Abstract
OBJECTIVE
Few studies have quantified the prevalence of weight-related orthopedic conditions in otherwise healthy overweight children. The goal of the present investigation was to describe the musculoskeletal consequences of pediatric overweight in a large pediatric cohort of children that included severely overweight children.
METHODS
Medical charts from 227 overweight and 128 nonoverweight children and adolescents who were enrolled in pediatric clinical studies at the National Institutes of Health from 1996 to 2004 were reviewed to record pertinent orthopedic medical history and musculoskeletal complaints. Questionnaire data from 183 enrollees (146 overweight) documented difficulties with mobility. In 250, lower extremity alignment was determined by bilateral metaphyseal-diaphyseal and anatomic tibiofemoral angle measurements made from whole-body dual-energy x-ray absorptiometry scans.
RESULTS
Compared with nonoverweight children, overweight children reported a greater prevalence of fractures and musculoskeletal discomfort. The most common self-reported joint complaint among those who were questioned directly was knee pain (21.4% overweight vs 16.7% nonoverweight). Overweight children reported greater impairment in mobility than did nonoverweight children (mobility score: 17.0 ± 6.8 vs 11.6 ± 2.8). Both metaphyseal-diaphyseal and anatomic tibiofemoral angle measurements showed greater malalignment in overweight compared with nonoverweight children.
CONCLUSIONS
Reported fractures, musculoskeletal discomfort, impaired mobility, and lower extremity malalignment are more prevalent in overweight than nonoverweight children and adolescents. Because they affect the likelihood that children will engage in physical activity, orthopedic difficulties may be part of the cycle that perpetuates the accumulation of excess weight in children.
Keywords: obesity, fractures, valgus deformity, child, quality of life
According to the Centers for Disease Control and Prevention 1999–2002 statistics, almost 16% of children and adolescents have a BMI (kg/m2) ≥95th percentile for age and gender and are classified as overweight.1 The prevalence of overweight has more than tripled in the past 3 decades;2 concomitantly, the prevalence has increased for many obesity-related comorbid conditions.3
Orthopedic complications of excess weight in adults include progression of degenerative osteoarthritis and articular cartilage breakdown,4,5 a decline in physical functioning,6 and poorer outcomes after orthopedic surgery for obesity-related disorders.7,8 Some orthopedic disorders that are unique to childhood also have been suggested to be weight related. For example, retrospective analyses of children and adolescents with slipped capital femoral epiphysis and adolescent tibia vara (Blount’s disease) reveal overrepresentation of overweight individuals.9–11 However, few prospective data that quantify the prevalence and manifestations of potentially weight-related orthopedic conditions in overweight children and adolescents who are not referred for orthopedic concerns are available. Furthermore, the impact of such conditions on mobility in overweight children has not previously been examined.
The goal of the present investigation was to describe the musculoskeletal consequences of pediatric overweight in a large cohort of children who ranged in BMI from normal to severely overweight. We hypothesized that, compared with nonoverweight children and adolescents, those who were overweight would experience a significantly greater prevalence of orthopedic complications, including musculoskeletal pain, fractures, slipped capital femoral epiphysis, tibia vara, and both valgus and varus lower extremity misalignment. We also hypothesized that the orthopedic comorbidities that are found in children and adolescents with significant overweight would hinder their mobility and tolerance for physical activity.
METHODS
Subjects
We studied 355 black and white children and adolescents (198 girls and 157 boys) who were recruited between 1996 and 2004 either for weight-reduction trials (n = 135) or nonintervention studies of metabolism and body composition (n = 220) at the National Institutes of Health. Youth were recruited through notices that were mailed to school children in the Washington, DC, metropolitan area requesting healthy volunteers; by advertisements in local newspapers; and, in the case of overweight children who were seeking weight-reduction treatment, by referral from local physicians. There was no mention of musculoskeletal disorders in any advertisement. The study was approved by the Intramural National Institute of Child Health and Human Development Institutional Review Board. Each child gave written assent and a parent gave written consent for protocol participation.
Protocol
History and Physical Examination
Before initiating any study protocol, each youth underwent a structured medical history and physical examination that included historical review of joint-, bone-, and muscle-related complaints; height; weight; Tanner staging for pubertal development; and a physical examination that included a brief musculoskeletal examination. Youth were considered overweight when their BMI exceeded the 95th percentile (as determined by National Health and Nutrition Examination Survey I age-, gender-, and race-specific data).12 Youth were considered nonoverweight when their BMI was between the 5th and 95th percentiles. A subset of adolescents (n = 154) also completed an extensive musculoskeletal review of systems that originally was designed as part of an adverse drug reaction detection questionnaire,13 which was administered by 2 of the authors (K.A.C. and E.D.T.).
Quality-of-Life Questionnaire
A subset of adolescents (n = 183) completed the Impact of Weight on Quality-of-Life, adapted for use with adolescents (IWQOL-A) questionnaire.14 The IWQOL-A is a 66-item, self-report, condition-specific instrument that was designed to measure the perceived effect of weight on quality of life. The original IWQOL has demonstrated good construct validity, test–retest reliability, and internal consistency.15 The “mobility” domain of the IWQOL-A includes 10 specific questions regarding physical limitations related to movement. Examples of questions that are scored under the mobility domain include, “I have trouble with mobility,” “I have trouble using stairs,” “I feel clumsy or awkward,” and, “I have difficulty getting up from chairs,” with the 5 possible responses ranging from, “Always,” to, “Never true.” A higher IWQOL-A mobility subscale score indicates a greater level of impairment.
Dual-Energy X-Ray Absorptiometry
Body composition was assessed by whole-body dual energy x-ray absorptiometry (DXA) using the Hologic (Bedford, MA) QDR 2000 pencil beam or 4500A fan-beam densitometer in 250 youth. Each youth was supine with his or her feet stabilized in an inverted position. Images were analyzed using eFilm Lite DICOM image viewer software (Milwaukee, WI). Using the skeletal images produced by the DXA scanner, we evaluated axial alignment of the lower extremity by measuring the anatomic tibiofemoral angle (A-TFA) and metaphyseal-diaphyseal angle (MDA) of each youth’s lower extremity to the nearest degree (Fig 1). The A-TFA is created by lines that are drawn along the longitudinal axes of the tibia and the femur. The MDA is produced by a line that is drawn perpendicular to the longitudinal axis of the tibia and a second line that is drawn through 2 beaks of the tibial metaphysis. Given the predetermined axis of reference, positive values of the MDA and A-TFA represent degrees of varus alignment. Conversely, negative values indicate degrees of valgus alignment. Using results from previous studies of standing radiographs,16–21 the following cut points were used for the limits of normal alignment: MDA between +11 and −11 degrees and A-TFA between +5 and −15 degrees.
FIGURE 1.
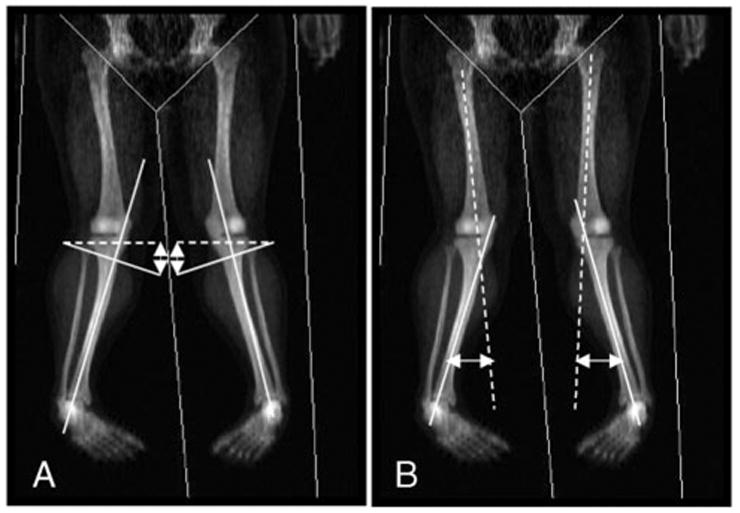
Measurement of lower extremity alignment. Whole-body DXA scans were used to measure lower extremity alignment. The MDA was defined as the angle between a line through the metaphyseal beaks (dashed line) and a line perpendicular to the tibial shaft (A). The A-TFA was defined as the angle formed by lines through the tibial and femoral shafts (B). In these sample images, the lower extremities demonstrate a bilateral valgus alignment of 20 degrees in the left leg and 20 degrees in the right leg, according to MDA measurements.
Statistical Analysis
Contingency table analyses, multiple regression, and mixed model analyses of covariance were performed using StatView version 5.01 (SAS Institute, Inc Cary, NC). Results are presented as mean ± SD unless otherwise specified, with statistical significance set at P ≤ .05. There were 3 primary research outcomes for this investigation: (1) the prevalence of specific orthopedic conditions (slipped capital femoral epiphysis, tibia vara, gait abnormalities, and joint pain) as determined by history obtained from overweight and normal-weight adolescents and their parents; (2) the relationship between body weight and self-reported difficulties with mobility, as measured by the mobility scale of the IWQOL-A; and (3) the relationship between body weight and lower extremity alignment in adolescents as determined by DXA scan.
Intra- and interobserver variabilities for assessments of lower extremity alignment on DXA scan images were determined through calculation of coefficients of variation for each of the angles from repeated measurements that were obtained from 19 randomly selected youth. The coefficient of variation measures variability relative to the magnitude of the data and is defined as the ratio of sample SD to sample mean.
RESULTS
Participant Characteristics
A total of 355 youth, 227 overweight and 128 nonoverweight, were studied (Table 1). Compared with nonoverweight participants, overweight youth were slightly but significantly older (11.8 ± 2.9 vs 12.6 ± 2.7 years; P < .001), more likely to be female (P < .01), and more likely to be self-identified as black (P < .001). Age, gender, and race therefore were included as covariates in subsequent analyses.
TABLE 1.
Participant Demographics
| Nonoverweight (BMI <95th Percentile; N =128) | Overweight (BMI ≥ 95th Percentile; N =227) | |
|---|---|---|
| Gender, % | ||
| Male | 54 | 39 |
| Female | 46 | 61 |
| Age, y | 11.8 ± 2.9 | 12.6 ± 2.7 |
| Race, % | ||
| Black | 27.3 | 52.9 |
| White | 67.4 | 46.3 |
| Other | 5.3 | 0.8 |
| BMI, kg/m2 (range) | 19.6 ± 3.5 (12.9–28.3) | 36.4 ± 8.9 (19.0–69.0) |
| BMI-SD score for age and gender (range) | 0.42 ± 0.85 (−2.29 to 1.63) | 2.45 ± 0.36 (1.64–3.41) |
Data are mean ± SD unless otherwise indicated. Compared with nonoverweight participants, overweight participants were significantly older (P <.001), more likely to be female (P <.01), and more likely to be self-identified as black (P <.001).
Medical Chart Review
The medical charts of all 355 participants were reviewed. The prevalence of documented skeletal fractures was significantly greater in overweight than in nonoverweight children and adolescents (odds ratio [OR]: 4.54; 95% confidence interval [CI]: 1.6–13.2; P = .0053; Fig 2A). The prevalence of any recorded musculoskeletal pain, including back, hip, leg, knee, ankle, or foot pain, also was significantly greater in overweight than in nonoverweight participants (OR: 4.04; 95% CI: 1.5–10.6; P = .0073). The most common documented musculoskeletal joint complaint, knee pain, was noted in the medical charts of 6.6% of overweight and 2.3% of nonoverweight youth (OR: 2.95; 95% CI: 0.8–10.4; P = .079). Eighty percent of the musculoskeletal complaints reported were described by the 242 adolescents, aged 12 to 18 years, who were taking part (overweight versus nonoverweight: 14.4 ± 1.5 vs 14.4 ± 1.5 years; P = .50); when these adolescents were evaluated separately, the prevalence of musculoskeletal complaints was significantly greater for the overweight group (18.3% vs 4.8%; OR: 4.41; 95% CI: 1.3–15.0; P = .0096).
FIGURE 2.

Prevalence of fractures and musculoskeletal pain. The prevalence of chart-review documented fractures and complaints of musculoskeletal (MSK) pain at any anatomic location was significantly greater in overweight than in nonoverweight youth. aP < .01 (A). The prevalence of self-reported MSK complaints by a structured symptom questionnaire (B) also tended to be greater in the overweight group. Fracture history and history of leg pain were not assessed in the symptom questionnaire. Upper 95% CIs are shown.
There were 3 (1.3%) documented cases of slipped capital femoral epiphysis and 3 (1.3%) documented cases of Blount’s disease among overweight black male adolescents; the prevalence of these disorders was similar to that of past reports.9–11 Although none of the nonoverweight participants had a history of either condition, there were no significant differences in the chart-documented prevalence of any joint abnormality.
Musculoskeletal Review of Systems
Starting in 1999, a structured musculoskeletal review of systems was conducted with 154 overweight adolescents (mean age: 14.39 ± 1.48 years) and 31 age-matched nonoverweight adolescents (mean age: 14.64 ± 1.99 years) who were studied under 1 protocol. Consistent with the medical chart review findings, the most common site of musculoskeletal pain in the overweight group was the knee, with 21.4% endorsing knee pain as an active problem when asked directly. Although there were no significant differences in musculoskeletal disorder prevalence between overweight and nonoverweight adolescents who completed the structured review of systems, the prevalence of self-reported musculoskeletal complaints tended to be greater at all anatomic locations in overweight adolescents (Fig 2B).
Quality-of-Life Questionnaire
The IWQOL-A questionnaire was completed by 146 overweight and 37 nonoverweight participants (mean age: 14.4 ± 1.5 vs 14.1 ± 1.9 years; P = .35). Overweight youth reported poorer quality of life on the mobility subscale compared with their nonoverweight counterparts (16.9 ± 6.8 vs 11.6 ± 2.8; P < .001).
Lower Extremity Alignment by DXA
To validate the use of DXA scans for study of lower extremity alignment, we examined interobserver and intraobserver variability. Nineteen DXA images were randomly selected for blinded replicate measurements by 2 of the authors (E.D.T. and D.A.W.). Replicate measurements were significantly correlated both within and between observers (Table 2). Coefficients of variation for the 2 measures of lower extremity alignment also are given in Table 2. There was somewhat greater interobserver and intraobserver variability for the MDA measurements than for those of the A-TFA.
TABLE 2.
Validation of DXA Lower Extremity Alignment Measurements
| Measurement | Correlation Coefficient
|
Mean, degrees
|
SD
|
Coefficient of Variation, %
|
||||
|---|---|---|---|---|---|---|---|---|
| Interobserver | Intraobserver | Interobserver | Intraobserver | Interobserver | Intraobserver | Interobserver | Intraobserver | |
| Right MDA | 0.879a | 0.748a | −7.7 | −8.9 | 1.4 | 1.7 | 18.7 | 19.6 |
| Left MDA | 0.892a | 0.862a | −7.4 | −8.3 | 1.6 | 1.5 | 21.3 | 18.2 |
| Right A-TFA | 0.938a | 0.911a | −11.3 | −12.0 | 1.5 | 1.3 | 12.9 | 11.2 |
| Left A-TFA | 0.971a | 0.978a | −10.1 | −10.3 | 1.3 | 1.0 | 12.7 | 9.5 |
MDA and A-TFA from right and left lower extremities, measured in a blinded manner twice, either by the same investigator both times (intraobserver) or by two investigators (interobserver).
P <.01, N =19.
Lower extremity alignment was studied in 250 youth (91 nonoverweight and 159 overweight) whose scans were available for radiographic analysis. Scans were not available either because study participants exceeded the weight limit of the DXA machine (>136.4 kg; n = 58) or because their scans could not be retrieved from the computerized radiology archive (n = 47). Youth who were known to have documented Blount’s disease by medical history also were excluded. Among youth with assessable DXA scans, overweight youth were slightly but significantly older than nonoverweight participants (12.7 ± 2.6 vs 12.0 ± 2.7 years; P = .045). Bilateral measurement of the MDAs demonstrated significantly greater degrees of valgus alignment in overweight children, demonstrated both by a significant negative correlation between MDA and BMI z score (Fig 3A) and a significantly greater mean angle value in the overweight compared with the nonoverweight group (mean right MDA: −6.5 ± 4.6 vs −5.2 ± 3.9 degrees [P < .05]; left MDA: −7.2 ± 5.5 vs −4.8 ± 4.0 degrees [P < .05]). The correlation between A-TFA and BMI z score was not significant (Fig 3B), and mean A-TFAs were not significantly different between the overweight and nonoverweight groups (right A-TFA: −10.5 ± 5.5 vs −9.2 ± 6.0 degrees [P = NS]; left A-TFA: −9.1 ± 6.6 vs −9.2 ± 5.4 degrees [P = NS]). For both angle measurements, a significantly greater proportion of overweight children had angles classified as abnormal (Fig 3C); >11% of both MDA and A-TFA measurements were abnormal in overweight children, whereas <3.2% of each set of angle measurements were abnormal among children in the nonoverweight group.
FIGURE 3.

Lower extremity alignment measurements in overweight and nonoverweight children. Linear correlations between BMI SD score for age and gender (BMI z score) and MDA (A) and A-TFA (B) as determined using DXA. (C) A significantly greater proportion of overweight children (□) had abnormal MDA and A-TFA angles compared with nonoverweight children (■). aP <.01; bP <.05. Upper 95% CIs are shown.
DISCUSSION
This cross-sectional study investigated the association between overweight and orthopedic complications in children and adolescents. We found documented fractures and musculoskeletal pain to be more prevalent in the overweight pediatric sample compared with their nonoverweight counterparts by chart review, with similar trends found in a subset of adolescents who completed a structured musculoskeletal review of systems. Furthermore, overweight adolescents reported a greater impairment in mobility, and the results of DXA scan analyses suggested that the overweight group had a greater prevalence of abnormal lower extremity alignment.
Bone fractures are a frequent problem for children, and their incidence seems to be increasing in the United States.22 Although overweight in adults23,24 and children25–27 is associated with greater bone mineral density that might be expected to protect against fracture, the prevalence of fractures in children who are significantly overweight does not suggest a protective effect. Leonard et al27 proposed that the observed increase in bone mineral that is seen in overweight children is not sufficient to overcome the significantly greater forces that are generated when an overweight child falls on an out-stretched arm. A biomechanical analysis also has determined that overweight boys fall with much greater force than do nonoverweight boys and are at a relatively greater risk for fracture at low-fall heights. This finding is significant because exposure to falls at lower fall heights is most common among the most overweight, least active children, who do not tend to climb high on play equipment.28
Our finding that overweight children report a significant impairment in mobility compared with their nonoverweight counterparts may contribute further to their risk for fracture. Goulding et al29 reported that overweight male adolescents had poorer balance than healthy-weight adolescents and suggested that the poorer balance of boys with high adiposity may increase their risk for falling during daily activities, impede their ability to halt their forward progress once they begin to fall, and subsequently raise their risk for sustaining fractures.29 Therefore, because of their difficulties with mobility and balance, overweight children are at greater risk for falling from low heights, and because of the weight-related increase in force that is applied to their bones during such falls, they seem to be more likely to sustain a fracture.
Using DXA, we also detected a greater prevalence of lower extremity misalignment, mostly valgus deformity, in overweight children. Although we found statistically significant differences, it is unclear whether these findings are of clinical significance. However, we hypothesize that the combination of even a mild malalignment with excess weight loaded across the joints may be sufficient to contribute to the increased prevalence of musculoskeletal discomfort that is found in significantly overweight children. Children who are experiencing musculoskeletal pain and discomfort may be less likely to enjoy and therefore participate in many modes of physical activity, perpetuating the accumulation of excess weight over time.
This study has a number of strengths because of its prospective design. Whereas some published investigations have identified retrospectively obesity as a prevalent patient characteristic in conditions such as Blount’s disease,9,10 our study is one of the few cross-sectional analyses to explore a large population of overweight children who were not referred primarily for evaluation of orthopedic concerns.30 The use of multiple modalities to assess the musculoskeletal status of our youth provided confirmatory evidence for the greater musculoskeletal difficulties that overweight youth encounter. In addition, a novel technique using skeletal images that were derived from densitometry scans was used to examine lower extremity alignment in children without known skeletal or joint abnormalities. Interobserver and intraobserver correlations and variability coefficients were calculated to validate this procedure. The high correlation coefficients and general similarity between the inter- and intraobserver coefficients of variability illustrate that the systematic difference between observers was comparable to the intrinsic error of a single observer in reproducing these measures.
There also are limitations to this study. First, because youth did not routinely undergo standing radiographs, we could not determine conclusively how supine pediatric DXA alignment measures, although standardized among subjects, would correspond to those of a standing radiograph, the method typically used for such assessments. However, previous studies (in nonoverweight individuals) suggest that both lying and standing radiographs can be used to identify significant misalignments and differ by an average of only 2 degrees.31 It is unknown whether there are systematic biases in positioning that are caused by overweight; therefore, additional studies are needed to validate DXA for assessment of lower extremity alignment. DXA also has limitations in resolution that make it impossible to measure some of the standard angles that are used for assessment of alignment, including the mechanical axis. Second, our study did not implement a method to inquire about fracture history details, such as the precise mechanism of injury. Such data would have been useful in qualifying the correlation between fracture incidence and daily activities in overweight children. Similarly, additional inquiries into the severity of musculoskeletal pain and aggravating factors would have been useful in determining the relationship among joint pain, adiposity, and valgus lower extremity alignment. Third, although children with a wide range of BMIs were included, the group that was studied at the National Institutes of Health may not be fully representative of all overweight children in the United States. Fourth, because the heaviest children (>300 lb) could not be scanned by DXA, this study may underestimate the prevalence of lower limb deformity that is present among the heaviest children. Finally, the lack of significant findings from the musculoskeletal review of systems data may have been attributable to the small sample size of nonoverweight participants who completed this particular assessment.
CONCLUSION
Our results support the suggestion that fracture risk, musculoskeletal discomfort, and impairments in mobility may be health hazards of significant overweight in children and adolescents. Efforts should be made to encourage health care providers’ recognition of the orthopedic complications of excess weight so that interventions can be initiated. Future studies should investigate the biomechanical principles that underlie the increased prevalence of musculoskeletal pain in obesity. Finally, significantly overweight children and adolescents should be encouraged to engage in alternative modes of physical activity, such as bicycle riding or swimming, that potentially could alleviate the severity of lower extremity joint loading and discomfort.
Acknowledgments
This research was supported by the Intramural Research Program of the National Institutes of Health (NIH), grant ZO1-HD-00641 (National Institute of Child Health and Human Development, NIH) to J.A.Y. E.D.T. was supported by the NIH Clinical Research Training Program, a public–private partnership funded jointly by the NIH, and a grant to the Foundation for the NIH from Pfizer Pharmaceuticals Group. J.A.Y. is a Commissioned Officer in the US Public Health Service, Department of Health and Human Services.
We are appreciative of all participating children and their families. We also thank the nursing staff of the NIH and the technicians of the Department of Nuclear Medicine for invaluable assistance.
Abbreviations
- IWQOL-A
Impact of Weight on Quality-of-Life—adapted for use with adolescents
- DXA
dual-energy x-ray absorptiometry
- A-TFA
anatomic tibiofemoral angle
- MDA
metaphyseal-diaphyseal angle
- OR
odds ratio
- CI
confidence interval
Footnotes
The authors have indicated they have no financial relationships relevant to this article to disclose.
References
- 1.Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA. 2004;291:2847–2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999–2000. JAMA. 2002;288:1728–1732. doi: 10.1001/jama.288.14.1728. [DOI] [PubMed] [Google Scholar]
- 3.Must A, Strauss RS. Risks and consequences of childhood and adolescent obesity. Int J Obes Relat Metab Disord. 1999;23(suppl 2):S2–S11. doi: 10.1038/sj.ijo.0800852. [DOI] [PubMed] [Google Scholar]
- 4.Dougados M, Gueguen A, Nguyen M, et al. Longitudinal radiologic evaluation of osteoarthritis of the knee. J Rheumatol. 1992;19:378–384. [PubMed] [Google Scholar]
- 5.Cohen NP, Foster RJ, Mow VC. Composition and dynamics of articular cartilage: structure, function, and maintaining healthy state. J Orthop Sports Phys Ther. 1998;28:203–215. doi: 10.2519/jospt.1998.28.4.203. [DOI] [PubMed] [Google Scholar]
- 6.Xiaoxing Z, He DWB. Body Mass Index, physical activity, and the risk of decline in overall health and physical functioning in late middle age. Am J Public Health. 2004;94:1567–1573. doi: 10.2105/ajph.94.9.1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harrison MM, Morrell J, Hopman WM. Influence of obesity on outcome after knee arthroscopy. Arthroscopy. 2004;20:691–695. doi: 10.1016/j.arthro.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 8.Morris CD, Sepkowitz K, Fonshell C, et al. Prospective identification of risk factors for wound infection after lower extremity oncologic surgery. Ann Surg Oncol. 2003;10:778–782. doi: 10.1245/aso.2003.07.023. [DOI] [PubMed] [Google Scholar]
- 9.Henderson RC. Tibia vara: a complication of adolescent obesity. J Pediatr. 1992;121:482–486. doi: 10.1016/s0022-3476(05)81811-6. [DOI] [PubMed] [Google Scholar]
- 10.Dietz WH, Jr, Gross WL, Kirkpatrick JA., Jr Blount disease (tibia vara): another skeletal disorder associated with childhood obesity. J Pediatr. 1982;101:735–737. doi: 10.1016/s0022-3476(82)80305-3. [DOI] [PubMed] [Google Scholar]
- 11.Loder RT, Aronson DD, Greenfield ML. The epidemiology of bilateral slipped capital femoral epiphysis. A study of children in Michigan. J Bone Joint Surg Am. 1993;75:1141–1147. doi: 10.2106/00004623-199308000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Must A, Dallal GE, Dietz WH. Reference data for obesity: 85th and 95th percentiles of body mass index (wt/ht2) and triceps skinfold thickness. Am J Clin Nutr. 1991;53:839–846. doi: 10.1093/ajcn/53.4.839. [DOI] [PubMed] [Google Scholar]
- 13.Corso DM, Pucino F, DeLeo JM, Calis KA, Gallelli JF. Development of a questionnaire for detecting potential adverse drug reactions. Ann Pharmacother. 1992;26:890–896. doi: 10.1177/106002809202600704. [DOI] [PubMed] [Google Scholar]
- 14.Fallon EM, Tanofsky-Kraff M, Norman AC, et al. Health-related quality of life in overweight and nonoverweight black and white adolescents. J Pediatr. 2005;147:443–450. doi: 10.1016/j.jpeds.2005.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kolotkin RL, Head S, Brookhart A. Construct validity of the Impact of Weight on Quality of Life Questionnaire. Obes Res. 1997;5:434–441. doi: 10.1002/j.1550-8528.1997.tb00667.x. [DOI] [PubMed] [Google Scholar]
- 16.Arazi M, Ogun TC, Memik R. Normal development of the tibiofemoral angle in children: a clinical study of 590 normal subjects from 3 to 17 years of age. J Pediatr Orthop. 2001;21:264–267. [PubMed] [Google Scholar]
- 17.Feldman MD, Schoenecker PL. Use of the metaphyseal-diaphyseal angle in the evaluation of bowed legs. J Bone Joint Surg Am. 1993;75:1602–1609. doi: 10.2106/00004623-199311000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Iwasawa T, Inaba Y, Nishimura G, Aida N, Kameshita K, Matsubara S. MR findings of bowlegs in toddlers. Pediatr Radiol. 1999;29:826–834. doi: 10.1007/s002470050706. [DOI] [PubMed] [Google Scholar]
- 19.Levine AM, Drennan JC. Physiological bowing and tibia vara. The metaphyseal-diaphyseal angle in the measurement of bowleg deformities. J Bone Joint Surg Am. 1982;64:1158–1163. [PubMed] [Google Scholar]
- 20.Salenius P, Vankka E. The development of the tibiofemoral angle in children. J Bone Joint Surg Am. 1975;57:259–261. [PubMed] [Google Scholar]
- 21.Bowen RE, Dorey FJ, Moseley CF. Relative tibial and femoral varus as a predictor of progression of varus deformities of the lower limbs in young children. J Pediatr Orthop. 2002;22:105–111. [PubMed] [Google Scholar]
- 22.Khosla S, Melton LJ, 3rd, Dekutoski MB, Achenbach SJ, Oberg AL, Riggs BL. Incidence of childhood distal forearm fractures over 30 years: a population-based study. JAMA. 2003;290:1479–1485. doi: 10.1001/jama.290.11.1479. [DOI] [PubMed] [Google Scholar]
- 23.Finkelstein JS, Lee ML, Sowers M, et al. Ethnic variation in bone density in premenopausal and early perimenopausal women: effects of anthropometric and lifestyle factors. J Clin Endocrinol Metab. 2002;87:3057–2067. doi: 10.1210/jcem.87.7.8654. [DOI] [PubMed] [Google Scholar]
- 24.Stewart KJ, Deregis JR, Turner KL, et al. Fitness, fatness and activity as predictors of bone mineral density in older persons. J Intern Med. 2002;252:381–388. doi: 10.1046/j.1365-2796.2002.01050.x. [DOI] [PubMed] [Google Scholar]
- 25.Fischer S, Milinarsky A, Giadrosich V, Dib G, Arriagada M, Arinoviche R. X-ray absorptiometry of bone in obese and eutrophic children from Valparaiso, Chile. J Rheumatol. 2000;27:1294–1296. [PubMed] [Google Scholar]
- 26.De Schepper J, Van den Broek M, Jonckheer MH. Study of lumbar spine bone mineral density in obese children. Acta Paediatr. 1995;84:313–315. doi: 10.1111/j.1651-2227.1995.tb13635.x. [DOI] [PubMed] [Google Scholar]
- 27.Leonard MB, Shults J, Wilson BA, Tershakovec AM, Zemel BS. Obesity during childhood and adolescence augments bone mass and bone dimensions. Am J Clin Nutr. 2004;80:514–523. doi: 10.1093/ajcn/80.2.514. [DOI] [PubMed] [Google Scholar]
- 28.Davidson P, Goulding A, Chalmers D. Biomechanical analysis of arm fracture in obese boys. J Paediatr Child Health. 2003;39:657–664. doi: 10.1046/j.1440-1754.2003.00243.x. [DOI] [PubMed] [Google Scholar]
- 29.Goulding A, Jones IE, Taylor RW, Piggot JM, Taylor D. Dynamic and static tests of balance and postural sway in boys: effects of previous wrist bone fractures and high adiposity. Gait Posture. 2003;17:136–141. doi: 10.1016/s0966-6362(02)00161-3. [DOI] [PubMed] [Google Scholar]
- 30.Henderson RC, Kemp GJ, Hayes PR. Prevalence of late-onset tibia vara. J Pediatr Orthop. 1993;13:255–258. [PubMed] [Google Scholar]
- 31.Brouwer RW, Jakma TS, Bierma-Zeinstra SM, Ginai AZ, Verhaar JA. The whole leg radiograph: standing versus supine for determining axial alignment. Acta Orthop Scand. 2003;74:565–568. doi: 10.1080/00016470310017965. [DOI] [PubMed] [Google Scholar]


