The Case: A 66-year-old woman was admitted to hospital because of progressive dyspnea on exertion. At the time of admission, the patient became breathless on minimal activity. A high-grade atrioventricular block and associated congestive heart failure were diagnosed, and a biventricular internal cardiac defibrillator/pacemaker was inserted into her left pectoral region without complication. Her dyspnea rapidly resolved after insertion of the pacemaker and medical management of the heart failure; however, a routine postoperative chest radiograph revealed a mass in the right upper lobe (Fig. 1). No previous chest radiographs were available for comparison.
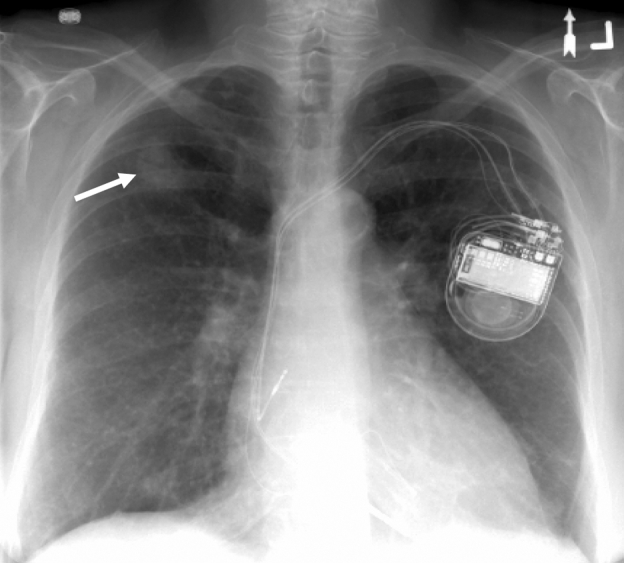
Fig. 1: Chest radiograph showing a mass in the right upper lobe (arrow).
The patient had a 50 pack-year history of smoking. She had received a diagnosis of hypothyroidism 3 months before admission, and she had a history of ischemic heart disease, with associated left ventricular dysfunction, and episodic supraventricular and nonsustained ventricular tachycardia. Her tachycardia had been treated with amiodarone (200 mg/d) for 4 years before admission (total cumulative dose about 300 g). She denied having any other respiratory or constitutional symptoms. The results of her physical examination were unremarkable. Blood count and routine serum biochemistry test results were normal except for a mildly elevated alanine transaminase level (67 [normal 1–40] U/L). A nonenhanced chest CT scan showed an irregular mass in the right upper lobe that measured 3.0 × 2.3 cm (Fig. 2). A smaller wedge-shaped lesion (1.8 × 1.2 cm) was also visible in the periphery of the right lower lobe. There was increased density of both the pulmonary lesions and the liver. These radiographic changes were consistent with amiodarone-induced toxicity; however, malignant disease was still a concern because of the patient's long history of smoking. Percutaneous fine-needle aspiration of the mass in the right upper lobe (guided by a CT scan) revealed numerous myofibroblasts with aggregates of foamy macrophages and chronic interstitial inflammation (Fig. 3). There was no evidence of malignant disease. Transmission electron microscopy confirmed the presence of multiple lamellar bodies within macrophages, consistent with amiodarone intake (Fig. 4). Microbiological cultures of the lung tissue were negative. Amiodarone-induced pulmonary toxicity was diagnosed. A repeat chest CT scan obtained 3 months after amiodarone therapy was stopped showed complete resolution of the mass (Fig. 5).

Fig. 2: Chest CT scan showing an irregular hyperdense mass in the right upper lobe.
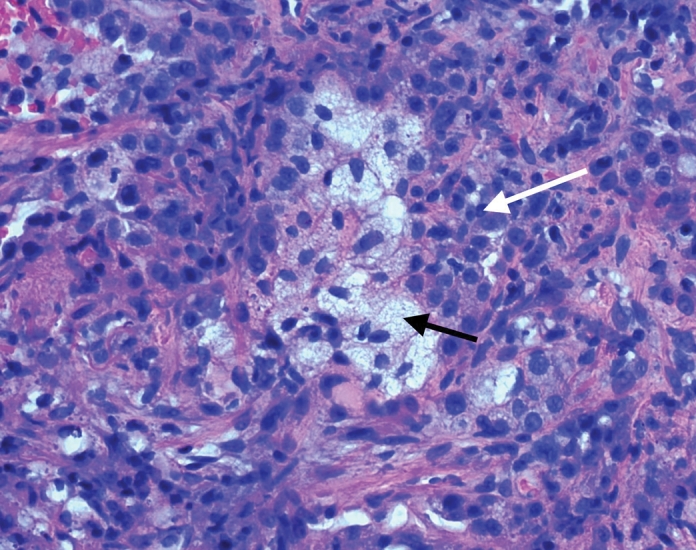
Fig. 3: Fine-needle aspirate showing numerous myofibroblasts with aggregates of foamy macrophages (black arrow) and chronic interstitial inflammation (white arrow; hematoxylin–eosin stain, original magnification × 400).
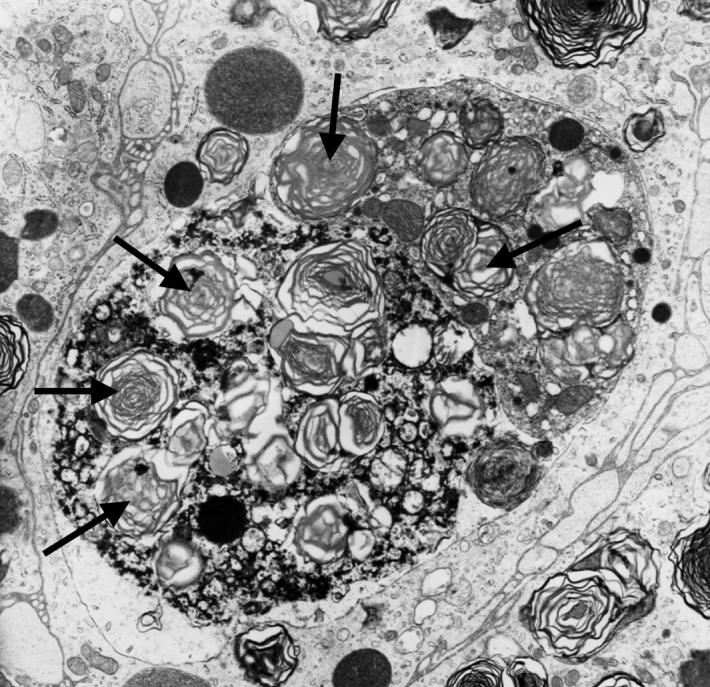
Fig. 4: Transmission electron micrograph of a core needle biopsy showing a macrophage with multiple lamellar bodies (arrows).

Fig. 5: Follow-up chest CT scan demonstrating resolution of mass at 3 months.
Amiodarone is a commonly prescribed antiarrhythmic benzofuran drug that has a variety of side effects that can involve the lung, liver, thyroid, cornea, skin and neuromuscular system. Pulmonary tox-icity is the most serious, yet potentially reversible, adverse effect. Although interstitial pneumonitis is the most common presentation, a range of abnormalities can be seen on a chest radiograph. There are no pathologic or radiographic abnormalities specific to amiodarone-induced pulmonary toxicity. Pulmonary toxicity is reported to develop in 0.5%–15% of patients who receive amiodarone therapy, although the frequency depends on the dose and duration of therapy.1 Risk factors include increasing age (e.g., > 50 years), dose greater than 400 mg/d and pre-existing lung disease. Previous studies support the notion that amiodarone-induced pulmonary toxicity correlates more closely with the total cumulative dose and duration of amiodarone therapy rather than with serum drug levels.1 Most cases develop within 12–18 months after the start of amiodarone therapy. Amiodarone is metabolized by the liver and has a long half-life (about 50 days).
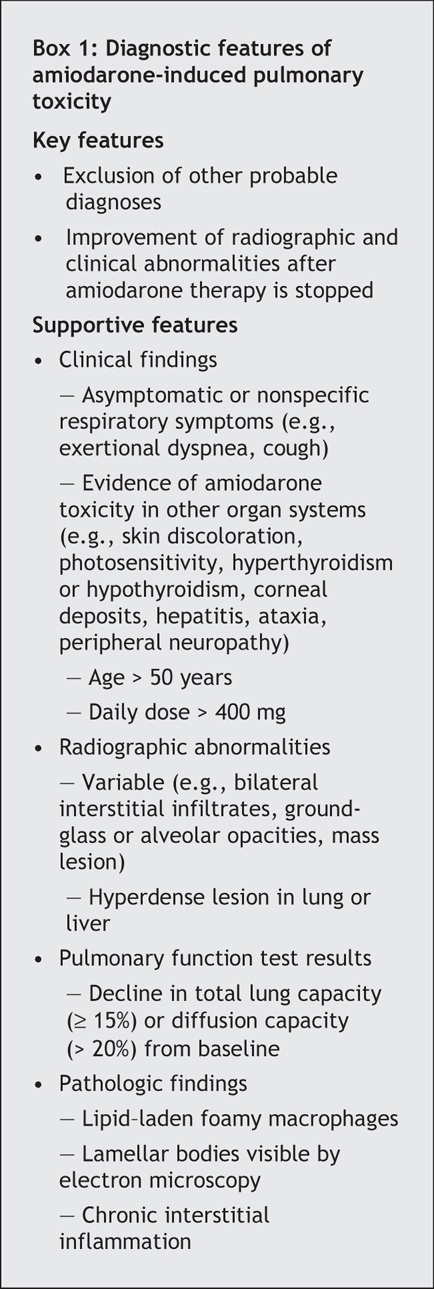
The mechanism of amiodarone-induced pulmonary toxicity is not entirely clear but is thought to be caused by direct cytotoxic damage and an indirect immune reaction. Amiodarone inhibits phospholipase A, which can result in an accumulation of phospholipids within lysosomes in the lungs and other tissues. Foamy lipid-laden macrophages and type 2 pneumocytes that contain whorled lamellar inclusion bodies are commonly seen during histologic and ultrastructural examination. Amiodarone-induced pulmonary toxicity can be diagnosed on the basis of a combination of clinical, radiologic and pathologic findings (Box 1) and is confirmed by improvement after discontinuation of amiodarone therapy and exclusion of other diagnoses. Follow-up radiographic images show complete resolution of the abnormalities in 85% of patients.1 Interstitial fibrosis, particularly if severe, is the least likely abnormality to resolve. Patients in whom acute respiratory distress syndrome develops have the highest mortality (up to 50%).
Box 1.
This case represents an unusual presentation of amiodarone-induced lung disease because the patient had a single pulmonary mass on the initial chest radiograph. In light of the patient's age and smoking history, the mass was initially suspected to be cancerous. There have been isolated case reports of similar presentations over the last 20 years;2,3 however, it is unclear why amiodarone-induced cellular toxicity and inflammation occurred in a localized fashion. Interestingly, all previously reported cases describe masses in the upper lobes of the lungs, particularly in the right upper lobe, as was seen in our patient. This case highlights the need to include amiodarone-induced pulmonary toxicity in the differential diagnosis of a solitary lung mass and also demonstrates that this phenomenon is reversible when amiodarone therapy is stopped.
When initiating amiodarone therapy, a chest radiograph and the results of pulmonary function tests, including lung volumes and diffusion capacity, should be obtained as baseline mea-surements. Longitudinal serial pulmonary function tests for all patients taking amiodarone therapy are currently not recommended. Patient education about the signs and symptoms of amiodarone-induced pulmonary toxicity and regular clinical follow-up are essential. An isolated drop in diffusion capacity should not prompt discontinuation of the amiodarone therapy, unless there is clinical or radiographic evidence of pulmonary toxicity. In our case, the patient had taken a cumulative dose of 300 g of amiodarone over 4 years. This report is also consistent with previous published reports in which patients had concomitant thyroid disease and liver toxicity.2,3 Amiodarone-related abnormalities in other organ systems should prompt physicians to consider amiodarone-induced pulmonary toxicity even in patients who do not report any respiratory symptoms.
Julie Jarand Division of Respiratory Medicine Department of Medicine Andrew Lee Department of Radiology Richard Leigh Division of Respiratory Medicine Department of Medicine University of Calgary Calgary, Alta.
Footnotes
This article was published in abstract form in Chest (2005;128:446S).
Competing interests: None declared.
REFERENCES
- 1.Camus P, Martin WJ, Rosenow EC. Amiodarone pulmonary toxicity. Clin Chest Med 2004;25:65-75. [DOI] [PubMed]
- 2.Arnon R, Raz I, Chajek-Shaul T, et al. Amiodarone pulmonary toxicity presenting as a solitary lung mass. Chest 1988;93:425-7. [DOI] [PubMed]
- 3.Piccione W, Faber P, Rosenberg MS. Amiodarone-induced pulmonary mass. Ann Thorac Surg 1989;47:918-9. [DOI] [PubMed]


