Abstract
Objective:
The purpose of this study was to investigate heath disparities as a function of race and gender and the extent to which socioeconomic factors mediate disparities among participants with spinal cord injury.
Design:
Survey methodology. Cross-sectional data.
Setting:
A large Southeastern specialty hospital.
Participants:
There were 1,342 participants in the current analysis, all of whom were identified from patient records. There were 3 inclusion criteria: (a) traumatic SCI, (b) at least 18 years of age at the time of study, and (c) injury duration of more than 1 year.
Main outcome measures:
Six outcomes were measured, including 3 general outcomes (self-ratings, days impacted by poor health, days impacted by poor mental health) and 3 that reflect utilization of services (hospitalizations, days hospitalized, and nonroutine physician visits in the past 2 years).
Results:
Results of multivariate analysis of variance (MANOVA) indicated significant main effects for both race and gender. Follow-up tests identified racial disparities on 3 of the 6 outcomes, whereas gender disparities were observed for a single outcome. Years of education and household income mediated interrelationships between race and health (but not gender) as racial disparities disappeared after consideration of these factors.
Conclusions:
These findings suggest the need to work more diligently to promote better health outcomes among African Americans and to further investigate how socioeconomic factors and access to health care related to diminished health outcomes among African Americans with spinal cord injury.
Keywords: Spinal cord injuries, Health disparities, Outcomes, Race, African Americans
INTRODUCTION
While the nation's health has improved over the past several decades, major health conditions continue to differentially affect multiple racial and ethnic minority groups at all life stages. Despite the heightened attention and effort to improve health status and quality of care, women and minority populations in the United States continue to experience substantial disparities in health access and outcomes (1–3). A recent report by the Institute of Medicine, “Unequal Treatment; Confronting Racial and Ethnic Disparities in Health Care,” reviewed and summarized the literature pertaining to racial disparities in health care (4) by concluding that there is clear and convincing evidence that racial and ethnic disparities in health care are consistently present across a wide range of illnesses and health care services. According to the National Institutes of Health (NIH), “health disparities are the differences in incidence, prevalence, mortality, and burden of diseases and other adverse health conditions that exist among specific population groups in the United States” (5). Over the last 2 decades, research has focused on identifying and understanding how inequities in health care contribute to disparities and how these health disparities can be eliminated (6–8). As a result, the general population not only has increased longevity but also has an improved quality of life.
Previous studies have found that racial and ethnic minorities receive a lower quality of health care services and have higher morbidity and mortality rates than nonminorities (7). For example, African Americans are less likely to receive cardiac bypass surgery (9–11), hemodialysis and kidney transplant (12), appropriate diagnostic tests for cancer (13), appropriate cardiac medications (14), appropriate analgesic medications after bone fractures (15), and they are more likely to receive a lower quality of clinical services (9). Furthermore, these disparities have been documented even after controlling for variables such as insurance status, income, age, comorbid conditions, and clinical presentation. In a recent study analyzing mortality data in the United States, it was found that the mortality rates of white men and women are typically 29% and 24% lower than those of African American men and women (16). This same study found that, had the age-specific mortality rates been comparable during their study period, 886,202 deaths could have been prevented.
Inequities in education, income, and occupation, the primary determinants of socioeconomic status, account for some of the documented racial- and gender-related differences (17–19). Disparities in health and access to resources among minorities often are reflective of inequities in socioeconomic status. A 2004 study investigating health disparities and cervical cancer found that 28% of the Medicaid-insured women in their sample were African American (compared with 10% for white women) (20). This same study found cervical cancer incidence to be significantly higher among low-income women, most of whom were insured by Medicaid. Thus, African American women had a higher incidence of cervical cancer and one factor contributing to this increased incidence was the type of insurance they carried, which likely affected access to health care resources. Along those same lines, in examining socioeconomic differences in smoking, it was found that the prevalence of current smoking was greatest in persons with working-class jobs, low education, and low income; it was found that this pattern also held across the majority of the racial groups studied (21). These data suggest that studies investigating racial disparities must examine the impact of socioeconomic factors on the presence of health disparities.
The significance of health disparities becomes even more critical when examining outcomes of persons with disabilities. In examining the disabled population, specifically individuals with spinal cord injury (SCI), the rate of disability among African Americans is disproportionately high (22). The Centers for Disease Control (CDC) National Center for Health Statistics (NCHS) has reported that African Americans are at higher risk than whites for SCI (23). This increased risk can be attributed to socioeconomic factors, lifestyle behaviors, social environment, and access to clinical preventive services, all of which are associated with health disparities (17,24).
The National Spinal Cord Injury Statistical Center (NSCISC) estimated that 243,000 persons in the United States live with a disability related to SCI, and approximately 11,000 new cases occur each year (25). More than half of the people who sustain SCI are 16 to 30 years old, and 81.2% of persons in the National SCI Statistical Center Database are male. The epidemiology of SCI has resulted in certain groups being notably underrepresented. Research has utilized the more predominant population (ie, young white men), resulting in limited investigation on gender and race-ethnicity health outcomes after SCI (26). However, over the years, studies have gradually increased their focus on gender and racial/ethnic disparities.
In investigating the impact of race and ethnicity in persons with SCI, it was found that, overall, women and racial/ethnic minorities have lower satisfaction with finances and less education (27,28). These factors are associated with health outcomes and quality of life in the SCI population. Lower socioeconomic status also influences emotional and psychosocial outcomes following SCI (29–31). Therefore, it is important to investigate the influence of socioeconomic variables on gender and racial differences in SCI outcomes.
The most common psychological disorder among people with SCI appears to be depression (31–34). Contrary to research stating that women adjust better to SCI, other studies have found that women were at considerably more risk for serious depression than men (35–38). However, the prevalence of depressive symptomatology and stress in women may be associated with a lower degree of mobility within the home and community and severe chronic pain (39).
Outcomes following SCI also vary depending on racial/ethnic background. One study found that women with SCI of different ethnic groups tend to differ by functional levels, health status, and disability (40). In a study investigating psychological outcomes following SCI by racial background, Kemp and associates found that Latino participants reported greater depressive symptomatology than either African American or white participants (41). In a similar study, African American women were at a substantially higher risk for depressive symptomatology than their white counterparts (42). Low education and income largely account for this elevated risk. Also, compared with white men, minority men were more likely to report scores indicative of probable major depression. Minority women were more likely to report clinically significant symptomatology and probable major depression. Likewise, minority women with SCI appear to experience greater emotional distress than minority men and white men and women with SCI (43).
In summary, the relationship among race/ethnicity, gender, and socioeconomic status shape a person's health. Furthermore, preliminary evidence suggests that, whereas gender and racial differences in functional and emotional outcomes post-SCI may exist, more investigation is required to further elucidate these differences and the factors that contribute to them. It is critical to understand differences in health care to eliminate health disparities. Negative health outcomes of women and racial/ethnic minorities reveal the existence of insufficient interventions and access to care. Continued research efforts to identify health inequities are likely to address gaps in both basic and intervention research on the interaction of minority groups with health care systems.
Purpose
The purpose of this study was to identify disparities in health outcomes after SCI as a function of gender and race (white and African American) and to explicitly test a model that hypothesizes that racial disparities are related to socioeconomic factors.
Hypotheses
African American participants will report poorer overall health compared with white participants.
Compared with men, women will report a greater number of days adversely impacted by poor mental health.
Socioeconomic factors, as defined by years of education and household income, will mediate the relationship between race and health outcomes.
No such mediational relationship will be observed for gender.
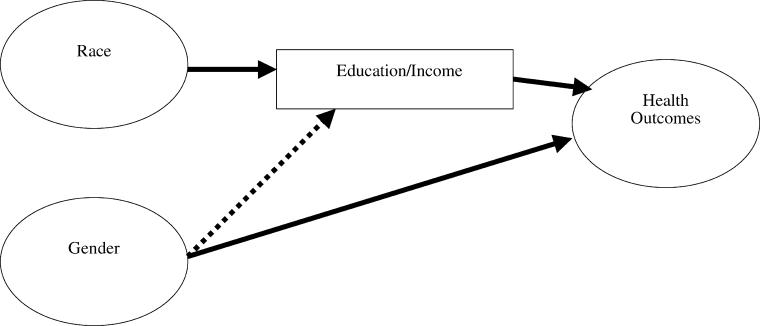
The hypotheses are taken from related findings in the SCI literature, but are extended using a mediational model based on socioeconomic status. The primary findings suggest that socioeconomic factors are more important to race than to gender (a hypothesis tested in this study). Figure 1 summarizes this mediational model. When using a mediational model, the relationships between independent and dependent variables are present in the absence of additional variables (ie, mediators), but the relationships between independent and dependent variables disappear or are at least substantially reduced when accounting for mediating variables (44). According to the model, race differences in health are mediated by socioeconomic factors, whereas the relationship between gender and health is direct.
Figure 1. A mediational model based on socioeconomic factors.
METHODS
Participants
Participants were identified from outpatient records of a large Southeastern rehabilitation hospital and were identified from 3 types of hospital records that were searched for prospective participants: (a) the model SCI systems (MSCIS) database—those in the catchment area, (b) the MSCIS registry—outside the catchment area, and (c) outpatient records. There were 3 inclusion criteria: (a) traumatic SCI, (b) at least 18 years of age at the time of study, and (c) had been injured for at least 1 year. There were 1,342 participants and a 72.3% response rate. Of these, 75% were white and 74% were men. A breakdown by gender and race indicates 56% were white men (n = 755), 21% were white women (n = 280), 18% were African American men (n = 238), and 5% were African American women (n = 69). The limited number of minorities other than African American precluded their use in the comparative analyses.
Data Collection Procedures
Following approval from the Institutional Review Board, prospective participants were sent cover letters to explain the study and as an alert that materials were forthcoming. Complete packets of materials were sent to participants about 4 weeks later, with a second set of materials sent to all nonrespondents, followed by an additional phone call. A third mailing was implemented to all individuals who either agreed to participate during the follow-up phone call or who could not be reached by phone at that time. In order to bolster response rates, participants were offered a $20 stipend to complete the study materials and were made eligible for drawings totaling another $1,500.
Measures
Two sets of outcome measures were used: general health indicators from the Behavioral Risk Factor Surveillance System (BRFSS) and recent medical treatments. Predictive factors in the mediational analyses included socioeconomic indicators and social support.
The BRFSS is a standardized instrument that has been used with more than 100,000 individuals by the CDC. It is used to monitor relevant basic health behaviors within the general population and in specific regions of the country (45–49). At the time of prospective data collection, this instrument consisted of 3 parts: (a) a standardized core section that consists of 78 questions divided into 10 sections including health care access, exercise, tobacco use, and women's health; (b) optional modules with questions about diabetes, sexual behavior, injury control, and alcohol use; and (c) an added group of questions of special interest to the state or agency utilizing the survey.
The BRFSS contains 3 general health-related items that were used in this study: self-rated health, poor physical health days in past month, and poor mental health days in the past month. The CDC has used each of the items extensively such that existing data are available for normative purposes.
Three items measured recent medical history: the number of nonroutine physician visits, number of hospitalizations, and days hospitalized. Each of these items has been used in multiple previous studies. The mediational variables include years of education and household income, which was grouped according to the categories used in the BRFSS (less than $15,000, $15,000 to $24,999 … $75,000 or more).
Analyses
Descriptive statistics were generated in order to describe the study sample. The multivariate analysis of variance (MANOVA) was used to compare all programs across all outcome variables as a function of race and gender, as well as the interaction between race and gender. The Wilks statistic was used to determine significance of each effect. Follow-up univariate ANOVAs were generated for each significant effect (only main effects were significant).
Regression was used to test mediation. Three conditions must be present for mediation to occur: (1) the predictor variable must be correlated with the outcome variable, (2) the mediational variable(s) must be correlated with the predictor and outcome variable, and (3) the correlation between the predictor and outcome variables must disappear when considering the mediators (partial mediation would occur if the correlation between the predictor and outcome variables declines but is still statistically significant). Mediation was tested using multiple linear regression and logistic regression. Linear regression was used for each of the 6 outcome variables, whereas logistic regression was used exclusively in a secondary analysis in which hospitalizations were dichotomized (0, 1, or more). In each mediational analysis, the primary predictive factors of race and gender were entered into the equation in order to determine their statistical significance and their contribution to the squared multiple correlation (linear regression) and the odds ratio (logistic regression). A second regression analysis was then conducted with the mediating variables inserted into the equation prior to the primary variables to determine whether the primary variables continue to explain variation above and beyond that of the mediators. If the primary variables were no longer significant after inclusion of the mediators, then this was evidence for mediation.
RESULTS
Descriptive
The average age of the participants was 41.6 years (SD = 13.8; range of 18–85 years) at the time of the study and 31.8 years at injury onset (SD = 14.0; range of 2–82 years). An average of 9.7 years had passed between the time of injury and the time of the study (SD = 6.8; range of 1–50 years). Cervical injuries occurred in 55% of the participants. Participants classified their injuries into 1 of 4 groups based on completeness of injury: (a) no sensation or movement below injury level (29.4%), (b) sensation, but no movement below injury level (28.5%), (c) movement below injury level but not sufficient to aid in ambulation (20.8%), and (d) useful function below level of injury that allows for some ambulation (21.5%). The most common etiology of injury was motor vehicle crashes (51%), followed by falls (17%), acts of violence (13%), sporting incidents (12%), and other causes (7%). The average number of years of education was 13.1 (SD = 2.8; range of 5–20 years). The results revealed that 42% of participants reported an annual income of less than $15,000, followed by 17% reporting incomes between $15,000 and $24,999, 22% between $25,000 and $49,999, 9% between $50,000 and $74,999, and 9% $75,000 or more.
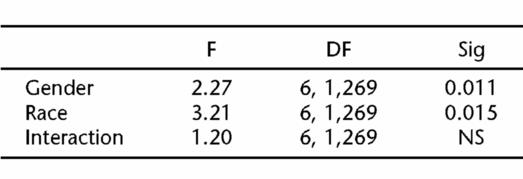
MANOVA. Missing data from outcome measures reduced the sample to 1,278 for the MANOVA (missing data on any variable eliminates that case on the MANOVA). Significant main effects were observed for both race, F(6, 1269) = 3.21, P <0.001; and gender, F(6, 1269) = 2.27, P <0.001 (Table 1). The interaction between race and gender was not significant, F(6, 1269) = 1.20, NS. Because both main effects were statistically significant, follow-up univariate tests for main effects were conducted for each of the outcome variables.
Table 1.
Mulitvariate Analysis of Variance (MANOVA) of Health Outcomes as a Function of Gender and Race
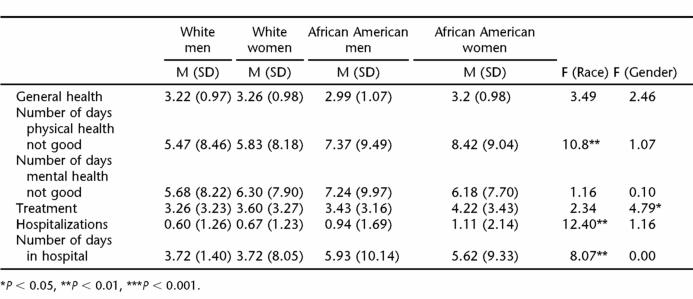
There were significant race differences on 3 of the 6 outcome variables (Table 2): days in poor health in the past month, number of hospitalizations, and days hospitalized. African American participants reported more days in poor health (7.9 vs 5.7 d), more hospitalizations in the past year (1.03 vs 0.064) and days hospitalized (5.8 vs 3.9 d). The only significant gender difference was for number of nonroutine physician visits, where women reported significantly more physician visits than men (3.3 vs 3.9). (The maximum number of physician visits and hospitalizations recorded was 10 and days hospitalized was 30, so means underestimate true averages, but are less affected by extreme individual outliers.)
Table 2.
Follow-Up Univariate Analysis of Variance of the Relationship of Race and Gender with 6 Health Outcomes
Mediation
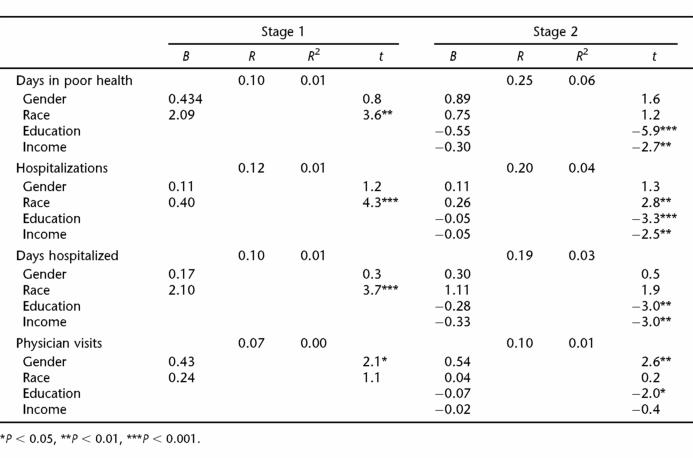
Mediational analyses were conducted for each outcome variable that was significantly related to either race or gender during the MANOVA. Therefore, the following outcome variables were used in the linear regression analyses: days in poor health, hospitalizations, days hospitalized, and nonroutine physician visits. Although statistically significant, neither race nor gender accounted for substantial variation in any of the outcome variables, and the mediators accounted for greater variation in all cases.
There was support for mediation for race, with one exception, but not for gender (Table 3). On the only outcome for which gender differences were observed, number of nonroutine physician visits, gender remains statistically significant after entry of the mediating variables.
Table 3.
Multiple Correlations, Squared Multiple Correlations, and Significance of Gender and Race with Health Outcomes Prior to the Addition of Socioeconomic Predictors (Stage 1) and After the Addition of Socioeconomic Predictors (Stage 2)
Race was significantly associated with days in poor physical health but accounted for only 1% of the variation prior to inclusion of the mediators. When entered into the equation first, the mediators accounted for 6% of the variation, with race no longer significantly adding to the equation. Similar findings were observed for days hospitalized, as race was no longer statistically significant after accounting for the mediators. However, for number of hospitalizations, race remained significant after inclusion of the mediators (this is a highly skewed variable and therefore dichotomized in a subsequent analysis).
Because the number of hospitalizations and days hospitalized are highly skewed variables, we dichotomized hospitalizations (0, 1, or more) and used logistic regression to identify the odds of being hospitalized as a function of gender, race, and the mediating variables. Prior to entering the mediating variables, African Americans had 1.49 greater odds of being hospitalized in the previous year than did whites. In the second analysis, the 2 mediators were entered into the equation prior to race, both of which were associated with a decreased likelihood of hospitalization. The odds ratio of hospitalization among African Americans dropped to 1.17 and was no longer statistically significant.
DISCUSSION
There were mixed results for the study hypotheses. First, racial disparities were observed on 3 of the 6 health outcomes, with African Americans reporting a greater number of poor health days, more hospitalizations, and a greater number of days hospitalized (generally supporting hypothesis 1). The magnitude of these disparities was small from the standpoint of variation explained using regression, but the differences were clinically significant. For instance, African Americans averaged more than 2 poor health days in the last month and nearly 2 days more per year in the hospital.
Gender was largely unrelated to health outcomes, although women did report a greater number of nonroutine physician visits. This does not necessarily indicate differences in health per se, but could also reflect differences in likelihood of seeking medical advice. We anticipated women would report a greater number of poor emotional health days based on previous findings of a greater incidence of depressive symptoms, but this was not the case. Therefore, hypothesis 2 was not supported.
The mediational hypotheses (hypotheses 3 and 4) were supported with one minor exception. On 2 of 3 health outcomes in which racial disparities were observed, education and household income mediated these relationships such that race was no longer associated with these outcomes after consideration of the mediating factors. Although socioeconomic factors did not mediate the relationship for number of hospitalizations, this outcome was highly skewed, with most participants reporting no hospitalizations, and this may have accounted for the finding. When we dichotomized hospitalizations into those who were and were not hospitalized, the socioeconomic factors mediated the relationship between race and hospitalization. In fact, the odds of a hospitalization for African Americans decreased from 1.49 to a nonsignificant 1.17, which clearly is important. As hypothesized, no mediation was observed for gender, suggesting that other factors led to these differences between men and women in physician visits.
Implications
One of the primary goals of the federally funded national Healthy People 2010 initiative is to eliminate health disparities and improve access to quality health services (50). In order to eliminate the documented racial disparity in post-SCI outcomes, it is critical to determine if the difference is due to differential socioeconomic status and how this affects access to care. Thus, this study has numerous public health implications, as health disparities due to race and socioeconomic status are one of the biggest problems facing our nation today. When disability is factored into that equation, the implications multiply. First, with African Americans post-SCI reporting more days of poor health and more time in the hospital, it is clear that more attention needs to be paid to this population. As studies have reported, African Americans have a significantly higher mortality rate than do whites, and this remains true for individuals with SCI (16,51–53). Second, socioeconomic status appears to have a significant impact on health disparities and needs to be addressed, especially for individuals with SCI. There are a number of educational and vocational challenges that can arise after SCI, including a difficulty in returning to school and work, an increased time period before being able to return to employment, as well as the inability to return to the same field of employment due to physical implications of SCI (49,51,54–61). When all of these challenges are taken together, conquering socioeconomic disparities seems an almost insurmountable task. Furthermore, socioeconomic status, directly related to the type of insurance a patient has, is a primary factor influencing health disparities. According to a recent report, “insurance more than any demographic or economic factor, determines the timeliness and quality of health care, if it is received at all” (62). For individuals with SCI, it would be extremely beneficial to address some of these socioeconomic factors during rehabilitation in order to maximize the chance for successful outcomes and to work toward the reduction of disparities in health outcomes.
Limitations
There are several limitations in this study. First, all data are self-reported and there is always the prospect of some degree of bias in retrospective recall. We attempted to limit this concern by using standardized ratings; such data are overall ratings of health and bad health days within the last month. We also used memorable outcomes, such as hospitalizations, over time-limited periods (1 year). Second, although this study focuses on disparities among minority participants, African Americans were the sole minority group utilized. Although other studies have been conducted with broader representation, most of the studies are limited to analysis of the model SCI systems data set, which lacks the breadth of outcome variables, or more focused studies that have relatively small sample sizes. Third, although the mediational design helps us understand factors that might help for the observed racial disparities, the cross-sectional data preclude determination of causality. This is a common limitation because of the rare use of longitudinal designs. Fourth, because we did not find complete mediation across all outcome variables, factors beyond socioeconomic status must be considered in studies of racial disparities. Finally, important covariates that also mediate health disparities, such as type of insurance, were not examined in this study. It is possible that African Americans have less severe injuries and that the health disparities would have been magnified if this variable were also considered. Investigation of broader outcomes with a larger number of covariates over an extended period of time may shed further light on these issues.
Future Research
In looking toward the future, it is clear that further research needs to focus on gender and racial disparities for individuals with SCI. While this is an important first step in the identification of gender and racial disparities post-SCI, further studies are required to verify the presence or absence of these disparities and to provide insight into the factors that may be contributing to any observed disparities. A multitude of variables may contribute to the documented racial disparities in access to health care services and to resultant health disparities, and it is likely that many of these factors operate simultaneously. One of the first conceptual frameworks developed to examine access to health care identified 3 major categories of factors that influence access: health policy, characteristics of health delivery systems, and characteristics of the population (63). Characteristics of the population are further refined into 3 components: predisposing factors, enabling factors, and need factors. Each of these categories and components needs to be addressed as fully as possible in future studies.
To further clarify these results, it is important to extend this study to a larger sample with other minority groups and to identify a larger range of outcomes. Second, it is important to identify and collect other variables that might influence racial and gender disparities in health outcomes, such as type of insurance, geographic location and the distribution of health resources near the patient's home, the presence of comorbidities, and other factors. These data and data from future related studies could be utilized to influence health policy and reduce disparities in access to health care and in health outcomes post-SCI.
Footnotes
This research was supported by Model Spinal Cord Injury Systems (MSCIS) grants from the National Institute for Disability and Rehabilitation Research (NIDRR) of the Office of Special Education and Rehabilitative Services (OSERS) of the Department of Education (#H133N00023 and #H133N000005).
REFERENCES
- Dougherty RH. Reducing disparity in behavioral health services: a report from the American College of Mental Health Administration. Adm Policy Ment Health. 2004;3:253–263. doi: 10.1023/b:apih.0000018833.22506.fc. [DOI] [PubMed] [Google Scholar]
- Cox R. Global health disparities: crisis in the diaspora. J Natl Med Assoc. 2004;4:546–549. [PMC free article] [PubMed] [Google Scholar]
- Alliance for Health Reform. Closing the gap: racial and ethnic disparities in healthcare. J Natl Med Assoc. 2004;96:436–440. [PMC free article] [PubMed] [Google Scholar]
- Smedley B, Stith A, Nelson A, editors. Unequal Treatment: Confronting Racial And Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2002. [PubMed] [Google Scholar]
- Department of Health and Human Services. Health Disparities Among Minorities and Underserved Women. 2004. Available at: http://grants.nih.gov/grants/guide/pa-files/PA-04-153.html. Accessed January 16, 2006.
- Dikmen S, Reitan RM. Psychological deficits and recovery of functions after head injury. Trans Am Neurol Assoc. 1976;101:72–77. [PubMed] [Google Scholar]
- US Dept of Health and Human Services. Healthy People 2010: Understanding and Improving Health. 2nd ed. 2000. 8. Available at: http://www.healthypeople.gov/document/tablesofcontents.htm. Accessed October 14, 2005.
- Pamuk E, Wagner D, Molla M. Achieving national health objectives: the impact on life expectancy and on healthy life expectancy. Am J Public Health. 2004;94:378–383. doi: 10.2105/ajph.94.3.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayanian JZ, Weissman JS, Chasan-Taber S, Epstein AM. Quality of care by race and gender for congestive heart failure and pneumonia. Med Care. 1999;37:1260–1269. doi: 10.1097/00005650-199912000-00009. [DOI] [PubMed] [Google Scholar]
- Hannan EL, Van Ryn M, Burke J et al. Access to coronary artery bypass surgery by race/ethnicity and gender among patients who are appropriate for surgery. Med Care. 1999;37:68–77. doi: 10.1097/00005650-199901000-00010. [DOI] [PubMed] [Google Scholar]
- Petersen LA, Wright SM, Peterson ED, Daley ED. Impact of race on cardiac care and outcomes in veterans with acute myocardial infarction. Med Care. 2002;40:I86–I96. doi: 10.1097/00005650-200201001-00010. suppl. [DOI] [PubMed] [Google Scholar]
- Epstein AM, Ayanian JZ, Keogh JH et al. Racial disparities in access to renal transplantation. New Engl J Med. 2000;343:1537–1544. doi: 10.1056/NEJM200011233432106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMahon LF, Wolfe RA, Huang S et al. Racial and gender variation in use of diagnostic colonic procedures in the Michigan Medicare population. Med Care. 1999;37:712–717. doi: 10.1097/00005650-199907000-00011. [DOI] [PubMed] [Google Scholar]
- Herholz H, Goff DC, Ramsey DJ et al. Women and Mexican Americans receive fewer cardiovascular drugs following myocardial infarction than men and non-Hispanic-Whites: The Corpus Christi Heart Project, 1988–1990. J Clin Epidemiol. 1996;49:279–287. doi: 10.1016/0895-4356(95)00572-2. [DOI] [PubMed] [Google Scholar]
- Todd KH, Samaroo N, Hoffman JR. Ethnicity as a risk factor for inadequate emergency department analgesia. JAMA. 1993;269:1537–1539. [PubMed] [Google Scholar]
- Woolf SH, Johnson RE, Fryer GE, Rust G, Satcher D. The health impact of resolving racial disparities: an analysis of US mortality data. Am J Public Health. 2004;94:2078–2081. doi: 10.2105/ajph.94.12.2078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiscella K, Willams D. Health disparities based on socioeconomic inequities: implications for urban health care. Acad Med. 2004;79:1139–1147. doi: 10.1097/00001888-200412000-00004. [DOI] [PubMed] [Google Scholar]
- Starfield B. Promoting equity in health through research and understanding. Developing World Bioeth. 2004;4:76–95. doi: 10.1111/j.1471-8731.2004.00068.x. [DOI] [PubMed] [Google Scholar]
- Roy J. Socioeconomic status and health: a neurobiological perspective. Med Hypotheses. 2004;62:222–227. doi: 10.1016/S0306-9877(03)00315-3. [DOI] [PubMed] [Google Scholar]
- Bradley CJ, Given CW, Roberts C. Health care disparities and cervical cancer. Am J Public Health. 2004;94:2098–2103. doi: 10.2105/ajph.94.12.2098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbeau EM, Krieger N, Soobader M. Working class matters: socioeconomic disadvantage, race/ethnicity, gender and smoking in NHIS 2000. Am J Public Health. 2004;94:269–278. doi: 10.2105/ajph.94.2.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NSCISC. Facts and Figures at a Glance. Birmingham, AL: University of Alabama; 2003. [Google Scholar]
- Statistics CNCfH. National Mortality Data, 1997. 1998.
- Farmer M, Ferraro K. Are racial disparities in health conditional on socioeconomic status? Soc Sci Med. 2005;60:191–204. doi: 10.1016/j.socscimed.2004.04.026. [DOI] [PubMed] [Google Scholar]
- NSCIS. Annual Report for the Model Spinal Cord Injury Systems. Birmingham, AL: University of Alabama; 2000. [Google Scholar]
- Stuart G, Laraia M. Principles and Practices of Psychiatric Nursing. 7th ed. St. Louis, MO: Mosby; 2001. [Google Scholar]
- Krause JS. Subjective well-being after spinal cord injury: relationship to gender, race-ethnicity, and chronologic age. Rehabil Psychol. 1998;43:282–296. [Google Scholar]
- Krause JS. Employment after spinal cord injury: transition and life adjustment. Rehabil Couns Bull. 1996;39:244–255. [Google Scholar]
- Elliott TR, Frank RG. Depression following spinal cord injury. Arch Phys Med Rehabil. 1996;77:816–823. doi: 10.1016/s0003-9993(96)90263-4. [DOI] [PubMed] [Google Scholar]
- Frank R, Chaney J, Clay D et al. Dysphoria: a major symptom factor in persons with disability or chronic illness. Psychiatry Res. 1992;43:231–241. doi: 10.1016/0165-1781(92)90056-9. [DOI] [PubMed] [Google Scholar]
- Fuhrer MJ, Rintala DH, Hart KA, Clearman R, Young ME. Depressive symptomatology in persons with spinal cord injury who reside in the community. Arch Phys Med Rehabil. 1993;74:255–260. [PubMed] [Google Scholar]
- Turner R, Wood D. Depression and disability: the stress process in a chronological strained population. Res Community Men Health. 1985;5:77–109. [Google Scholar]
- Dijkers M. Correlates of life satisfaction among persons with spinal cord injury. Arch Phys Med Rehabil. 1999;80:867–876. doi: 10.1016/s0003-9993(99)90076-x. [DOI] [PubMed] [Google Scholar]
- Woodrich F, Patterson JB. Variables related to acceptance of disability in persons with spinal cord injuries. J Rehabil. 1983;49:26–30. [PubMed] [Google Scholar]
- Fuhrer M, Rintala D, Hart KA, Clearman R, Young M. Relationship to life satisfaction to impairment, disability, and handicap among persons with spinal cord injury living in a community. Arch Phys Med Rehabil. 1992;73:552–557. [PubMed] [Google Scholar]
- Gerhart KA, Weitzenkamp D, Kennedy P, Glass CA, Charlifue SW. Correlates of stress in long-term spinal cord injury. Spinal Cord. 1999;37:183–190. doi: 10.1038/sj.sc.3100804. [DOI] [PubMed] [Google Scholar]
- Cairns D, Adkins R, Scott M. Pain and depression in acute traumatic spinal cord injury: origins of chronic problematic pain? Arch Phys Med Rehabil. 1996;77:329–335. doi: 10.1016/s0003-9993(96)90079-9. [DOI] [PubMed] [Google Scholar]
- Demirel G, Yllmaz H, Gencosmanoglu B, Kesiktas N. Pain following spinal cord injury. Spinal Cord. 1998;36:25–28. doi: 10.1038/sj.sc.3100523. [DOI] [PubMed] [Google Scholar]
- Andersen E, Brownson R. Disability and health status: ethnic differences among women in the United States. J Epidemiol Community Health. 2000;54:200–206. doi: 10.1136/jech.54.3.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause JS, Kemp BJ, Coker JL. Depression after spinal cord injury: relationship with gender, race/ethnicity, aging and socioeconomic indicators. Arch Phys Med Rehabil. 2000;81:1099–1109. doi: 10.1053/apmr.2000.7167. [DOI] [PubMed] [Google Scholar]
- Kemp BJ, Krause JS, Adkins RA. Depressive symptomatology among African-American, Latino and Caucasian participants with spinal cord injury. Rehabil Psychol. 1999;44:235–247. [Google Scholar]
- Krause JS, Anson CA. Adjustment after spinal cord injury: relationship to gender and race. Rehabil Psychol. 1997;42:31–46. [Google Scholar]
- Powell-Griner E, Anderson JE, Murphy W. State-and sex-specific prevalence of selected characteristics—behavioral risk factor surveillance system, 1994 and 1995. MMWR CDC Surveill Summ. 1997;46:1–31. [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Krause JS. Factors associated with risk for subsequent injuries after the onset of traumatic spinal cord injury. Arch Phys Med Rehabil. 2004;85(9):1503–1508. doi: 10.1016/j.apmr.2004.01.017. [DOI] [PubMed] [Google Scholar]
- Krause JS, Broderick LE. Outcomes after spinal cord injury: comparison as a function of gender and race ethnicity. Arch Phys Med Rehabil. 2004;85:355–361. doi: 10.1016/s0003-9993(03)00615-4. [DOI] [PubMed] [Google Scholar]
- Krause JS, Broderick LE. Community outcomes after spinal cord injury: comparisons as a function of gender and race/ethnicity. Arch Phys Med Rehabil. 2004;85:355–362. doi: 10.1016/s0003-9993(03)00615-4. [DOI] [PubMed] [Google Scholar]
- Krause JS, Vines CL, Farley TL, Sniezek J, Coker J. An exploratory study of pressure ulcers after spinal cord injury: relationship to protective behaviors and risk factors. Arch Phys Med Rehabil. 2001;82:107–113. doi: 10.1053/apmr.2001.18050. [DOI] [PubMed] [Google Scholar]
- Krause JS. Aging and self-reported barriers to employment after spinal cord injury. Top Spinal Cord Inj Rehabil. 2001;6:101–115. [Google Scholar]
- Department of Health and Human Services. Healthy people 2002. Available at: http://www.healthypeople.gov/About/goals.htm. Accessed October 31, 2003.
- Krause JS, DeVivo MJ, Jackson AB. Health status, community integration, and economic risk factors for mortality after spinal cord injury. Arch Phys Med Rehabil. 2004;85:1764–1773. doi: 10.1016/j.apmr.2004.06.062. [DOI] [PubMed] [Google Scholar]
- Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Painting a truer picture of US socioeconomic and racial/ethnic health inequalities: the public health disparities geocoding project. Am J Public Health. 2005;95:312–323. doi: 10.2105/AJPH.2003.032482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian SV, Chen JT, Rehkopf DH, Waterman PD, Kreiger N. Racial disparities in context: a multilevel analysis of neighborhood variations in poverty and excess mortality among black populations in Massachusetts. Am J Public Health. 2005;95:260–265. doi: 10.2105/AJPH.2003.034132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wineman N. Adaptation to multiple sclerosis: the role of social support, functional disability, and perceived uncertainty. Nurs Res. 1990;39:294–299. [PubMed] [Google Scholar]
- Rohe DE, Krause J. Vocational interests of middle-aged men with traumatic spinal cord injury. Rehabil Psychol. 1999;44:160–175. [Google Scholar]
- Rohe DE, Krause J. Stability of interests after severe physical disability: an 11-year longitudinal study. J Vocat Behav. 1998;52:45–58. [Google Scholar]
- Rohe DE, Athelstan GT. Change in vocational interests after spinal cord injury. Rehabil Psychol. 1985;30:131–143. [Google Scholar]
- Krause JS, Broderick LE. Outcomes after spinal cord injury: comparisons as a function of gender and race and ethnicity. Arch Phys Med Rehabil. 2004;85:355–361. doi: 10.1016/s0003-9993(03)00615-4. [DOI] [PubMed] [Google Scholar]
- Krause JS. Return to employment after spinal cord injury. Arch Phys Med Rehabil. 2003;84:1282–1289. doi: 10.1016/s0003-9993(03)00265-x. [DOI] [PubMed] [Google Scholar]
- Krause JS, Broderick L. Outcomes after spinal cord injury: comparisons as a function of gender and race and ethnicity. Arch Phys Med Rehabil. 2004;85:355–362. doi: 10.1016/s0003-9993(03)00615-4. [DOI] [PubMed] [Google Scholar]
- Krause JS, Kewman D, DeVivo MJ et al. Employment after spinal cord injury: an analysis of cases from the Model Spinal Cord Injury Systems. Arch Phys Med Rehabil. 1999;80:1492–1500. doi: 10.1016/s0003-9993(99)90263-0. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Coverage Matters: Insurance and Health Care. Washington, DC: National Academy Press; 2001. [Google Scholar]
- Aday L, Andersen R. A framework for the study of access to medical care. Health Serv Res. 1974;9:208–220. [PMC free article] [PubMed] [Google Scholar]