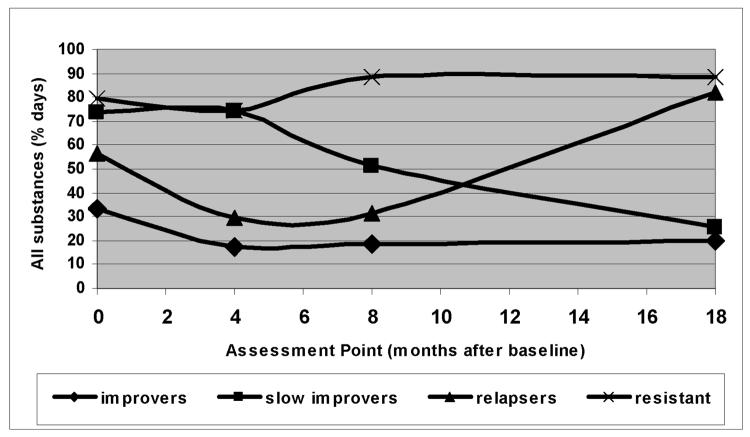
Using the clusters definition for each adolescent on the marijuana dependent variable, we also examined between cluster differences on other indicators of substance use. First, we examined the composite substance use measure, which assessed the percent of days that any substance was used (excluding tobacco). We performed a 4 (Cluster identification) × 4 (Time) repeated measures analysis of variance. The results indicated that the main effect for between cluster variable were highly significant on the all substance use measure, F(3,227) = 272.70, p < .000] as well as the effect size estimate (partial eta2 = 0.78) indicated that a four group cluster solution provided a very strong discrimination among the individuals. Although the main effect for time was not significant (F < 1.0), the Time × Cluster interaction was significant, F(9,681) = 35.98, p < 0.000, eta 2 = 0.32. The pattern of results is quite similar to the marijuana dependent variable. Thus, the four group solution appears to be sensitive to the individual variability in responding during the post-treatment periods.
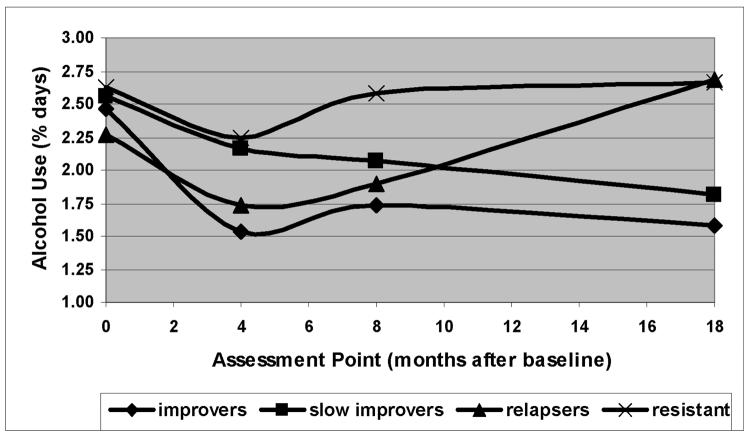
Because our sample consisted of youth referred for two clinical trials, one focusing primarily on marijuana users and the other on youth who had an alcohol use disorder in addition to their other drug use, we replicated the initial four group cluster analysis for alcohol use, in order to determine the discriminability of the clusters for this measure. We again used the marijuana cluster definition for each individual as the independent variable, and we compared the clusters, over time, for the alcohol dependent variable. The results indicated that the main effect for Cluster identification was also statistically significant, F(3,227) = 9.76, p <.000, eta 2 =0.114. Again, the Time main effect was not significant (F < 1.0), but the Time × Cluster effect was significant F(9,681) = 5.61, p < .000, eta 2 =0.069. Again, the profile pattern is quite similar to the marijuana use pattern. Alcohol use was a specific intervention target in one of the two clinical trials, although average alcohol use was substantially lower than marijuana use in both trials. Nevertheless, the findings for alcohol use replicated those for overall substance use and for marijuana use alone (see Figure 3).
Figure 3.
Comparison of four clusters groupings for alcohol use.
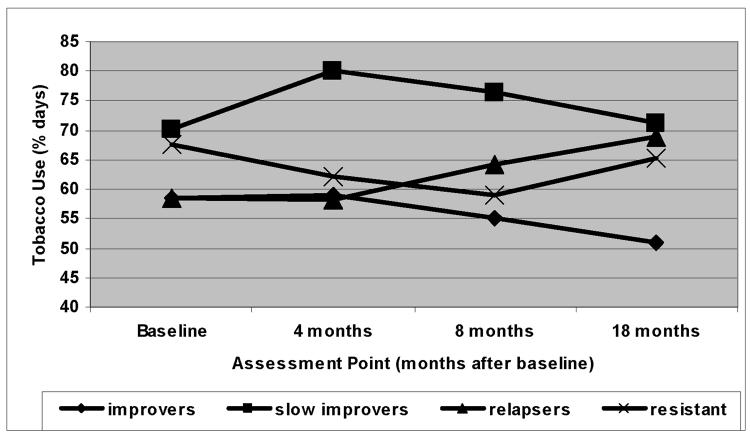
Tobacco use was not an intervention target in either clinical trial. However, the cluster groups for tobacco were also quite similar to those for substance use (excluding tobacco), marijuana use, and alcohol use (see Figure 4). A repeated measures analysis of variance with cluster group membership as the independent variable and tobacco use at the four time points as dependent variables revealed a significant multivariate F (F(3,227) = 2.72, p < .045, eta 2 = 0.035). In addition, the Time × Cluster effect was significant (F(9,681) = 1.99, p <.038, eta 2 = 0.026).
Figure 4.
Comparison of four clusters groupings for tobacco use.
We recognized that the differences in profile patterns might reflect either individual characteristics of the youths and their families or the response profiles might reflect different treatment conditions. To evaluate these possibilities, we examined the occurrence of the different profiles with our three types of treatment interventions (i.e., Family, individual CBT, or Group). The results indicated that the “no change” trajectory occurred in 20% of the youths for the CBT condition and 21% in the Group condition, and 17% in the FFT condition, and 40% of the IBFT condition. The “relapse” trajectory occurred in 18% of the CBT group, 16% of the Group condition, and 28% in the FFT condition, and 24% of the IBFT condition. Approximately 35% of the youths in each condition displayed the quick response profile and 20% displayed the gradual improvement profile. The present findings provide empirical validation for prior classification research and suggest that within each of the treatment conditions youth have different profiles of change.
3.2. Cross-validation of the Trajectories on Other Process Measures
One important concern about cluster analysis procedures is that the decision about the number of solutions to be used in a k-means procedure is somewhat arbitrary. To evaluate the adequacy of a proposed solution, additional criteria should be employed. First, we required that each of our groups identified in the cluster analysis procedure must have at least 10 individuals in order to have an accurate estimate of the means and standard deviations for each dependent measure in the cluster.
To evaluate the validity of our solution, then, we assessed differences among the clusters on other measures that should be related to the classifications. For each family, the primary care giver (usually the mother) and the adolescent were assessed at baseline on the Beck Depression Inventory (BDI; Beck et al., 1961) and the Child Behavior Check List (CBCL) and the Youth Self Report (YSR) (Achenbach, & Edelbrock, 1982). Using selected measures from these instruments, we compared individuals in the four change profiles to determine whether the pretreatment assessments would discriminate among the different response profiles.
3.2.1. Parent perceptions
Using a one way multivariate analysis of variance (MANOVA), we compared the four marijuana defined profiles on four dependent measures as perceived by the parent on the CBCL: the youth’s aggression, depression, internalizing and externalizing. The differences among profiles in parent reports on the youth, using Wilk’s criteria were not statistically significantly different MVF(9,511) = 0.71, p < 0.70]. Thus, parent reports did not differentiate among the four cluster profiles of substance use.
3.2.2. Adolescent perceptions
Using a one-way MANOVA, we also compared the youths self reported levels of aggression and delinquency on the CBCL as well as the youth’s depression on the Beck Depression Inventory. The results indicated that the multivariate comparison among the four clusters was statistically significant, MVF(9, 518.5) = 2.07, p < .031, eta2 = 0.028. The means for the delinquency dependent variable were significantly different on the delinquency dependent variable, F(3, 228) = 2.58, p < .05, eta2 = 0.033, and the means for this dependent variable are presented in Figure 5. Post hoc, pairwise comparisons among the four clusters indicated that the improving group was statistically significantly lower in self-reported delinquency than the resistant group, (p < .01), or slow improver group, p < .05). Comparisons among other means were not statistically significant.
Figure 5.
Differences between drug change cluster groups on YSR Delinquency scores at baseline.
Note: The improver cluster is statistically significantly different (p < .05) from the resistant group on the delinquency dependent variable.
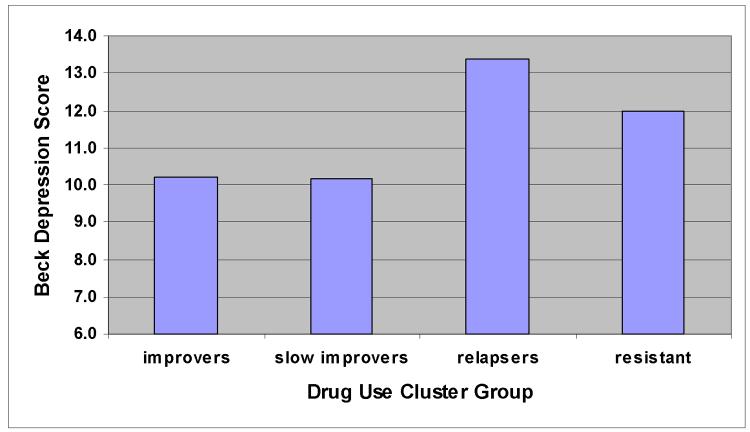
We also examined the BDI scores using gender as a covariate to control for possible differences between boys and girls. The cell means for this dependent variable are reported in Figure 6. Post hoc comparison among the cell means indicated that the relapse group had significantly higher levels of reported depression than the improving group (p < .03) and the slow improving group (p < .05). The comparisons among other means were not statistically significant.
Figure 6.
Differences between drug change cluster groups on Beck Depression scores at baseline.
Note: The relapse cluster is statistically significantly different (p < .03) from the improvers and the slow improvers on the depression measure.
4. Discussion
Among adolescents in treatment for substance abuse or dependence, four distinct response profiles or trajectories of change were identified, with highly consistent findings across marijuana, alcohol, overall substance use, and tobacco. These trajectories, improvers, gradual improvers, relapsers, and continuous heavy users are similar to the conceptually defined treatment response patterns identified by Brown et al. (2001), providing empirical validation for these general profiles of change. The consistency of these categories is remarkable, given the different approaches to classification, the different geographic regions in which the studies were conducted, and the different treatment settings and modalities of each study.
The empirical validation of adolescent change profiles is important because, to date, the empirical support for adolescent substance abuse treatments has been documented almost exclusively at the group level. Recent developments in analytic approaches, such as cluster analysis, have the potential to broaden our understanding of individual patterns of change across treated adolescents. Without the implementation of more advanced analytic strategies to examine differential treatment responding, important effects between individuals that might serve as a guide for tailoring treatments to individual adolescents are likely to go undetected. Such effects could help address critical questions associated with treatment mechanisms, moderators, and long-term outcomes including patterns of relapse.
The four profiles were distributed across the different treatment conditions, suggesting that some youth benefited from each of the treatments and that no one treatment accounted for positive trajectories more than any other. Conversely, within all of the treatments there were youth who improved, but then relapsed and others who failed to respond. One treatment, the intervention combining family and individual CBT, appeared disproportionately over-represented in the non-improvement or continuous heavy use trajectory. This over-representation was not observed in our previous study (Waldron et al., in press). However, this earlier study did not include the sample of youth from the alcohol trial. The key difference between the combined treatment conditions in the two clinical trials was that in the marijuana trial, youth were offered 12 sessions each of family therapy and individual CBT, while in the alcohol trial, youth were offered 14 sessions total. Possibly, the combined condition in the alcohol trial did not provide a sufficient dose of either family or individual treatment and, thus, more youth failed to benefit from the treatment. However, the relatively low dose of CBT did not appear to influence treatment outcomes in the five-session CBT intervention in Cannabis Youth Treatment Study (Dennis et al., 2004) and our CBT modules in the combined intervention were nearly identical to the five-session intervention of Dennis and colleagues. Thus, it may also be possible that an integrated intervention, in which an attempt is made to incorporate theoretically distinct treatments and target a wider array of risk factors (e.g., family dysfunction and maladaptive coping behaviors) into a single course of therapy, may run the risk of introducing interference between the approaches that serves to dilute the potential effectiveness of either treatment.
Compared to the findings of Brown and her colleagues (2001), the proportion of youth in each of the categories of treatment response appeared somewhat different in the present study. For example, Brown et al. (2001) found that 28% of youth ranged from abstainers to slow improvers, compared to 62% in the present study. Relapsers and nonimprovers represented 27% and 48%, respectively, in the Brown et al. study, compared to 24.8% and 21.1%, respectively, in this study. These different proportions could be due to the methodological approaches, the differences in samples, treatments, and settings, or other variables that have yet to be identified. That said, the relapse patterns and lack of treatment responding found in other studies and across interventions in the present study strongly point to the need for improvement in treatments for adolescent substance abuse and dependence if certain subgroups of youth are to receive the help they need.
The finding that depression is predictive of youth who reduce their use in response to treatment, but then relapse suggests that treatments for adolescent substance use disorders do not adequately address the needs of youth with co-occurring disorders. This finding is mirrored in treatment outcome research for depressed adolescents with co-morbid substance use disorders. For example, Rohde and his colleagues found that a history of substance use disorder was associated with longer time to depression recovery for community adolescents in group CBT (Rohde et al., 2001) and that their depression intervention had no detectable effect on recovery rates for either conduct disorder or substance abuse or dependence (Rohde et al., 2004). Moreover, negative affect is one of the frequently reported reasons given for relapse among adolescents treated for substance use disorders (Cornelius et al., 2003). The co-occurrence of substance use and major depressive disorders is also associated with a host of other problems, including higher rates of PTSD (Riggs, Baker, Mikulich, Young, & Crowley, 1995), academic impairment (King et al., 1996); treatment utilization (Wu, Ringwalt, & Williams, 2003), and HIV risk behaviors (Dausey & Desai, 2003), adolescent suicide attempts and completion (Aharonovich, Liu, Nunes, & Hasin, 2002; Lewinsohn, Rohde, & Seeley, 1995; Shafii, Steltz-Lenarsky, Derrick, & Beckner, 1988). Little is known regarding the effective delivery of treatments for youth with co-occurring depression and substance use disorders and increased treatment development efforts are critically need for this group of adolescents. One improvement for youth with this change profile might involve intensified levels of relapse prevention training during treatment (Dobkin et al. 1998; Crowley et al., 1998; Latimer et al., 2000a; 2000b).
Higher levels of delinquency and aggression were associated with failure to respond to treatment. Clearly, for this group of youth, new approaches to treatment are needed. Latimer and his colleagues (2000a) found that, setting pretreatment risk and protective factors aside, post-treatment risk factors did not predict longer term outcomes. Rather, youth who failed to develop protective factors by the end of treatment appeared to be most prone to relapse and hence, perhaps, most in need of continued aftercare. These researchers concluded that protective factors may take time to develop and continuing treatment may foster growth of new psychosocial factors (Latimer et al., 2000a). Thus, even for the non-improving youth who maintain high levels of substance use throughout treatment, increasing treatment intensity and offering continuing care, especially aimed at enhancing protective factors, may foster recovery (Brown et al., 2001; Latimer et al., 2000a; 2000b; McKay et al., 2001; Miller et al., 1997; Orwin et al., 2000). Regular follow-up booster sessions may also be helpful for youth at risk for relapse or for those following a slower change trajectory. Another strategy for helping youth who fail to benefit from treatment is stepped care (Sobell & Sobell, 2000) or adaptive, progressive treatment (Compton & Pringle, 2004). Using this approach, adolescents who do not show an initial response to a standard, cost-effective treatment offered to all youth can be moved into a more intensive treatment or higher level of care. Youth with this change profile also need specific interventions focusing on smoking cessation. Without overtly targeting tobacco use, youth are unlikely to succeed in abstaining from tobacco use (Myers, 2001). This is important because tobacco use remains a critical public health issue that has been predictive of a host of health problems over the developmental life span (Myers & Brown, 1994; USDHSS, 1994). The regular smoking patterns in this sample indicate that the addictive properties of nicotine have taken effect.
Research on mechanisms of change in adolescent treatment may also provide some clues for understanding the relationship between client and therapist behaviors during therapy sessions and positive trajectories of change (Robbins, Alexander, Newell, & Turner, 1996; Robbins, Alexander, & Turner, 2000; Waldron, Turner, Barton, Alexander, & Cline, 1985). For example, some studies have found support for the link between the improvements in family functioning resulting from family therapy and subsequent reductions in adolescent problem behavior (Huey, Henggeler, Brondino, & Pickrell, 2000; Eddy & Chamberlain, 2000), although similar links for substance abuse treatments have yet to be established (Ozechowski & Liddle, 2000; Szapocznik et al., 1989; Waldron, 1998). Other research suggests that youth may be learning skills in therapy that they are gradually successful in implementing over time (Myers & Brown, 1990; Myers, Brown, & Mott, 1993). Observational research on therapeutic processes associated with improvement, relapse, or failure to respond to substance abuse treatment holds the potential to inform how mechanisms of change may vary for different subgroups of youth. Such research could also shed light on the contexts and circumstances under which specific interventions are most appropriate and could be used to guide clinicians regarding the sequencing or timing of specific interventions (Ozechowski & Liddle, 2000).
4.1. Limitations
One limitation of the study is that we combined samples across two different clinical trials. Systematic differences between the two samples, such as the relatively higher baseline alcohol use in one trial, could have obscured patterns that might have emerged in a single sample. However, the studies were conducted in the same outpatient treatment program, with considerable overlap in time, and the protocol differences were slight. Moreover, the findings in the present study replicated those found in our smaller study (Waldron et al., in press) and were remarkably similar to the findings of Brown et al. (2001), even though Brown and her colleagues derived their treatment response groups on a theoretical basis rather than using an empirical strategy such as the one used here. These similar outcomes lend more confidence to the current findings. Another limitation is that the present study examined a very limited number of predictor variables in relation to adolescent treatment response patterns. More research is needed to examine a broader range of variables that may discriminate profiles of change, including peer influence, family relationships, engagement in school, and academic functioning.
Further, cluster analysis is a person-centered (rather than variable-centered) technique and is not a true multi-level analysis. Researchers must be mindful of several key limitations and caveats associated with this technique and appreciate that statistical guidelines and criteria for evaluating the accuracy and validity of cluster solutions are not well developed and the potential for subjectivity on the part of the researcher is high. Researchers should not rely on any single cluster solution but rather should develop a range of plausible cluster solutions and conduct supplemental univariate and multivariate tests to assess the internal and external (i.e. predictive) validity of each solution using variables not included in the cluster analysis. Above all, the validity of any cluster solution should be measured against the yardstick of clinical theory and experience.
Ultimately, the study of individual change over time requires a multi-level modeling approach in which individual- and group-level effects can be statistically modeled simultaneously. Individual growth curve modeling is one such approach that is gaining popularity in substance abuse research (e.g., Duncan, Duncan, & Hops, 1998). The multi-level analog of cluster analysis, called longitudinal or growth mixture modeling, is concerned with discovering latent classes (i.e., clusters) of individual growth trajectories which may vary in terms of initial status, rate or shape of change over time, and may be associated with different sets of covariates or predictors (McArdle, & Hamagami, 1996; Muthen, 2001; Muthen, & Curran, 1997; Muthen & Muthen, 2000; Raudenbush & Bryk, 2002; Willett, & Sayer, 1994). For example, these procedures enable the researcher to determine whether change profiles for one clinically targeted behavior (say, family relationships) provide a predictive association to another targeted change profiles (say, drug use changes). We are currently developing latent growth curve models for studying individual trajectories of change in adolescent substance abuse treatment.
4.2. Conclusions
By numerous accounts, the field of adolescent substance abuse treatment is entering a new stage in its development as a science-based clinical discipline (cf. Dennis, Dawud-Noursi, & Muck, 2002). With nearly two decades of experimental research yielding compelling evidence for the overall efficacy of a variety of treatments, the field is now poised to pursue a more diverse and complex array of questions concerning the components, processes, and mechanisms of effective treatment, for whom treatment is effective, and how those effects unfold over time. Answers to such intricate and relatively subtle research questions are sure to reside at the level of individual differences (as opposed to group differences) in response to treatment. Research designs and analytic methods capable of elucidating differences between individuals are bound to be pivotal components in an expanded research agenda for the field.
As a step toward an individually focused research agenda, this study provides support for the use of cluster analysis for studying profiles of individual change in response to adolescent substance abuse treatment. The differences in the profiles themselves, as well as factors related to cluster membership, appear to provide some guidance with respect to tailoring treatments to the needs of different subgroups of adolescents. Understanding profiles and predictors of change through cluster analysis and other advanced procedures can help advance the science of adolescent substance abuse treatment and facilitate efforts to transport such treatments into community treatment settings.
Figure 2.
Comparison of four clusters groupings for percent days substance use for substance use (excluding tobacco).
Acknowledgements
This research was supported in part by grants from the National Institute on Drug Abuse (RO1 DA09422) and National Institute on Alcohol Abuse and Alcoholism (RO1 AA12183). We also gratefully acknowledge the tireless efforts of our therapists and support staff. We especially would like to thank Janet L. Brody for providing clinical supervision to the therapy staff and Sheryl Kern-Jones and Meg Curtin for coordinating the data collection process.
Footnotes
Several procedures have been developed to address the problem of incomplete data in the assessment of change trajectories. We will apply an approach called multiple imputation for the present data but these other approaches sometime may be more appropriate. One statistical approach is called pattern mixture modeling (Hedekker & Gibbons, 1997). In this approach, the sample is divided into subgroups that appear to have similar patterns of missing values. Separate analyses are conducted within each pattern of missing data to determine whether findings are consistent across the various patterns of missing data. The pattern mixture modeling procedure can be especially effective when sample sizes are relatively large (n > 50) and the number of patterns of missing data are rather small (say, 5 or less). Under these circumstances, the sample size for each pattern can be large enough to create separate estimates for each pattern. These requirements are usually not met for clinical trials involving family therapy and we will not apply this procedure to the current data.
The objective of the missing data analysis is to determine whether or not data are missing at random, a critical issue because methods of handling missing data are contingent on whether data are randomly or systematically missing. An important assumption of the MI estimation procedure is that the data are missing at random. However, data may not be missing at random in typical clinical trials since the attrition from treatment may be due to clinically relevant rather than random factors. Procedures other than the MI approach are available for addressing missing data when data are not missing at random. A third statistical approach (i.e., other than HLM or MI) is pattern mixture modeling (Hedekker & Gibbons, 1997). In this approach, the sample is divided into subgroups that appear to have similar patterns of missing values. If the missing data patterns are consistent with the pattern-mixture model approach, we will use this approach to examine the data. The objective of the missing data analysis is to determine whether or not data are missing at random, a critical issue because methods of handling missing data are contingent on whether data are randomly or systematically missing.
We will use propensity scores to statistically control for differential attrition biases as well as other systematic missing data mechanisms in the proposed study (Little & Rubin, 1989; Rosenbaum & Rubin, 1985). Propensity scores will be used to estimate the likelihood of completing or dropping out of a study based on sets of variables that may predict the participant’s attrition status, including treatment group membership. Specifically, the predictor variables will be incorporated in a logistic regression analysis with attrition status as the dependent variable. The logistic regression will yield a probability estimate of an individual dropping out of the study as a linear function of the predictor variables in the equation. These probability estimates, or propensity scores, will then be used as covariates in subsequent statistical tests to control for differential attrition biases.
A simple example may help to understand the Euclidean distance. Suppose that you have placed a number of objects in a box with the sides represented by x, y and z. The Euclidean distance between any two pairs of objects in the box is the value that would be obtained by using a ruler to directly measure the distance between the objects. We can also create this “ruler” distance by using the values measured along the x, y, and z axes. To estimate the ruler distance, we square the values obtained reflecting differences between a pair of individuals on each axis and then we add the squared distances for this pair. Next, we calculate the square root of this sum. The resulting value should be the same as the distance obtained if we directly measured the distance between the objects. The notion of Euclidean distance becomes more abstract when we have more than three dimensions, but the fundamental meaning is the same as for two or three dimensions.
References
- Achenbach TM, Edelbrock CS. Manual for the Child Behavior Checklist and Child Behavior Profile. Child Psychiatry, University of Vermont; Burlington, VT: 1982. [Google Scholar]
- Aharonovich E, Liu X, Nunes E, Hasin DS. Suicide attempts in substance abusers: effects of major depression in relation to substance use disorders. American Journal of Psychiatry. 2002;159:1600–1602. doi: 10.1176/appi.ajp.159.9.1600. [DOI] [PubMed] [Google Scholar]
- Aldenderfer MS, Blashfield RK. Cluster analysis. Sage Publications; Thousand Oaks, CA: 1984. [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Beck AT, Ward C, Mendelson M, Mock J, Erlbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:53–63. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Broome KM, Joe GW, Simpson DD. Engagement models for adolescents in DATOS-A. Journal of Adolescent Research. 2001;16(6):608–623. [Google Scholar]
- Brown SA, D’Amico EJ, McCarthy DM, Tapert SF. Four-year outcomes from adolescent alcohol and drug treatment. Journal of Studies on Alcohol. 2001:381–388. doi: 10.15288/jsa.2001.62.381. [DOI] [PubMed] [Google Scholar]
- Brown SA, Myers MG, Mott MA, Vik PW. Correlates of success following treatment for adolescent substance abuse. Applied Preventative Psychology. 1994;3:61–73. [Google Scholar]
- Brown SA, Vik PW, Creamer VA. Characteristics of relapse following adolescent substance abuse treatment. Addictive Behaviors. 1989;14:291–300. doi: 10.1016/0306-4603(89)90060-9. [DOI] [PubMed] [Google Scholar]
- Catalano RF, Hawkins JD, Wells EA, Miller J, Brewer DD. Evaluation of the effectiveness of adolescent drug abuse treatment, assessment of risks for relapse, and promising approaches for relapse prevention. International Journal of the Addictions. 19901991;25(9A and 10B):1085–1140. doi: 10.3109/10826089109081039. [DOI] [PubMed] [Google Scholar]
- Coatsworth JD, Santisteban DA, McBride CK, Saapocznik J. Brief strategic family therapy versus community control: Engagement, retention, and an exploration of the moderating role of adolescent symptom severity. Family Process. 2001;40(3):313–332. doi: 10.1111/j.1545-5300.2001.4030100313.x. [DOI] [PubMed] [Google Scholar]
- Cornelius JR, Maisto SA, Pollock NK, Martin CS, Salloum IM, Lynch KG, Clark DB. Rapid relapse generally follows treatment for substance use disorders among adolescents. Addictive Behaviors. 2003;28:381–386. doi: 10.1016/s0306-4603(01)00247-7. [DOI] [PubMed] [Google Scholar]
- Crowley TJ, Mikulich SK, MacDonald M, Young SE, Zerbe GO. Substance-dependent, conduct-disordered adolescent males: Severity of diagnosis predicts 2-year outcome. Drug and Alcohol Dependence. 1998;49:225–237. doi: 10.1016/s0376-8716(98)00016-7. [DOI] [PubMed] [Google Scholar]
- Dausey DJ, Desai RA. Psychiatric comorbidity and the prevalence of HIV infection in a sample of patients in treatment for substance abuse. Journal of Nervous and Mental Disease. 2003;191:10–17. doi: 10.1097/00005053-200301000-00003. [DOI] [PubMed] [Google Scholar]
- Deas D, Thomas SE. An overview of controlled studies of adolescent substance abuse treatment. The American Journal on Addictions. 2001;10:178–189. doi: 10.1080/105504901750227822. [DOI] [PubMed] [Google Scholar]
- Deas D, Riggs P, Langenbucher J, Goldman M, Brown S. Adolescents are not adults: Developmental considerations in alcohol users. Alcoholism: Clinical and Experimental Research. 2000;24(2):232–237. [PubMed] [Google Scholar]
- Dennis ML, Dawud-Noursi S, Muck RD, McDermeit (Ives) M. The need for developing and evaluating adolescent treatment models. In: Stevens SJ, Morral AR, editors. Adolescent drug treatment in the United States: Exemplary models from a National Evaluation Study. Haworth Press; Binghamton, NY: 2002. pp. 3–34. [Google Scholar]
- Dennis ML, Godley SH, Tims FM, Babor T, Donaldson J, Liddle H, et al. The Cannabis Youth Treatment (CYT) Study: Main findings from two randomized trials. Journal of Substance Abuse Treatment. 2004;27:197–213. doi: 10.1016/j.jsat.2003.09.005. [DOI] [PubMed] [Google Scholar]
- Dobkin PL, Chabot L, Miliantovitch K, Craig W. Predictors of outcome in drug treatment of adolescent inpatients. Psychological Reports. 1998;83:175–186. doi: 10.2466/pr0.1998.83.1.175. [DOI] [PubMed] [Google Scholar]
- Duncan TE, Duncan SC, Hops H. Latent variable modeling of longitudinal and multilevel alcohol use data. Journal of Studies on Alcohol. 1998;59:399–408. doi: 10.15288/jsa.1998.59.399. [DOI] [PubMed] [Google Scholar]
- Eddy JM, Chamberlain P. Family management and deviant peer association as mediators of the impact of treatment condition on youth antisocial behavior. Journal of Consulting and Clinical Psychology. 2000;68:857–863. doi: 10.1037/0022-006X.68.5.857. [DOI] [PubMed] [Google Scholar]
- Elliott DS, Huizinga D. Social Class and delinquent behavior in a national youth panel. Criminology: An interdisciplinary journal. 1983;21(2):149–177. [Google Scholar]
- Everitt B. Cluster analysis. 4th Ed. Oxford University Press; New York: 2001. [Google Scholar]
- Finney JW, Moos RH, Chan DA. Length of stay and program component effects in the treatment of alcoholism: A comparison of two techniques for process analyses. Journal of Consulting & Clinical Psychology. 1981;49:120–131. doi: 10.1037//0022-006x.49.1.120. [DOI] [PubMed] [Google Scholar]
- Friedman AS, Glickman NW, Morrissey MR. What mothers know about their adolescents’ alcohol/drug use and problems, and how mothers react to finding out about it. In: Friedman AS, Granick, editors. Family Therapy for Adolescent Drug Abuse. Lexington Books; New York: 1990. pp. 169–181. [Google Scholar]
- Godley SH, Godley MD, Dennis ML. The Assertive Aftercare Protocol for adolescent substance abusers. In: Wagner EF, Waldron HB, editors. Innovations in Adolescent Substance Abuse Interventions. Pergamon; New York: 2001. pp. 313–331. [Google Scholar]
- Gorman-Smith D, Tolan PH, Loeber R, Henry DB. Relation of family problems to patterns of delinquent involvement among urban youth. Journal of Abnormal Child Psychology. 1998;26:319–333. doi: 10.1023/a:1021995621302. [DOI] [PubMed] [Google Scholar]
- Hanish LD, Tolan PH. Patterns of change in family-based aggression prevention. Journal of Marital and Family Therapy. 2001;27:213–226. doi: 10.1111/j.1752-0606.2001.tb01158.x. [DOI] [PubMed] [Google Scholar]
- Hops H, Davis B, Lewin L. The development of alcohol and other substance use: A gender study of family and peer context. Journal of Studies on Alcohol. 1999;(Supplement No13):22–31. doi: 10.15288/jsas.1999.s13.22. [DOI] [PubMed] [Google Scholar]
- Huey SJ, Henggeler SW, Brondino MJ, Pickrel SG. Mechanisms of change in multisystemic therapy: Reducing delinquent behavior through therapist adherence and improved family and peer functioning. Journal of Consulting and Clinical Psychology. 2000;68:451–467. [PubMed] [Google Scholar]
- Jacob T, Seilhamer RA. Alcoholism and family interaction. In: Jacob T, editor. Family Interaction and Psychopatholgy: Theories, Methods, and Findings. Plenum Press; New York: 1987. pp. 535–580. [Google Scholar]
- Jacob T, Tennenbaum DL. Family assessment: Rationale, methods, and future directions. Plenum Press; New York: 1988. [Google Scholar]
- Jessor R, Jessor SL. Problem behavior and psychosocial development: A longitudinal study of youth. Academic Press; New York: 1977. [Google Scholar]
- Kaminer Y, Burleson JA. Psychotherapies for adolescent substance abusers: 15-month follow-up of a pilot study. American Journal on Addictions. 1999;8(2):114–119. doi: 10.1080/105504999305910. [DOI] [PubMed] [Google Scholar]
- Kaminer MD, Burleson JA, Blitz C, Sussman J, Rounsaville BJ. Psychotherapy for adolescent substance abusers. A pilot study. The Journal of Nervous and Mental Disease. 1998;186(11):684–690. doi: 10.1097/00005053-199811000-00004. [DOI] [PubMed] [Google Scholar]
- King CA, Ghaziuddin N, McGovern L, Brand E, Hill E, Naylor M. Predictors of comorbid alcohol and substance abuse in depressed adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:743–751. doi: 10.1097/00004583-199606000-00014. [DOI] [PubMed] [Google Scholar]
- Latimer WW, Newcomb M, Winters KC, Stinchfield RD. Adolescent Substance Abuse Treatment Outcome: The Role of Substance Abuse Problem Severity, Psychosocial, and Treatment Factors. Journal of Consulting and Clinical Psychology. 2000a;68(4):684–696. [PubMed] [Google Scholar]
- Latimer WM, Winters KC, Stinchfield R, Traver RE. Demographic, individual, and interpersonal predictors of adolescent alcohol and marijuana use following treatment. Psychology of Addictive Behaviors. 2000b;14:162–173. doi: 10.1037//0893-164x.14.2.162. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR. Adolescent psychopathology: III. The clinical consequences of comorbidity. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:510–519. doi: 10.1097/00004583-199504000-00018. [DOI] [PubMed] [Google Scholar]
- Liddle HA, Dakof GA, Parker K, Diamond GS, Barrett K, Tejeda M. Multidimensional Family Therapy for adolescent drug abuse: Results of a randomized clinical trial. American Journal of Drug and Alcohol Abuse. 2001;27:651–688. doi: 10.1081/ada-100107661. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Pollock NK, Lynch KG, Martin CS, Ammerman R. Course of functioning in adolescents 1 year after alcohol and other drug treatment. Psychology of Addictive Behaviors. 2001;15(1):68–76. doi: 10.1037/0893-164x.15.1.68. [DOI] [PubMed] [Google Scholar]
- McArdle JJ, Hamagami F. Multilevel models from a multiple group structural equation perspective. In: Marcoulides G, Schumacker R, editors. Advanced Structural Equation Modeling Techniques. Erlbaum; Hillsdale, N.J.: 1996. pp. 89–124. [Google Scholar]
- McKay JR, Buka SL. Issues in the treatment of antisocial adolescent sbustance abusers. Journal of Child and Adolescent Substance Abuse. 1994;3:59–79. [Google Scholar]
- McKay JR, Merikle E, Mulvaney FD, Weiss RV, Kppenhaver JM. Factors accounting for cocaine use two years following initiation of continuing care. Addiction. 2001;96:213–225. doi: 10.1046/j.1360-0443.2001.9622134.x. [DOI] [PubMed] [Google Scholar]
- Miller NS, Ninonuevo FG, Klamen DL, Hoffmann NG, Smith DE. Integration of treatment and posttreatment variables in predicting results of abstinence-based outpatient treatment after one year. Journal of Psychoactive Drugs. 1997;29(3):239–248. doi: 10.1080/02791072.1997.10400197. [DOI] [PubMed] [Google Scholar]
- Morral AR, Iguchi MY, Belding MA, Lamb RJ. Natural classes of treatment response. Journal of Consulting and Clinical Psychology. 1997;65:673–685. doi: 10.1037//0022-006x.65.4.673. [DOI] [PubMed] [Google Scholar]
- Muthen B. Second generation structural equation modeling with a combination of categorical and continuous latent variables: New opportunities for latent class/latent growth modeling. In: Sayer A, Collins L, editors. New methods for the analysis of change. American Psychological Association; Washington, D. C.: 2001. [Google Scholar]
- Muthen B, Curran P. General longitundinal modeling of individual differences in experimental designs: A latent variable framework for analysis and power estimation. Psychological Methods. 1997;2:371–402. [Google Scholar]
- Myers MG. (2001). Cigarette smoking treatment for substance abusing adolescents. In: Wagner EF, Waldron HB, editors. Innovations in the treatment of adolescent substance abuse. Elsevier Science; 2001. [Google Scholar]
- Myers MG, Brown SA. Coping responses and relapse among adolescent substance abusers. Journal of Substance Abuse. 1990;2:177–189. doi: 10.1016/s0899-3289(05)80054-9. [DOI] [PubMed] [Google Scholar]
- Myers MG, Brown SA. Smoking and health in substance abusing adolescents: A two year follow-up. Pediatrics. 1994;93:561–566. [PubMed] [Google Scholar]
- Myers M, Brown S, Mott Coping as a predictor of adolescent substance abuse treatment outcome. Journal of Substance Abuse. 1993;5:15–29. doi: 10.1016/0899-3289(93)90120-z. [DOI] [PubMed] [Google Scholar]
- Needle R, McCubbin H, Lorence J, Hochhauser M. Reliability and validity of adolescent self-reported drug use in a family-based study: A methodological report. International Journal of Addiction. 1983;18:901–912. doi: 10.3109/10826088309033058. [DOI] [PubMed] [Google Scholar]
- Orwin RG, Ellis B, Williams V, Maranda M. Relationships between treatment components, client-level factors, and positive treatment outcomes. Journal of Psychopathology and Behavioral Assessment. 2000;22(4):383–397. [Google Scholar]
- Ozechowski TJ, Liddle HA. Family-based therapy for adolescent drug abuse: Knowns and unknowns. Clinical Child and Family Psychology Review. 2000 doi: 10.1023/a:1026429205294. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2nd ed. Sage; Newbury Park, CA: 2002. [Google Scholar]
- Riggs PD, Baker S, Mikulich SK, Young SE, Crowley TJ. Depression in substance-dependent delinquents. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:764–771. doi: 10.1097/00004583-199506000-00017. [DOI] [PubMed] [Google Scholar]
- Roberts RE, Lewinsohn PM, Seeley JR. Screening for adolescent depression: A comparison of depression scales. Journal of the American Academy of Child and Adolescent Psychiatry. 1991;30:58–66. doi: 10.1097/00004583-199101000-00009. [DOI] [PubMed] [Google Scholar]
- Robbins MS, Alexander JF, Newell RM, Turner CW. The immediate effect of reframing on client attitude on family therapy. Journal of Family Psychology. 1996;10:28–34. [Google Scholar]
- Robbins MS, Alexander JF, Turner CW. Disrupting defensive family interactions in family therapy with delinquent adolescents. Journal of Family Psychology. 2000;14:688–701. doi: 10.1037//0893-3200.14.4.688. [DOI] [PubMed] [Google Scholar]
- Rohde P, Clarke GN, Mace DE, Jorgensen JS, Seeley JR. An efficacy/effectiveness study of cognitive-behavioral treatment for adolescents with comorbid major depression and conduct disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:660–668. doi: 10.1097/01.chi.0000121067.29744.41. [DOI] [PubMed] [Google Scholar]
- Rohde P, Clarke GN, Lewinsohn PM, Seeley JR, Kaufman NK. Impact of comorbidity on a cognitive-behavioral group treatment for adolescent depression. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:795–802. doi: 10.1097/00004583-200107000-00014. [DOI] [PubMed] [Google Scholar]
- Schafer JL. Analysis of incomplete multivariate data. Chapman and Hall; New York: 1997. [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the start of the art. Psychological Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Shafii M, Steltz-Lenarsky J, Derrick AM, Beckner C. Comorbidity of mental disorders in the post-mortem diagnosis of completed suicide in children and adolescents. Journal of Affective Disorders. 1988;15:227–233. doi: 10.1016/0165-0327(88)90020-1. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow-back. In: Litten R, Allen J, editors. Measuring alcohol consumption. Humana Press; Totowa, NJ: 1992. pp. 41–72. [Google Scholar]
- Sobell LC, Sobell MB. Alcohol consumption measures. In: Allen JP, Columbus M, editors. Assessing alcohol problems: A guide for clinicians and researchers. National Institutes of Health; Rockville, MD: 1995. pp. 55–74. National Institute on Alcohol Abuse and Alcoholism. [Google Scholar]
- Spear SF, Ciesla JR, Skala SY. Relapse patterns among adolescents treated for chemical dependency. Substance Use and Misuse. 1999;34:1795–1815. doi: 10.3109/10826089909039427. [DOI] [PubMed] [Google Scholar]
- Stanton MD, Shadish WR. Outcome, attrition, and family/couples treatment for drug abuse: A review of the controlled, comparative studies. Psychological Bulletin. 1997;122:170–191. doi: 10.1037/0033-2909.122.2.170. [DOI] [PubMed] [Google Scholar]
- Szapocznik J, Kurtines W. Breakthroughs in family therapy with drug abusing problem youth. Springer; New York: 1989. [Google Scholar]
- USDHHS . Preventing tobacco use among young people: A report of the Surgseon General. United States Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Atlanta, GA: 1994. [Google Scholar]
- Wagner EF, Brown S, Myers M, Monti PM, Waldron HB. Innovations in adolescent substance abuse intervention. Alcoholism. 1999;23:236–249. [PubMed] [Google Scholar]
- Wagner EF, Waldron HB, editors. Innovations in the treatment of adolescent substance abuse. Elsevier Science; 2001. [Google Scholar]
- Waldron HB. Adolescent substance abuse and family therapy outcome: A review of randomized trials. In: Ollendick TH, Prinz RJ, editors. Advances in clinical child psychology. Vol. 19. Plenum; New York: 1997. pp. 199–234. [Google Scholar]
- Waldron HB. Adolescent substance abuse disorders. In: Bellack A, Hersen M, editors. Comprehensive clinical psychology (Vol. 5: Children and adolescents: Clinical formulation and treatment) Elsevier Science; 1998. pp. 539–563. [Google Scholar]
- Waldron HB, Kaminer Y. On the learning curve: Cognitive-behavioral therapies for adolescent substance abuse. Addiction. 2004;99:93–105. doi: 10.1111/j.1360-0443.2004.00857.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldron HB, Turner CW, Barton C, Alexander JF, Cline VB. The contribution of therapist defensiveness to marital therapy process and outcome: A path analytic approach. The American Journal of Family Therapy. 1997;25:40–50. [Google Scholar]
- Waldron HB, Turner CW, Ozechowski T. Trajectories of change in behavioral and family interventions for adolescent substance abuse and dependence. In: Rowe C, Liddle H, editors. Treating adolescent substance abuse: State of the science. Cambridge University Press; New York: (In press). [Google Scholar]
- Willett JB, Sayer AG. Using covariance structure analysis to detect correlates and predictors of individual change over time. Psychological Bulletin. 1994;116(2):363–381. [Google Scholar]
- Williams RJ, Chang SY, Addiction Centre Adolescent Research Group A comprehensive and comparative review of adolescent substance abuse treatment outcome. Clinical Psychology: Science and Practice. 2000;7:138–166. [Google Scholar]
- Wills AW, McNamara G, Vaccaro D, Hirkey AE. Escalated substance use: A longitudinal grouping analysis from early to middle adolescence. Journal of Abnormal Psychology. 1996;105:166–180. doi: 10.1037//0021-843x.105.2.166. [DOI] [PubMed] [Google Scholar]
- Winters KC. Treating adolescents with substance use disorders: An overview of practice issues and treatment outcome. Substance Abuse. 1999;20:203–225. doi: 10.1080/08897079909511407. [DOI] [PubMed] [Google Scholar]
- Wu LT, Ringwalt CL, Williams CE. Use of substance abuse treatment services by persons with mental health and substance use problems. Psychiatric Services. 2003;54:363–369. doi: 10.1176/appi.ps.54.3.363. [DOI] [PubMed] [Google Scholar]