Abstract
To this day, a significant proportion of the human genome remains devoid of functional characterization. In this study, we present evidence that the previously functionally uncharacterized product of the human DHRS10 gene is endowed with 17β-HSD (17β-hydroxysteroid dehydrogenase) activity. 17β-HSD enzymes are primarily involved in the metabolism of steroids at the C-17 position and also of other substrates such as fatty acids, prostaglandins and xenobiotics. In vitro, DHRS10 converts NAD+ into NADH in the presence of oestradiol, testosterone and 5-androstene-3β,17β-diol. Furthermore, the product of oestradiol oxidation, oestrone, was identified in intact cells transfected with a construct plasmid encoding the DHRS10 protein. In situ fluorescence hybridization studies have revealed the cytoplasmic localization of DHRS10. Along with tissue expression data, this suggests a role for DHRS10 in the local inactivation of steroids in the central nervous system and placenta. The crystal structure of the DHRS10 apoenzyme exhibits secondary structure of the SDR (short-chain dehydrogenase/reductase) family: a Rossmann-fold with variable loops surrounding the active site. It also reveals a broad and deep active site cleft into which NAD+ and oestradiol can be docked in a catalytically competent orientation.
Keywords: crystal structure, DHRS10, 17β-hydroxysteroid dehydrogenase, pre-receptor control, short-chain dehydrogenase/reductase, steroid metabolism
Abbreviations: DHEA, dehydroepiandrosterone; ER, oestrogen receptor; GFP, green fluorescent protein; HEK-293T cells, HEK-293 cells (human embryonic kidney cells) expressing the large T-antigen of SV40 (simian virus 40); HSD, hydroxysteroid dehydrogenase; MDR, medium-chain dehydrogenase/reductase; NCS, non-crystallographic symmetry; RMSD, root mean square deviation; SDR, short-chain dehydrogenase/reductase; TCEP, tris-(2-carboxyethyl)phosphine
INTRODUCTION
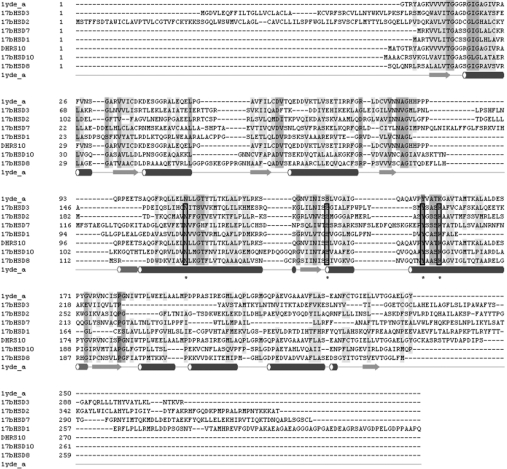
HSDs (hydroxysteroid dehydrogenases) catalyse the oxidoreduction of hydroxy/oxo groups of steroid hormones and in this manner regulate intracellular availability of steroid ligands to their nuclear receptors, and constitute a pre-receptor control mechanism [1,2]. All mammalian HSDs characterized to date are members of the AKRs (aldo/keto reductases) [3], MDRs (medium-chain dehydrogenases/reductases), or the SDR (short-chain dehydrogenase/reductase) families, with the clear majority of HSDs belonging to the latter family [4,5]. The main steroid-metabolizing activities regulating ligand access are oxidoreductases acting on positions 3, 11, 17 and 20, depending on the steroid hormone class. Whereas 3(α/β)-HSDs are involved in metabolism of all classes of steroid hormones, and 11β-HSDs and 20(α/β)-HSDs are restricted to glucocorticoids and progestins, 17β-HSDs play a central role in androgen and oestrogen physiology. At present, 13 different isoforms of 17β-HSDs have been characterized, and with the exception of 17β-HSD5 all are members of the SDR family [6–8]. They differ in nucleotide cofactor [NAD(H) or NADP(H)] and steroid substrate (androgen/oestrogen) specificity, subcellular compartmentalization and tissue-specific expression patterns. Accordingly, 17β-HSDs are numbered in chronological order according to their date of discovery. These HSDs can be grouped into in vivo oxidative enzymes (17β-HSD type 2, 4, 6, 8, 9, 10, 11 and 12) catalysing the NAD+-dependent inactivation of steroid receptor ligands, or into in vivo reductive enzymes (17β-HSD type 1, 3, 5 and 7) which are NADPH-dependent and whose reactions lead to steroid receptor ligands. A specific feature of most 17β-HSDs is their remarkably broad substrate specificity, as observed in particular with fatty acyl-CoA derivatives (with type 4 and 10 17β-HSDs) or retinoic acid metabolites (observed with murine type 6 and 9 17β-HSDs). A multiple sequence alignment of human 17β-HSDs is given in Figure 1.
Figure 1. Multiple sequence alignment of selected human 17β-HSDs.
Active site motifs (see text) are highlighted through boxing and marked by asterisks. Secondary structure elements as determined for DHRS10 are indicated below the alignment as arrows (extended strands) and tubes (α helices).
The present study concerns the characterization of the product of the human DHRS10 gene. We show that DHRS10 possesses 17β-HSD functionality both in vivo and in vitro and that its structure shares a common architecture with most of 17β-HSD enzymes. The DHRS10 cDNA was previously isolated from retina epithelium [9], was initially termed retSDR3 and is currently annotated as ‘DHRS10’ in the HUGO Gene Nomenclature Database [10]. The encoded SDR enzyme was originally suspected to function in retinol metabolism as an oxidoreductase, a role that could not be verified experimentally [9].
The functional annotation as 17β-HSD described in the present paper forms the basis for the proposal to rename the human DHRS10 gene as HSD17B14.
EXPERIMENTAL
Cloning of human DHRS10
A cDNA coding for human DHRS10 was obtained by gene synthesis using codon optimization for expression in Escherichia coli (Genscript). The insert DNA was subcloned into a bacterial pET-based expression vector, in frame into NdeI and BamHI sites, resulting in a variant containing an N-terminal His6 tag, followed by a TEV (tobacco etch virus) protease cleavage site. For expression in cell culture or for Northern-blot analysis, human DHRS10 cDNA was amplified from HEK-293T [HEK-293 cells (human embryonic kidney cells) expressing the large T-antigen of SV40 (simian virus 40)] cDNA using PCR with specific primers [for Northern blot, probe forward: 5′-GAGGTGAAAGAGGCCCAGAGTAG-3′, reverse: 5′-GTGACCCGGCACCTTGCTAAC-3′; for cloning into pcDNA3 (Invitrogen): 5′-TATAGGATCCATGGCTACGGGAACGCGCTATGCC-3′, reverse: 5′-TTAAGAATTCTCAGGAAGGGATATCGGGGGCGTC-3′; for cloning into pcDNA4 Myc-His (Invitrogen): 5′-TATAGGATCCGCCACCATGGCTACGGGAACGCGCTATGCC-3′, reverse: 5′-TTAACCGCGGGGAAGGGATATCGGGGGCGTCCAC-3′; for cloning into pEGFP-C2 (BD Biosciences, Heidelberg, Germany): 5′-TATAGAATTCATGGCTACGGGAACGCGCTATGCC-3′, reverse: 5′-TTAAGGATCCTTCAGGAAGGGATATCGGGGGCGTC-3′). Inserts were verified by dideoxy sequence analysis using vector-specific primers. For transfection, DNA was isolated using the PureYield Midi kit (Promega, Mannheim, Germany) according to the manufacturer's instructions.
Heterologous expression in E. coli and purification of recombinant protein
The plasmid was transformed into Rosetta 2 (DE3) strain, and cells were grown overnight in 1 litre of Teriffic Broth containing 34 μg/ml chloramphenicol and 100 μg/ml ampicillin in a 2.5 litre baffled flask at 37 °C. Protein expression was induced by addition of 100 μM IPTG (isopropyl β-D-thiogalactoside) to cells that had been grown to a D600 of 0.6. The temperature was lowered to 15 °C and the culture was continued for a further 20 h. The cells were harvested and stored at −80 °C. The frozen cell pellet was resuspended in 30 ml of 50 mM Hepes (pH 7.5), 500 mM NaCl, 5 mM imidazole and 0.5 mM TCEP [tris-(2-carboxyethyl)phosphine]. The cells were then disrupted using a high-pressure homogenizer (Emulsiflex-C5, Avestin). Following centrifugation (35000 g, 40 min and 4 °C) the clarified supernatant was passed through a 10 ml DE-52 column to remove DNA. The flow through was applied to a 2 ml Ni-NTA (Ni2+-nitrilotriacetate; Qiagen) column, washed with 20 ml of 50 mM Tris/HCl (pH 7.5), 500 mM NaCl, 5 mM imidazole and 0.5 mM TCEP and eluted by raising the imidazole concentration to 250 mM. The eluted peak was loaded on to an S75 16/60 prep grade (GE/Amersham) gel filtration column in 10 mM Hepes (pH 7.5), 500 mM NaCl, 5% (v/v) glycerol and 0.5 mM TCEP. The essentially pure DHRS10-containing peak was concentrated (Vivaspin 20; Vivascience; molecular-mass cut-off 15 kDa) to a final concentration of 12 mg/ml. After flash freezing in liquid nitrogen, the protein was stored at −80 °C for further analysis by crystallization or substrate screening. The mass of the purified product was verified by LC (liquid chromatography)/MS on an Agilent LC/MSD TOF (time-of-flight) system (Agilent).
Crystallization and structure determination
Crystals were grown by the sitting drop vapour diffusion method in 24-well sitting drop Cryschem plates (Hampton Research) at 20 °C. The concentrated protein (2 μl) was mixed with 2 μl of 0.2 M magnesium acetate, 0.1 M sodium cacodylate (pH 6.5) and 20% (v/v) MPD (2-methyl-2,4-pentanediol). The crystals were flash cooled in liquid nitrogen and X-ray diffraction data were collected at 100 K, at beamline 17-ID [APS (advanced photon source); Argonne, IL, U.S.A.] at a wavelength of 0.9794 Å (1 Å=0.1 nm). Data were indexed, integrated and scaled using the HKL2000 suite [11]. Phases were obtained by molecular replacement using the program PHASER [12]. Since a single highest homology model did not give a molecular replacement solution, a superimposed ensemble of 11 homologous structures (sequence identity between 30 and 38%) was used as a molecular replacement model. Refinement was initiated using strict NCS (non-crystallographic symmetry) constraints in CNS [13]. However, in later stages it became apparent that the four tetramers in the asymmetric unit have A2B2 symmetry, the main difference between molecule A and B being the conformation of a 20-residue loop (residues 190–210). At this point, refinement was continued with refmac5 [14], imposing tight NCS restraints on appropriate molecules. Refinement was alternated with RESOLVE [15] run in prime-and-switch mode to remove model bias. Refinement converged to a crystallographic R-factor of 0.181 and Rfree of 0.229. The co-ordinates and structure factors were deposited in the PDB with the code 1YDE.
Ligand docking
Two consecutive ligand docking procedures were performed according to the methodology described by Abagyan and Totrov [16,17] and implemented in the program ICM versus 3.4-1: one to position the NAD+ molecule into the cofactor-binding pocket and a second one to dock the oestradiol molecule into the active site of DHRS10. In both cases, grid maps representing different properties of the enzyme were computed. During the docking, either one of the torsional angles of the ligand was randomly changed or a pseudo-Brownian move was performed. Each random change was followed by 100 steps of local conjugate-gradient minimization. The new conformation was accepted or rejected according to metropolis criteria using a temperature of 600 K. The length (number of Monte Carlo steps) of the docking run as well as the length of local minimization was determined automatically by an adaptive algorithm, depending on the size and number of flexible torsions in the ligand. The lowest energy conformation satisfying the absence of clashes after docking NAD+ was incorporated into the structure file of DHRS10 and this was in turn used as receptor for the docking of oestradiol. In this second docking, a positional restraint was imposed on the O17 atom of oestradiol and the Tyr154-OH, based on the catalytic mechanism of SDR enzymes [18,19].
Substrate screening and kinetic analysis of purified recombinant human DHRS10
A compound library comprising 50 different steroids (androgen, oestrogen, progestin, glucocorticoid hormones, bile acids and oxysterols; obtained from Sigma and Steraloids) with hydroxy/keto functions at position 3, 7, 11, 17, 20 and 21 were screened against purified human DHRS10 using a fluorescence-based assay on cofactor fluorescence change in a Spectramax M2 microplate reader (Molecular Devices). Steroids were dissolved in DMSO with stock solutions ranging from 5 to 20 mM, and were further diluted 1:1000 in the assay mixture (oxidation: 50 mM Tris/HCl, pH 8.5, 100 mM NaCl, 200 μM NAD+ or NADP+ and 50–100 μg/ml enzyme; reduction: 50 mM Tris/HCl, pH 7.5, 100 mM NaCl and 10 μM NADH or NADPH). Excitation was set to 340 nm, emission was at 460 nm, and the assay was conducted in 96-well plates (Costar). Initial hits from this screen were verified by analysis of product formation using radioactively labelled steroids with an HPLC system coupled with online radioactivity detection. Kinetic analysis was carried out in 96-well plates as described above, or in single, 10 mm pathlength quartz cuvettes, by varying steroid substrate (200 nM–100 μM) and cofactor (0.1 μM–10 mM) concentrations. Initial velocities were converted into product formation using freshly prepared nucleotide cofactor solutions as standards, and data obtained were fitted by non-linear regression to the Michaelis–Menten equation using SigmaPlot or GraphPad software packages.
Cell culture and transfection
HEK-293T, SaOS-2 and HeLa cells were grown under humidified standard conditions (37 °C and 5% CO2) in high-glucose Dulbecco's modified Eagle's medium (Invitrogen, Karlsruhe, Germany) supplemented with 10% (v/v) foetal bovine serum (Biochrom AG, Berlin, Germany), 2 mM L-Glutamax I (Invitrogen) and 100 units/ml penicillin/100 μg/ml streptomycin. For transfection, FuGENE™ 6 transfection reagent (Roche Biosciences, Mannheim, Germany) was used according to the manufacturer's instructions. For metabolite analysis, HEK-293T cells were seeded on to 12-well plates (Nunc, Wiesbaden, Germany) and grown overnight before transfection. Twenty-four hours after transfection, 1 μl of [2,4,6,7-3H(N)]oestradiol (final concentration 20 nM) (PerkinElmer, Wellesley, MA, U.S.A.) was added to cell culture medium and incubation was continued. Cell culture medium was collected at different time points, and purified with Strata-C18E columns (Phenomenex, Aschaffenburg, Germany). Samples were then analysed on HPLC (Beckman, Fullerton, CA, U.S.A.) with 43% (v/v) acetonitrile (in water) on a Luna C-18 column (Phenomenex). Conversion rates were obtained after integration of chromatograms and evaluated with 24Karat-software (Beckman). For analysis of subcellular localization, HeLa or SaOS-2 cells were seeded on to coverslips. After 24 h, cells were transfected and grown for a further 24 h. For counterstaining of mitochondria MitoTracker Orange was used, for nuclear counterstaining Hoechst 33342 and for F-actin counterstaining, Alexa Fluor® 568 phalloidin (all Invitrogen). For immunochemical detection of the Myc tag 9B11 mouse monoclonal antibody (Cell Signaling Technology, NEB, Frankfurt a.M., Germany) was used as the primary antibody and the secondary antibody was Alexa Fluor® 488 goat anti-mouse IgG (Invitrogen). After fixation and staining, coverslips were mounted on to slides using Vectashield (Vector Laboratories, Burlingame, CA, U.S.A.). Subcellular localization was analysed by Zeiss Axiophot fluorescence microscope (Carl Zeiss, Oberkochen, Germany) with the ISIS (MetaSystems, Altlussheim, Germany) image processing software.
Expression analysis of DHRS10 in human tissues
FirstChoice Northern Blot Human Blot II (Ambion) was used with recommended wash solutions and Ultrahyb hybridization solution according to the manufacturer's instructions. The PCR product used as a probe for Northern blot was labelled with a Strip-EZ DNA kit (Ambion, Huntington, U.K.). Radioactively labelled nucleotides were purchased from Amersham Biosciences (Uppsala, Sweden). Detection was by autoradiography using BioMax XAR films (Kodak Industrie, Chalon-sur-Saône, Cedex, France).
RESULTS
Expression, purification and activity of human DHRS10
Full-length DHRS10 was expressed and purified in a two-step chromatographic procedure yielding approx. 20 mg/l of culture. The purified protein was judged homogeneous by SDS/PAGE and MS (results not shown), and was found suitable for subsequent use in substrate screening, kinetic and crystallographic studies. A fluorescent assay was used to carry out substrate screening against a collection of different steroids. Purified DHRS10 enzyme converted NAD+ into NADH in the presence of oestradiol, testosterone or 5-androstene-3β,17β-diol. Michaelis–Menten kinetics were observed for oestradiol and 5-androstene-3β,17β-diol; with Km values of 5.6±1.7 and 13.6±1.6 μM and Vmax values of 2.5±1.0 and 9.1±1.6 nmol of NADH·min−1·mg−1 for oestradiol and 5-androstene-3β,17β-diol respectively. However, non-saturable kinetics were found for testosterone (Figure 2, Table 1). No conversion was observed in the presence of NADP(H) or with β-OH-butyryl CoA, which is a bona fide substrate for other 17β-HSDs such as 17β-HSD4 and 17β-HSD10 (Table 1).
Figure 2. Oxidation of oestradiol by human DHRS10.
(A) In vivo kinetics for the formation of radioactively labelled oestrone from oestradiol over a period of time in HEK-293T cells transfected with DHRS10. As a control, cells were also mock transformed with the pcDNA3 vector only. The net conversion is the percentage conversion carried out by DHRS10-transfected cells after subtracting the percentage conversion carried out by mock-transfected cells at the same time point. (B) Typical separation of oestradiol and oestrone by HPLC. CPS, counts per second; rt, retention time; E2, oestradiol; E1, oestrone. Unlabelled peaks correspond to autoradiolytic products of substrate (oestradiol) decay. (C) Michaelis–Menten plot for the in vitro conversion of NAD+ into NADH in the presence of oestradiol.
Table 1. Kinetic parameters determined for human DHRS10 using NAD+ as cofactor.
Abbreviation: n.d., no activity detectable. Number of experiments: n=3–4.
| Substrate | Km (μM) | Vmax (nmol of NADH· min−1·mg−1) | kcat (min−1) |
|---|---|---|---|
| Oestradiol | 5.6±1.7 | 2.5±1.0 | 0.076±0.026 |
| Testosterone | 470* | 2.6* | − |
| 5-Androstene-3β,17β-diol | 13.6±1.6 | 9.1±1.6 | 0.28±0.05 |
| OH-butyryl-CoA | n.d. | − | − |
| NADP+ | n.d. | − | − |
*Estimated Km and Vmax, due to non-saturable kinetics.
DHRS10 activity in intact cells
In order to verify steroid conversion by DHRS10 in intact cells and to investigate the direction of the DHRS10 reaction in vivo, HEK-293T cells were transfected with an expression plasmid encoding DHRS10 and exposed to 20 nM radiolabelled oestradiol. The transfected cells efficiently oxidized oestradiol to oestrone as revealed by HPLC analysis of the supernatant (Figure 2B). This conversion rate is significantly higher compared with that of mock-transfected cells (pcDNA3 vector only). Therefore intact cells expressing DHRS10 can indeed oxidize steroids at physiological concentrations.
Crystal structure of DHRS10
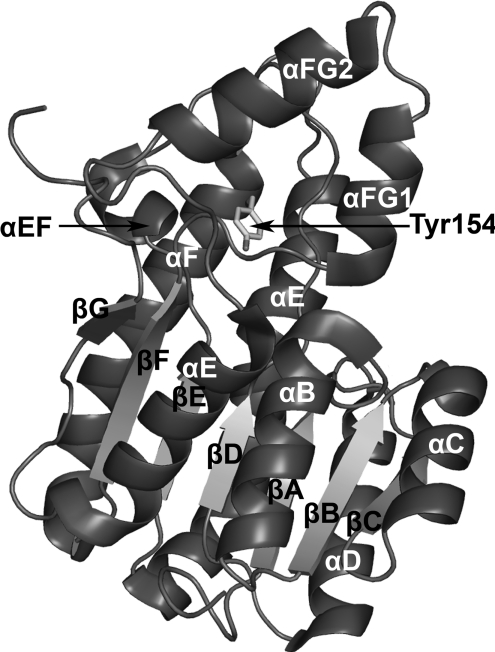
Following extensive crystallization trials, the purified protein yielded well diffracting crystals suitable for crystallographic analysis. The crystal structure of DHRS10 was solved by molecular replacement to a resolution of 2.4 Å, and a summary of the data processing and refinement statistics is compiled in Table 2. The asymmetric unit contains 16 DHRS10 monomers arranged as four tetramers with 222-point group symmetry. Each monomer comprises two distinct regions (Figure 3): the first region is a Rossmann-fold built up of a central β-sheet core consisting of seven parallel β-strands (βA–βG) sandwiched between two arrays of parallel helices (αB–αG). This region has a characteristic nucleotide cofactor [NAD(H) or NADP(H)]-binding motif T-G-X3-G-X-G located near its N-terminus. Residue Asp40 is present at the C-terminal end of the second β-strand (βB). In SDR structures the presence of an acidic residue at this location indicates a NAD(H) versus NAD(P) selectivity, since the carboxylate group is in a favourable location to interact with the 2′- and 3′-OH groups of the adenosine ribose of NAD. Accordingly, this residue prohibits NADP(H) binding by repelling the negative charge on the 2′-phosphate and thus confers NAD(H) specificity to DHRS10 [20]. Kinetic analysis (see above) confirmed NAD(H) as the cofactor for the DHRS10 reaction. Also within this region is a very short α-helix (αEF) inserted between αE and βF and encompassing residues 142–147. A second region contains two additional α-helical elements αFG1 (residues 189–197) and αFG2 (residues 201–212) that are inserted between βF and αG. As with all SDRs whose structures have been determined so far, this second region is more variable and is responsible for substrate binding.
Table 2. Data processing and refinement statistics for DHRS10 crystal structure.
| Parameter | Value |
|---|---|
| Data processing | |
| Wavelength (Å) | 0.9794 |
| Space group | P1211 |
| Unit cell parameters (Å, °) | 167.1, 98.8; 167.5, 90.0; 115.9, 90.0 |
| Resolution range (outer shell) (Å) | 82.6–2.4 (2.5–2.4) |
| Observed reflections (outer shell) | 558993 (13185) |
| Unique reflections (outer shell) | 176307 (12096) |
| Completeness (outer shell) (%) | 91.9 (55.2) |
| Mean I/σI (outer shell) | 9.1 (1.6) |
| Multiplicity (outer shell) | 2.9 (1.1) |
| Rmerge (outer shell) | 0.117 (0.575) |
| VM (Å3·Da−1) | 2.5 |
| Refinement | |
| Protein atoms | 29419 |
| Protein residues (per chain) | A, 250, B, 247; C, 250; D, 255; E, 250; F, 256; G, 247; H, 254; I, 247; J, 255; K, 250; L, 255; M, 244; N, 240; O, 247; P, 254 |
| Water molecules in model | 1251 |
| Rwork | 0.181 |
| Rfree | 0.229 |
| RMSD | |
| Bond lengths (Å) | 0.016 |
| Bond angles (°) | 1.505 |
| Average B factor (Å2) | |
| Main chain (per chain) | 4.485 |
| Side chain (per chain) | 7.187 |
| Water molecules | 4.650 |
| PDB code | 1YDE |
Figure 3. The secondary structure of DHRS10.
The side chain of the catalytic Tyr154 is shown in stick representation. (All structural representations were drawn with the program PyMOL.)
In the apostructure determined, a broad active site cleft lies between the two regions (Figures 3 and 5). Apart from the highly conserved catalytic triad that consists of Ser141, Tyr154 and Lys158, this active site cleft contains a number of hydrophobic residues potentially involved in binding of hydrophobic substrates (Figure 4).
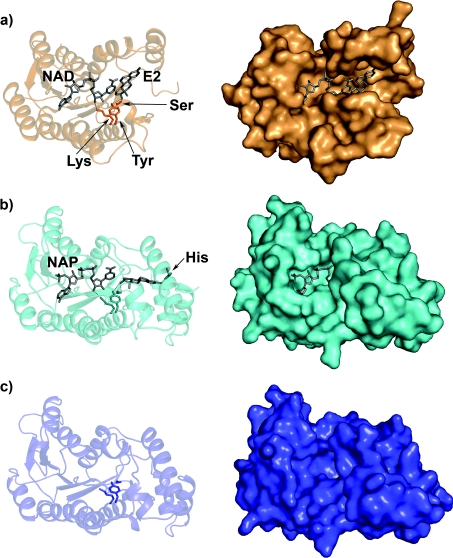
Figure 5. Comparison of the DHRS10 structure with the structures of ternary complex and apoenzyme 17β-HSD1.
The panels on the left show the various structures in ribbon representation set at 80% transparency and the panels on the right show the structures in the same orientation in surface representation. (a) The structure of DHRS10 apoenzyme (PDB code 1YDE) with modelled NAD+ and oestradiol (E2) shown in grey stick representation. The catalytic residues Tyr154, Lys158 and Ser141 are in orange stick representation. (b) The crystal structure of the 17β-HSD1 ternary complex containing NADP+ (NAP) and oestradiol (E2) (PDB code 1FDT). The catalytic residues Tyr155, Lys159 and Ser142 are shown in cyan stick representation. (c) The structure of the 17β-HSD1 (PDB code 1BHS) apoenzyme. The catalytic residues are shown in blue stick representation.
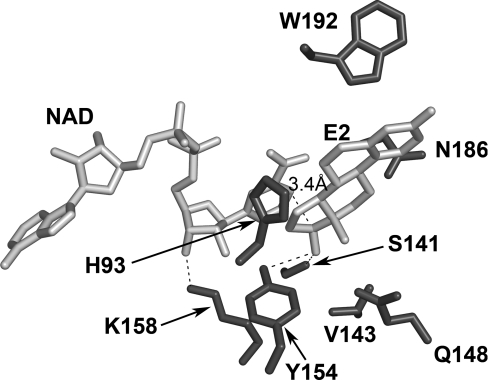
Figure 4. Detailed view of the active site of DHRS10.
Modelled NAD+ and oestradiol (E2) are shown in grey stick representation and side chains of residues belonging to DHRS10 are shown in dark grey stick representation. The distance measurement (3.4 Å) between C-4 of nicotinamide and C-17 of the steroid is shown in black dashed line and other polar contacts under 3.2 Å are shown in unlabelled dashed lines.
Ligand docking into the DHRS10 active site
Although numerous co-crystallization experiments were attempted, DHRS10 crystallized as an apoenzyme with no cofactor or substrate in the active site. In order to understand the interactions of DHRS10 with its cofactor and substrate on a molecular level, in silico ligand docking was performed on the protein monomer.
Starting models for the oestradiol substrate and NAD+ cofactor were obtained from the crystal structure of rat 17β-HSD10 (also known as type II 3-hydroxyacyl-CoA dehydrogenase, PDB code 1E6W). The in silico docking of NAD+ yielded a very satisfactory conformation for both protein and cofactor. The docked NAD+ molecule presented an RMSD (root mean square deviation) of 0.855 Å for all atoms when compared with the NAD+ cofactor of type II 3-hydroxyacyl-CoA dehydrogenase. The small difference was expected since the cofactor-binding pocket is not completely conserved and small variations in the binding pose are expected in these situations. In spite of this, the overall geometry of the DHRS10-binding pocket has been preserved and NAD+ could be docked in a manner very similar to that observed in 1E6W.
The docking of oestradiol to the DHRS10–NAD+ model can be achieved by placing the atom O-17 of oestradiol within the proximity of the catalytic tyrosine (Tyr154) while keeping the atom C-17 close enough to C-4 of the nicotinamide for hydride transfer during catalysis (3.4 Å) (Figure 4). Consequently the C-17 hydroxyl is within hydrogen-bonding distance of Tyr154 (3.2 Å) and Ser141 (3.0 Å). In this conformation the remainder of the environment of the oestradiol molecule is made up of a mixture of polar and non-polar residues: His93, Val143, Gln148, Trp192 and Asn186 lie within 4 Å of the oestradiol molecule and contribute to van der Waals interactions with oestradiol. There are no residues that contribute to additional hydrogen bonding with oestradiol.
A structural comparison of DHRS10 with docked NAD/oestradiol was carried out with the crystal structure of the ternary complex of 17β-HSD1 with NADP/oestradiol (PDB code 1FDT), apo-17β-HSD1 (PDB code 1BHS) and to other structures of members of the 17β-HSD family. The DHRS10 molecule possesses a prominent broad and open active site cleft that is not observed in 17β-HSD1 (Figure 5) or other 17β-HSDs (results not shown). Within this cleft the docked oestradiol molecule sits rather loosely. Again this is in contrast with 17β-HSD1 where oestradiol interactions are better defined. Here, the oestradiol is stabilized by three rather than two hydrogen bonds: two to the catalytic serine and tyrosine residues and an additional hydrogen bond between oestradiol O3 and Nϵ2 of His221 [21]. Additionally, a number of neighbouring residues contribute to hydrophobic interactions with the core of the steroid.
Nonetheless the docking procedure employed within does not take into account the possible conformational changes to the DHRS10 structure induced by binding of cofactor or substrate. Consequently, the milieu of the oestradiol could be significantly different in the secondary or tertiary complex of DHRS10.
Interestingly, a comparison of the apo and ternary complex structure of 17β-HSD1 reveals that although some structural rearrangement does occur in the loop connecting βF and αFG1, overall the active site remains closed in both structures (Figure 5).
Subcellular localization of DHRS10
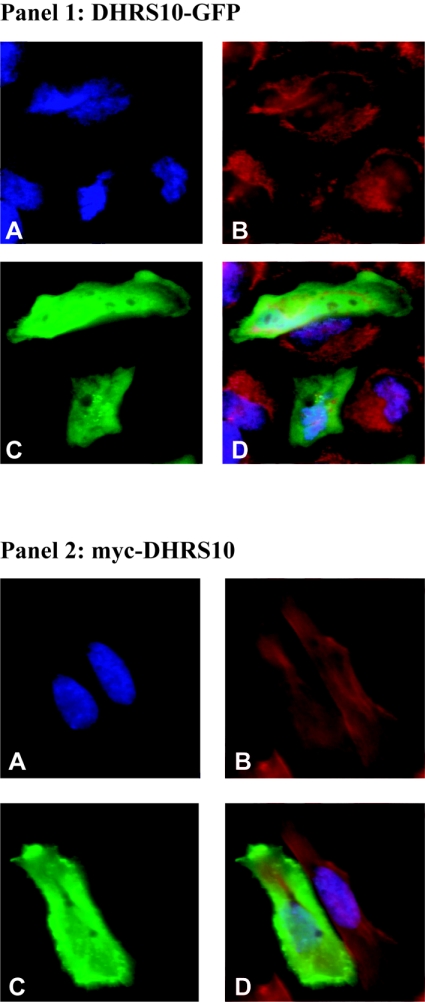
Immunofluorescence subcellular localization studies were carried out where a DHRS10 construct with a Myc tag at its N-terminus was probed with a primary anti-Myc monoclonal mouse antibody and a secondary fluorescent antibody. To eliminate the possibility of the N-terminal tag interfering with the proper targeting of the DHRS10 protein, in situ fluorescence experiments were also carried out on HeLa cells expressing human DHRS10 with a GFP (green fluorescent protein) tag at its C-terminus. In both cases the studies clearly reveal the cytoplasmic localization of DHRS10 protein (Figure 6). No mitochondrial or nuclear targeting could be observed using fluorescent mitochondrial (results not shown) and nuclear reporter dyes.
Figure 6. Cytosolic localization of human DHRS10.
(Panel 1) A shows nuclear counterstaining with the blue fluorescent dye Hoechst 33342, B shows mitochondrial counterstaining with the orange fluorescent dye MitoTracker Orange and C shows green fluorescence due to expression of GFP tag at the C-terminus of DHRS10. D is an overlay of the previous three inserts. (Panel 2) The Figure is arranged as above except that B shows phalloidin staining for F-actin and C shows immunofluorescence due to the probing of the Myc tag at the N-terminus of DHRS10 with a primary anti-Myc 9B11 mouse monoclonal antibody and a secondary green fluorescent Alexa Fluor® goat anti-mouse IgG antibody.
Expression analysis of DHRS10 in human tissues
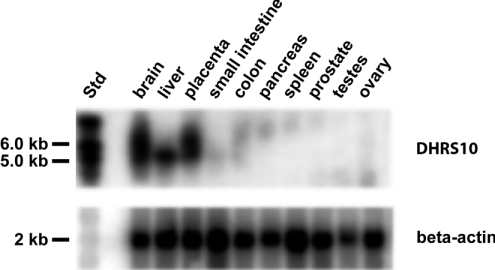
Northern-blot analysis using a radioactively labelled probe of DHRS10 was carried out on selected human tissues (Figure 7). High expression is observed in brain, liver and placenta, whereas no or low signals are observed in small intestine, colon, pancreas, spleen and gonads (testes and ovary). Two distinct sizes of specific signals are observed (∼5.5 and 7 kbp), indicating two distinct transcription or splicing sites in brain and placenta, whereas in liver only one mRNA species is observed (Figure 7).
Figure 7. Northern-blot analysis of DHRS10 in human tissues.
mRNA from various human tissues was probed with a 32P-labelled DHRS10 probe. RNA molecular mass standards are shown on the left-hand side. Loading control hybridization with a 32P-labelled probe for β-actin is also shown.
DISCUSSION
In the present study, we have identified DHRS10 as a cytosolic SDR enzyme with 17β-HSD activity on steroid substrates. Out of the human tissues investigated the highest levels of DHRS10 expression were observed in the brain, liver and placenta.
The DHRS10 gene was initially cloned in an attempt to define retinoid metabolizing enzymes; however, this function was excluded after heterologous expression [9]. To our knowledge, no further functional studies are available on this human gene or any mammalian orthologue. To investigate the structural and functional features of the enzyme, we determined the crystal structure and correlated these results to functional analyses. To this end, experimental structure determination appears to be essential to derive functional conclusions. We performed homology modelling of human DHRS10 using the two closest available structures as templates, namely Rv2002 gene product from Mycobacterium tuberculosis (PDB code 1NFQ) and TT0321 from Thermus thermophilus HB8 (PDB code 2D1Y), both with 38% sequence identity. Although the predicted folding was very similar to the experimental structure, and homology modelling could be performed in a satisfactory manner for most of the molecule, an important active site segment comprising ∼14 residues was not correctly predicted due to high sequence variation. Thus a docking analysis to suggest possible substrates for de-orphanization of DHRS10 could not be carried out due to the lack of reliable templates for this critical portion of the structure. Structure prediction for a segment with such size to the level required for de-orphanization via docking methods is therefore still beyond the reach of present technology.
In common with most of the 17β-HSDs, the crystal structure displays the typical characteristics of the SDR family with a largely conserved fold and the presence of catalytically important residues, Asn114, Ser141, Tyr154 and Lys158 (Figure 1) [19]. Interestingly, a deep and broad active site cleft is found within the DHRS10 structure. This feature is more prominent than in other 17β-HSDs for which three-dimensional structures have been determined to date. As well as demonstrating that this protein converts 17β-OH steroids such as oestradiol into oestrone both in vivo and in vitro, we also show that NAD+ and oestradiol can be docked within the cleft in a catalytically competent conformation. The present study reveals the molecular details of the enzyme–substrate–cofactor interaction and shows that the oestradiol substrate sits rather loosely within the active site cleft. Such a conformation has several possible implications. First, it might explain the rather low catalytic turnover value for the in vitro DHRS10 reaction. However, the low kcat value for DHRS10 is not entirely unusual and a number of other SDR enzymes have similarly low kcat values for substrates that have nevertheless been shown to be relevant in their physiological context. The latter is exemplified by human 11β-HSD1, which carries out metabolic activation of the glucocorticoid hormone cortisol from the precursor cortisone. The determined kcat for cortisone reduction is only approx. 20 times higher [22] than the kcat value for the DHRS10/NAD+/oestradiol reaction, yet the in vivo importance of this reaction has been demonstrated on a number of occasions and is highlighted by its involvement in metabolic diseases such as obesity and insulin resistance [23–26]. Furthermore, human 17β-HSD10 displays an approx. 10-fold higher kcat than DHRS10/NAD+/oestradiol [22]; however, the Km of 17β-HSD10 for this reaction is approx. 5-fold higher, suggesting that 17β-HSD10 and DHRS10 have similar kcat/Km values. Secondly, the broad active site cleft suggests that the DHRS10 enzyme might have other substrate specificities besides oestradiol since the active site cleft is wide enough to accommodate larger substrates than steroid molecules. This broad substrate spectrum appears to be a hallmark for 17β-HSDs, and accordingly, broad substrate specificity has been demonstrated for a number of 17β-HSDs such as type 4, 6 and 10 [2,8]. In addition, wider substrate specificity of DHRS10 is also possible, as deduced from a phylogenetic analysis that shows that DHRS10 clusters with SDR proteins such as PECR (peroxisomal trans-2-enoyl-CoA reductase) [27,28] and mitochondrial DECR1 (2,4-dienoyl CoA reductase 1) [29,30] whose primary roles are in converting fatty-acyl CoAs rather than steroids (results not shown). However, an initial screen with a limited number of compounds (comprising >200 compounds including CoA derivatives) as possible substrates or ligands for SDR enzymes did not reveal any significant binding except for oestrogen-based steroids (results not shown). Thirdly, it is also possible that the extensive and open active site cleft is a feature of the apoenzyme and that the cleft might undergo a conformational change and close when ligands are bound.
Together with the expression observed in tissues such as liver, brain and placenta, the proven in vivo and in vitro functions of DHRS10 as oxidative 17β-hydroxy dehydrogenase suggest possible roles for DHRS10 in the local regulation of active steroid hormones levels [1,2]. DHRS10 would therefore be responsible for steroid inactivation similar to 17β-HSD2. However, as shown in the present study, the tissue distribution of DHRS10 is distinct from that reported for type 2 [31,32] and because of that a tissue-specific function is postulated. This is in analogy to other 17β- or 11β-HSD enzymes that constitute critical determinants of steroid hormone physiology [1]. It appears in several situations essential that steroid ligands are excluded from their receptors, as is the case with glucocorticoids and the mineralocorticoid receptor.
Our in vitro results indicate that DHRS10 is involved in the local inactivation of 5-androstene-3β,17β-diol and of oestradiol, and taken together with the initial expression data obtained in the present study, suggest possible functional roles mainly in the placenta and the central nervous system. The activity and expression in the central nervous system thus adds DHRS10 isoenzyme to the complexity of oestrogen and DHEA (dehydroepiandrosterone)-metabolizing steroid dehydrogenases observed in a study conducted by Steckelbroeck et al. [33], noting multiple 17β-HSDs involved in human brain tissues. The weak oestrogenic steroid 5-androstene-3β,17β-diol is an important metabolic intermediate in the peripheral sex steroid synthesis starting from DHEA. 5-Androstene-3β,17β-diol is secreted by the adrenal gland, and like the sex steroids display important functions in the brain such as hippocampal neurogenesis and neural survival [34]. Oestrogens have an extensive range of effects on the brain [35]. These include effects on brain development [36], centrally regulated effects on reproduction, mood [37], cognition [38], protection from neurotoxins/neurodegeneration or injury [39,40], neuron plasticity [41], transcription of neuropeptides [42] and regulative effects on the enzymes that affect the synthesis and turnover of classical neurotransmitters, e.g. serotonin [43] and dopamine [44].
It is clear that the cytosolic localization of DHRS10 could allow ‘control by access’ by limiting exogenously and endogenously produced active oestrogen (oestradiol) from reaching ERs (oestrogen receptors) ERα/β located in the nucleus. Interestingly, surface membrane-associated ERs, whose existence has also been recently demonstrated [45,46], would allow bypass of such a control.
Taken together, we have provided a structural and functional characterization of an as yet poorly documented mammalian gene product. Further studies concerning temporal and spatial expression patterns, animal studies, as well as a search for other possible substrate activities will be mandatory for the additional characterization of this SDR member.
Acknowledgments
The Structural Genomics Consortium is a registered charity (number 1097737) funded by the Wellcome Trust, GlaxoSmithKline, Genome Canada, the Canadian Institutes of Health Research, the Ontario Innovation Trust, the Ontario Research and Development Challenge Fund, the Canadian Foundation for Innovation; Vinnova, Knut and Alice Wallenberg Foundation; and Karolinska Institutet. Data collection by Dr F. von Delft (Structural Genomics Consortium, University of Oxford, Oxford, U.K.) is gratefully acknowledged.
References
- 1.Nobel S., Abrahmsen L., Oppermann U. Metabolic conversion as a pre-receptor control mechanism for lipophilic hormones. Eur. J. Biochem. 2001;268:4113–4125. doi: 10.1046/j.1432-1327.2001.02359.x. [DOI] [PubMed] [Google Scholar]
- 2.Mindnich R., Moller G., Adamski J. The role of 17 beta-hydroxysteroid dehydrogenases. Mol. Cell. Endocrinol. 2004;218:7–20. doi: 10.1016/j.mce.2003.12.006. [DOI] [PubMed] [Google Scholar]
- 3.Jez J. M., Penning T. M. The aldo-keto reductase (AKR) superfamily: an update. Chem. Biol. Interact. 2001;130–132:499–525. doi: 10.1016/s0009-2797(00)00295-7. [DOI] [PubMed] [Google Scholar]
- 4.Marschall H. U., Oppermann U. C., Svensson S., Nordling E., Persson B., Hoog J. O., Jornvall H. Human liver class I alcohol dehydrogenase gammagamma isozyme: the sole cytosolic 3beta-hydroxysteroid dehydrogenase of iso bile acids. Hepatology. 2000;31:990–996. doi: 10.1053/he.2000.5720. [DOI] [PubMed] [Google Scholar]
- 5.Oppermann U. C., Filling C., Jornvall H. Forms and functions of human SDR enzymes. Chem. Biol. Interact. 2001;130–132:699–705. doi: 10.1016/s0009-2797(00)00301-x. [DOI] [PubMed] [Google Scholar]
- 6.Adamski J., Jakob F. J. A guide to 17beta-hydroxysteroid dehydrogenases. Mol. Cell. Endocrinol. 2001;171:1–4. doi: 10.1016/s0303-7207(00)00383-x. [DOI] [PubMed] [Google Scholar]
- 7.Penning T. M., Burczynski M. E., Jez J. M., Lin H. K., Ma H., Moore M., Ratnam K., Palackal N. Structure–function aspects and inhibitor design of type 5 17beta-hydroxysteroid dehydrogenase (AKR1C3) Mol. Cell. Endocrinol. 2001;171:137–149. doi: 10.1016/s0303-7207(00)00426-3. [DOI] [PubMed] [Google Scholar]
- 8.Lukacik P., Kavanagh K. L., Oppermann U. Structure and function of human 17beta-hydroxysteroid dehydrogenases. Mol. Cell. Endocrinol. 2006;248:61–71. doi: 10.1016/j.mce.2005.12.007. [DOI] [PubMed] [Google Scholar]
- 9.Haeseleer F., Palczewski K. Short-chain dehydrogenases/reductases in retina. Methods Enzymol. 2000;316:372–383. doi: 10.1016/s0076-6879(00)16736-9. [DOI] [PubMed] [Google Scholar]
- 10.Wain H. M., Lush M. J., Ducluzeau F., Khodiyar V. K., Povey S. Genew: the Human Gene Nomenclature Database, 2004 updates. Nucleic Acids Res. 2004;32:D255–D257. doi: 10.1093/nar/gkh072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Otwinowski Z., Minor W. New York: Academic Press; 1997. Processing of X-ray Diffraction Data Collected in Oscillation Mode. [DOI] [PubMed] [Google Scholar]
- 12.Storoni L. C., McCoy A. J., Read R. J. Likelihood-enhanced fast rotation functions. Acta Crystallogr. D Biol. Crystallogr. 2004;60:432–438. doi: 10.1107/S0907444903028956. [DOI] [PubMed] [Google Scholar]
- 13.Brunger A. T., Adams P. D., Clore G. M., DeLano W. L., Gros P., Grosse-Kunstleve R. W., Jiang J.-S., Kuszewski J., Nilges M., Pannu N. S., et al. Crystallography & NMR System: a new software suite for macromolecular structure determination. Acta Crystallogr. D Biol. Crystallogr. 1998;54:905–921. doi: 10.1107/s0907444998003254. [DOI] [PubMed] [Google Scholar]
- 14.Murshudov G. N., Vagin A. A., Dodson E. J. Refinement of macromolecular structures by the maximum-likelihood method. Acta Crystallogr. D Biol. Crystallogr. 1997;53:240–255. doi: 10.1107/S0907444996012255. [DOI] [PubMed] [Google Scholar]
- 15.Terwilliger T. Maximum-likelihood density modification. Acta Crystallogr. D Biol. Crystallogr. 2000;56:965–972. doi: 10.1107/S0907444900005072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abagyan R. A., Totrov M. M. Contact area difference (CAD): a robust measure to evaluate accuracy of protein models. J. Mol. Biol. 1997;268:678–685. doi: 10.1006/jmbi.1997.0994. [DOI] [PubMed] [Google Scholar]
- 17.Abagyan R., Totrov M. High-throughput docking for lead generation. Curr. Opin. Chem. Biol. 2001;5:375–382. doi: 10.1016/s1367-5931(00)00217-9. [DOI] [PubMed] [Google Scholar]
- 18.Jornvall H., Persson B., Krook M., Atrian S., Gonzalez-Duarte R., Jeffery J., Ghosh D. Short-chain dehydrogenases/reductases (SDR) Biochemistry. 1995;34:6003–6013. doi: 10.1021/bi00018a001. [DOI] [PubMed] [Google Scholar]
- 19.Filling C., Berndt K. D., Benach J., Knapp S., Prozorovski T., Nordling E., Ladenstein R., Jornvall H., Oppermann U. Critical residues for structure and catalysis in short-chain dehydrogenases/reductases. J. Biol. Chem. 2002;277:25677–25684. doi: 10.1074/jbc.M202160200. [DOI] [PubMed] [Google Scholar]
- 20.Kallberg Y., Oppermann U., Jornvall H., Persson B. Short-chain dehydrogenases/reductases (SDRs) Eur. J. Biochem. 2002;269:4409–4417. doi: 10.1046/j.1432-1033.2002.03130.x. [DOI] [PubMed] [Google Scholar]
- 21.Breton R., Housset D., Mazza C., Fontecilla-Camps J. C. The structure of a complex of human 17beta-hydroxysteroid dehydrogenase with estradiol and NADP+ identifies two principal targets for the design of inhibitors. Structure. 1996;4:905–915. doi: 10.1016/s0969-2126(96)00098-6. [DOI] [PubMed] [Google Scholar]
- 22.Shafqat N., Elleby B., Svensson S., Shafqat J., Jornvall H., Abrahmsen L., Oppermann U. Comparative enzymology of 11 beta-hydroxysteroid dehydrogenase type 1 from glucocorticoid resistant (guinea pig) versus sensitive (human) species. J. Biol. Chem. 2003;278:2030–2035. doi: 10.1074/jbc.M210135200. [DOI] [PubMed] [Google Scholar]
- 23.Tomlinson J. W., Moore J. S., Clark P. M., Holder G., Shakespeare L., Stewart P. M. Weight loss increases 11beta-hydroxysteroid dehydrogenase type 1 expression in human adipose tissue. J. Clin. Endocrinol. Metab. 2004;89:2711–2716. doi: 10.1210/jc.2003-031376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Draper N., Echwald S. M., Lavery G. G., Walker E. A., Fraser R., Davies E., Sorensen T. I., Astrup A., Adamski J., Hewison M., et al. Association studies between microsatellite markers within the gene encoding human 11beta-hydroxysteroid dehydrogenase type 1 and body mass index, waist to hip ratio, and glucocorticoid metabolism. J. Clin. Endocrinol. Metab. 2002;87:4984–4990. doi: 10.1210/jc.2001-011375. [DOI] [PubMed] [Google Scholar]
- 25.Engeli S., Bohnke J., Feldpausch M., Gorzelniak K., Heintze U., Janke J., Luft F. C., Sharma A. M. Regulation of 11beta-HSD genes in human adipose tissue: influence of central obesity and weight loss. Obes. Res. 2004;12:9–17. doi: 10.1038/oby.2004.3. [DOI] [PubMed] [Google Scholar]
- 26.Seckl J. R., Morton N. M., Chapman K. E., Walker B. R. Glucocorticoids and 11beta-hydroxysteroid dehydrogenase in adipose tissue. Recent Prog. Horm. Res. 2004;59:359–393. doi: 10.1210/rp.59.1.359. [DOI] [PubMed] [Google Scholar]
- 27.Amery L., Mannaerts G. P., Subramani S., Van Veldhoven P. P., Fransen M. Identification of a novel human peroxisomal 2,4-dienoyl-CoA reductase related protein using the M13 phage protein VI phage display technology. Comb. Chem. High Throughput Screen. 2001;4:545–552. doi: 10.2174/1386207013330832. [DOI] [PubMed] [Google Scholar]
- 28.Das A. K., Uhler M. D., Hajra A. K. Molecular cloning and expression of mammalian peroxisomal trans-2-enoyl-coenzyme A reductase cDNAs. J. Biol. Chem. 2000;275:24333–24340. doi: 10.1074/jbc.M001168200. [DOI] [PubMed] [Google Scholar]
- 29.Helander H. M., Koivuranta K. T., Horelli-Kuitunen N., Palvimo J. J., Palotie A., Hiltunen J. K. Molecular cloning and characterization of the human mitochondrial 2,4-dienoyl-CoA reductase gene (DECR) Genomics. 1997;46:112–119. doi: 10.1006/geno.1997.5004. [DOI] [PubMed] [Google Scholar]
- 30.Koivuranta K. T., Hakkola E. H., Hiltunen J. K. Isolation and characterization of cDNA for human 120 kDa mitochondrial 2,4-dienoyl-coenzyme A reductase. Biochem. J. 1994;304:787–792. doi: 10.1042/bj3040787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mustonen M. V., Isomaa V. V., Vaskivuo T., Tapanainen J., Poutanen M. H., Stenback F., Vihko R. K., Vihko P. T. Human 17beta-hydroxysteroid dehydrogenase type 2 messenger ribonucleic acid expression and localization in term placenta and in endometrium during the menstrual cycle. J. Clin. Endocrinol. Metab. 1998;83:1319–1324. doi: 10.1210/jcem.83.4.4709. [DOI] [PubMed] [Google Scholar]
- 32.Miettinen M. M., Mustonen M. V., Poutanen M. H., Isomaa V. V., Vihko R. K. Human 17 beta-hydroxysteroid dehydrogenase type 1 and type 2 isoenzymes have opposite activities in cultured cells and characteristic cell- and tissue-specific expression. Biochem. J. 1996;314:839–845. doi: 10.1042/bj3140839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Steckelbroeck S., Watzka M., Lutjohann D., Makiola P., Nassen A., Hans V. H., Clusmann H., Reissinger A., Ludwig M., Siekmann L., et al. Characterization of the dehydroepiandrosterone (DHEA) metabolism via oxysterol 7alpha-hydroxylase and 17-ketosteroid reductase activity in the human brain. J. Neurochem. 2002;83:713–726. doi: 10.1046/j.1471-4159.2002.01187.x. [DOI] [PubMed] [Google Scholar]
- 34.Karishma K. K., Herbert J. Dehydroepiandrosterone (DHEA) stimulates neurogenesis in the hippocampus of the rat, promotes survival of newly formed neurons and prevents corticosterone-induced suppression. Eur. J. Neurosci. 2002;16:445–453. doi: 10.1046/j.1460-9568.2002.02099.x. [DOI] [PubMed] [Google Scholar]
- 35.Wang L., Andersson S., Warner M., Gustafsson J. A. Estrogen actions in the brain. Science STKE 2002. 2002:PE29. doi: 10.1126/stke.2002.138.pe29. [DOI] [PubMed] [Google Scholar]
- 36.Beyer C. Estrogen and the developing mammalian brain. Anat. Embryol. (Berlin) 1999;199:379–390. doi: 10.1007/s004290050236. [DOI] [PubMed] [Google Scholar]
- 37.Young E. A., Korszun A. The hypothalamic–pituitary–gonadal axis in mood disorders. Endocrinol. Metab. Clin. North Am. 2002;31:63–78. doi: 10.1016/s0889-8529(01)00002-0. [DOI] [PubMed] [Google Scholar]
- 38.Pinkerton J. V., Henderson V. W. Estrogen and cognition, with a focus on Alzheimer's disease. Semin. Reprod. Med. 2005;23:172–179. doi: 10.1055/s-2005-869485. [DOI] [PubMed] [Google Scholar]
- 39.Marin R., Guerra B., Alonso R., Ramirez C. M., Diaz M. Estrogen activates classical and alternative mechanisms to orchestrate neuroprotection. Curr. Neurovasc. Res. 2005;2:287–301. doi: 10.2174/156720205774322629. [DOI] [PubMed] [Google Scholar]
- 40.Wise P. M., Dubal D. B., Rau S. W., Brown C. M., Suzuki S. Are estrogens protective or risk factors in brain injury and neurodegeneration? Reevaluation after the Women's Health Initiative. Endocr. Rev. 2005;26:308–312. doi: 10.1210/er.2004-0014. [DOI] [PubMed] [Google Scholar]
- 41.Cooke B. M., Woolley C. S. Gonadal hormone modulation of dendrites in the mammalian CNS. J. Neurobiol. 2005;64:34–46. doi: 10.1002/neu.20143. [DOI] [PubMed] [Google Scholar]
- 42.Harlan R. E. Regulation of neuropeptide gene expression by steroid hormones. Mol. Neurobiol. 1988;2:183–200. doi: 10.1007/BF02935345. [DOI] [PubMed] [Google Scholar]
- 43.Osterlund M. K., Halldin C., Hurd Y. L. Effects of chronic 17beta-estradiol treatment on the serotonin 5-HT(1A) receptor mRNA and binding levels in the rat brain. Synapse. 2000;35:39–44. doi: 10.1002/(SICI)1098-2396(200001)35:1<39::AID-SYN5>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 44.Di Paolo T. Modulation of brain dopamine transmission by sex steroids. Rev. Neurosci. 1994;5:27–41. doi: 10.1515/revneuro.1994.5.1.27. [DOI] [PubMed] [Google Scholar]
- 45.Toran-Allerand C. D. Estrogen and the brain: beyond ER-alpha and ER-beta. Exp. Gerontol. 2004;39:1579–1586. doi: 10.1016/j.exger.2004.05.006. [DOI] [PubMed] [Google Scholar]
- 46.Toran-Allerand C. D., Guan X., MacLusky N. J., Horvath T. L., Diano S., Singh M., Connolly E. S., Jr, Nethrapalli I. S., Tinnikov A. A. ER-X: a novel, plasma membrane-associated, putative estrogen receptor that is regulated during development and after ischemic brain injury. J. Neurosci. 2002;22:8391–8401. doi: 10.1523/JNEUROSCI.22-19-08391.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]