Abstract
Background/Objective:
To determine the degree and duration of pain relief provided by specific pain treatments used by individuals with spinal cord injury (SCI) who have chronic pain.
Design:
Postal survey.
Setting:
Community.
Participants:
Participants were 117 individuals who had traumatic SCI, were 18 years of age or older, and reported a chronic pain problem.
Main Outcome Measures:
Questions assessing current or past use of 26 different pain treatments, the amount of relief each treatment provided, and the length of time that any pain relief usually lasts.
Results:
The medications tried most often were nonsteroidal anti-inflammatory drugs (tried by 71%) and acetaminophen (tried by 70%); these medications were still being used by more than one half of the patients who had tried them. Opioids produced the greatest degree of pain relief on average (mean, 6.27 ± 3.05 [SD] on a 0–10 scale, with 0 = no relief and 10 = complete relief) but were unlikely to be continued by those who tried them. Although 38% of respondents with pain had tried gabapentin, only 17% were still using it, and average pain relief was only moderate (mean, 3.32 ± 3.03 on the 0–10 relief scale). Seventy-three percent of the respondents had tried at least 1 of 7 alternative pain treatments, and the most frequently tried were massage, marijuana, and acupuncture. The most relief was provided by massage (mean, 6.05 ± 2.47] on the 0–10 relief scale) and marijuana (mean, 6.62 ± 2.54 on the 0–10 relief scale). The relief from the various treatments, including most medications, tended to last only minutes or hours; however, pain relief from alternative treatments such as massage, acupuncture, and hypnosis was reported to last for days in 25% to 33% of those who tried these treatments.
Conclusions:
Many patients are not finding adequate pain relief from commonly prescribed medications. Alternative therapies should be considered as additional treatment options in this population.
Keywords: Spinal cord injuries, Pain, Chronic, Neuropathic, Musculoskeletal, Analgesia, Gabapentin, Massage, Acupuncture, Alternative therapy
INTRODUCTION
Chronic pain remains a significant problem for many with spinal cord injury (SCI). Recent data from the national Model Spinal Cord Injury Systems indicate a pain prevalence ranging from 81% at 1 year after injury to 82.7% at 25 years (1). Studies have shown that persons with SCI commonly develop musculoskeletal pain problems and/or neuropathic pain at and/or below the level of the lesion, both of which can be very refractory to treatment (2–5). Attempts to treat musculoskeletal pain problems usually focus on the alleviation of underlying pathology or aggravating conditions such as poor posture or overuse. In the person with complete SCI, musculoskeletal pain is only appreciated above the level of the lesion. However, individuals with an incomplete SCI may complain of musculoskeletal pain problems that occur below the level of the injury.
Neuropathic pain, which may develop at or below the level of the lesion, is even more refractory to treatment than musculoskeletal pain. Clinically, neuropathic pain may be subdivided into 4 types: (a) SCI pain, which occurs below the level of the injury; (b) transition zone pain, which is usually bilateral and at the level of injury; (c) radicular pain, which is usually unilateral; and (d) visceral pain (6). The most common type of neuropathic pain is that below the level of injury (7–16).
The diagnosis of neuropathic pain attributed to the spinal cord lesion itself is essentially a diagnosis of exclusion. The diagnosing clinician should seek any potentially treatable causes of pain such as a post-traumatic syrinx, a Charcot arthropathy, or a herniated disk. Radicular pain is common in those with cauda equina lesions and may occur in the acute injury from disk herniation; however, in those with chronic SCI without cauda equina lesions, late onset of radiculopathy may develop from a Charcot spine (17).
Despite the high prevalence of pain problems after SCI and the existence of a number of studies that have increased our knowledge of the pathophysiologic changes that occur after SCI, much is still not known concerning the mechanism(s) that produce chronic pain or why it develops in one person with SCI but not in another. Treatment remains largely empirical and should include a comprehensive approach to the patient. The most commonly recommended oral pharmacological agents for chronic pain fall into 3 major categories: antidepressants, anticonvulsants, and analgesics. Historically, antidepressants, especially tricyclic antidepressants, have been considered first-line drugs for neuropathic pain after SCI based on clinical experience and case reports (3,18–20). Unfortunately, however, the evidence for the efficacy of antidepressants for treating chronic pain from randomized controlled trials in SCI has been negative thus far (20,21).
Anticonvulsants, most notably gabapentin, are increasingly being used for neuropathic pain and are now considered first-line drugs. In a recent randomized controlled trial, gabapentin was found more effective than placebo for neuropathic pain in persons with complete paraplegia (23). In this study, the dosage of gabapentin was increased to a maximum of 3,600 mg/day if tolerated, regardless of efficacy at a lower dose. Using a cross-over design, subjects were given a 4-week titration period followed by a 4-week stable dosing period. About a 50% reduction in pain was found at the end of the titration period with gabapentin and about 60% at the end of the stable dosing period. However, other anticonvulsants have not shown efficacy in randomized controlled trials for the treatment of chronic pain in persons with SCI (24,25).
Analgesics that are typically useful for musculoskeletal pain problems such as nonsteroidal anti-inflammatory drugs (NSAIDS), acetaminophen, and opioids are generally not found as helpful in relieving neuropathic pain (20,26,27). Moreover, the use of opioids is not without controversy, especially in persons with SCI who may be particularly sensitive to opioid side effects, such as constipation.
There are many patients who have not found relief of pain from oral agents and have therefore tried the intrathecal route of drug delivery. In one placebo-controlled trial, intrathecal administration of a bolus of baclofen was shown to provide a reduction in musculoskeletal and neuropathic pain (28), but long-lasting relief of neuropathic pain does not occur with the levels of this drug that are usually delivered (29).
Reports of the use of alternative therapies suggest that many people with SCI are seeking nontraditional methods for pain relief (30–34). In a previous study of community-dwelling individuals with SCI-related chronic pain by our group, many types of treatments were reported to have been tried by patients (35). These included oral medications, invasive therapies, physical therapy, counseling/psychotherapy, and alternative treatments. However, only a few of these treatments were rated as more than somewhat helpful.
There is a need to better understand the efficacy of various treatments for chronic pain in persons with SCI. To the extent that specific treatments can be identified that are rated as consistently helpful, these treatments should be considered as “first-line” interventions for patients with SCI presenting with chronic pain problems. On the other hand, if no single treatment or set of treatments can be identified as being consistently helpful, this would argue for the need to (a) continue to provide pain treatments on an empirical basis to find the treatment or treatments that are uniquely effective for each patient and (b) support research that identifies and develops new treatments that might be effective for SCI-related chronic pain problems.
In a longitudinal study recently completed, pain prevalence and psychosocial indicators of function were examined in persons from a community sample with chronic SCI (36). This study seeks to increase our understanding of the types and efficacy of treatment from the subsample in this study who reported chronic pain. This study represents a replication and extension of our previous study on pain treatments in individuals with SCI. In our previous study, we found that a great variety of pain treatments are tried by these patients but few are consistently helpful (35). One limitation of the previous study was that it provided only a limited number of pain treatments for patients to select and rate and also did not provide information concerning the length of pain relief produced by those treatments that did provide at least some relief for some patients. This study provided patients with a more thorough list of possible pain treatments to rate. It also allowed them to indicate the extent to which these treatments provided pain relief and the length of time that the relief lasted.
METHODS
As indicated above, the participants for this study came from a survey study of pain in persons with SCI (36). In that survey, questionnaires were initially mailed to 339 individuals, and 147 completed questionnaires (48% of 309 possible after 30 surveys were excluded; 27 because of out-of-date addresses, 2 because the potential participants had deceased, and 1 because the potential participant could not complete the survey because of being hospitalized) were returned. Each questionnaire was accompanied by a consent form and a cover letter inviting the potential study participants to participate in the study. Subjects were paid $25 for completing and returning the consent forms and survey. The study procedures were approved by the University of Washington Human Subjects Review Committee.
The survey questionnaire included a number of questions assessing demographic and SCI-related descriptive information (age, education level, employment status, race/ethnicity, marital status, time since SCI, and SCI level). Survey respondents were also asked to indicate the presence or absence of any recent pain problems using the following question: “Are you currently experiencing, or have you in the past 3 months experienced, any pain (other than occasional headaches or menstrual cramps)?” Respondents who answered “yes” to this question were asked to rate the average intensity of this pain during the past week on a 0 to 10 numerical rating scale, with 0 = no pain and 10 = pain as bad as could be.” Such 0 to 10 scales have shown their validity as measures of pain by their strong association with other measures of pain intensity, as well as by their responsivity to treatments known to impact pain (37).
The 117 respondents to this survey who reported having a pain problem were asked to indicate whether or not they had received or were currently receiving any 1 of 26 different pain treatments, including 10 oral medications or medication groups, 8 other standard pain treatment modalities, 7 alternative pain treatments, or any “other” treatment for pain (Tables 2 and 3 show a list of the treatments asked about). For each treatment received, subjects were asked to indicate the amount of relief each treatment provided on a 0 (no relief) to 10 (complete relief) scale and to indicate the length of time that any pain relief obtained usually lasts on a 6-point categorical scale (minutes, hours, days, weeks, months, years). The relief and categorical length of relief rating scales were developed specifically for this survey.
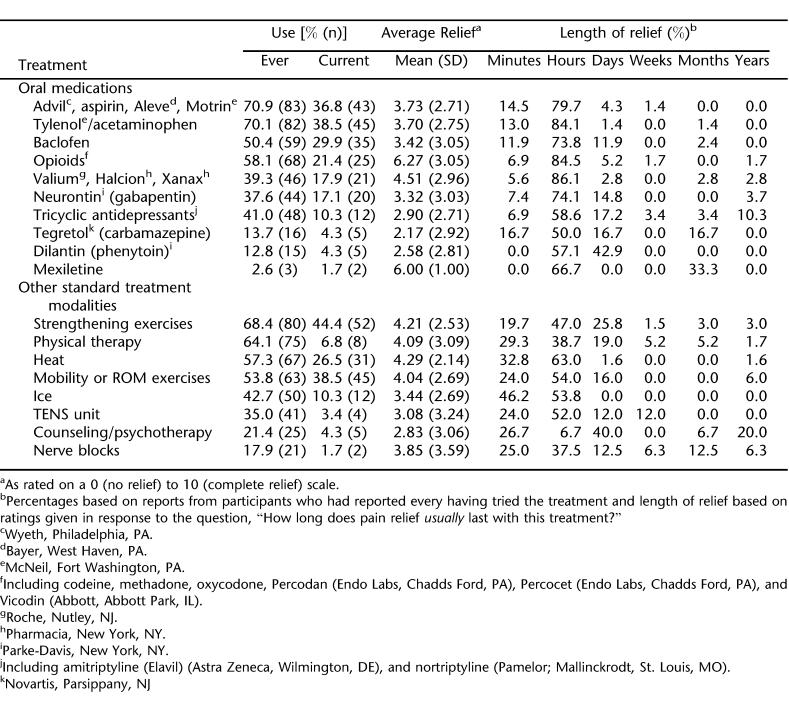
Table 2.
Past and Current Oral Medications and Standard Treatments for Pain, Average Relief Provided by Each Treatment, and Average Length of Relief Provided by Each Treatment
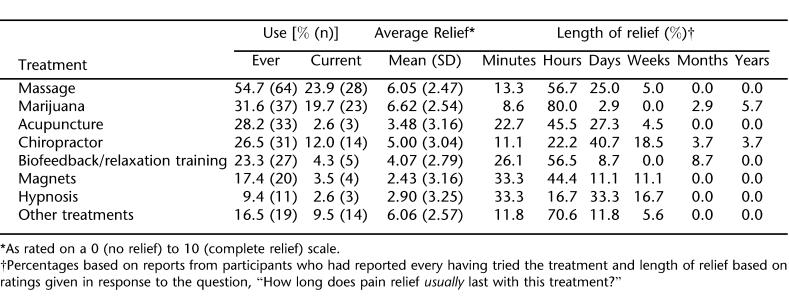
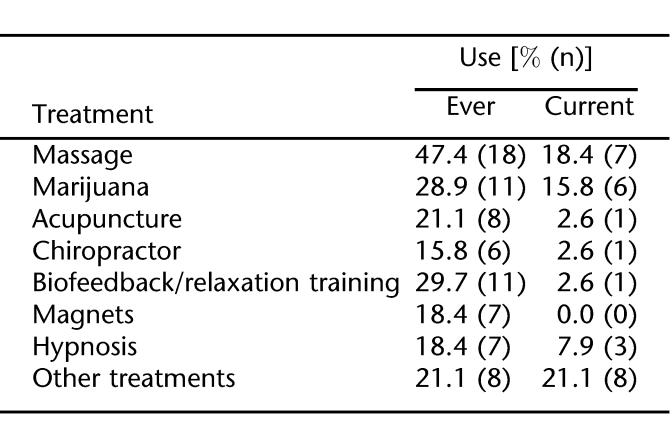
Table 3.
Past and Current Alternative and Other Treatments for Pain, Average Relief Provided by Each Treatment, and Average Length of Relief Provided by Each Treatment
RESULTS
Subject Characteristics
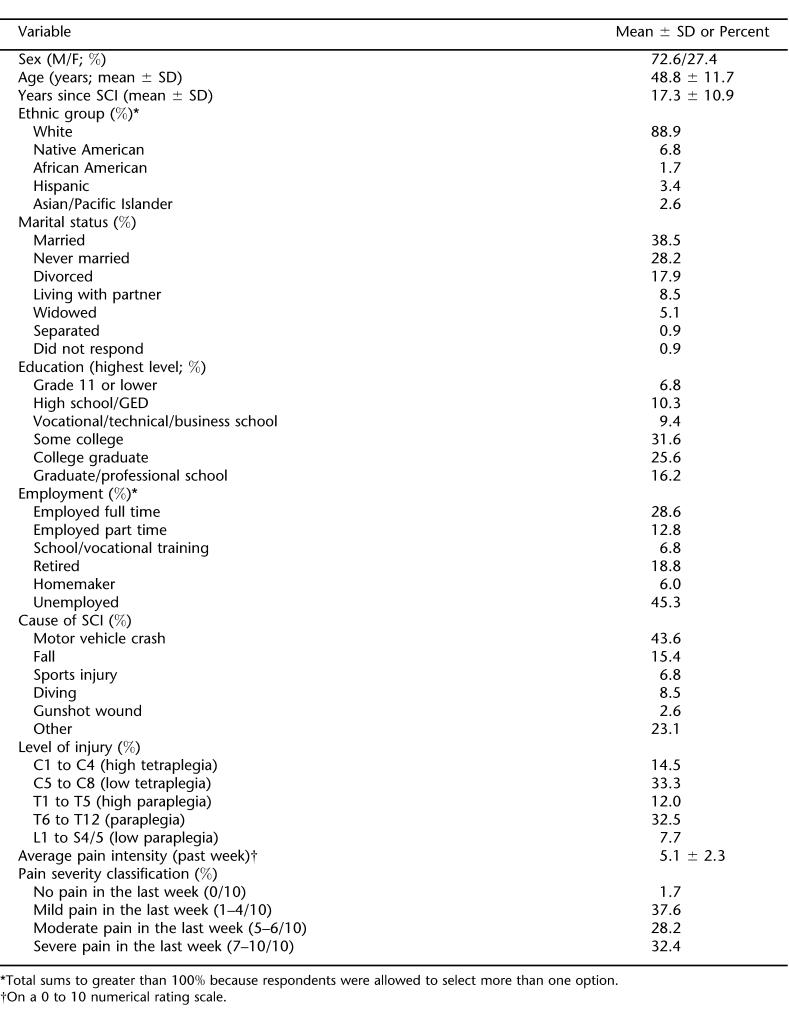
Demographic and SCI-related descriptive information of the 117 respondents reporting pain are presented in Table 1. The mean age of the study subjects was 48.8 ± 11.7 (SD) years (range, 21–79 years). As previously reported in the samples from which the current subjects were drawn (16,36,38), there was a wide degree of variability in the number of years since SCI (range, 3.2–57.4 years; mean, 17.3 ± 10.4 years). The average pain intensity (during the past week) of the study participants was 5.1 ± 2.3 on the 0 to 10 numerical scale. Among the respondents, 37.6% with pain reported mild pain (1–4 on the 0–10 scale) (39,40), 28.2% reported moderate pain (5–6 on the 0–10 scale), and 32.4% of the respondents reported that they experienced severe pain (:7 on the 0–10 scale). Two respondents who said they had experienced a pain problem in the last 3 months reported an average pain intensity of 0 during the past week on the 0 to 10 scale.
Table 1.
Demographic and Descriptive Information of All Survey Respondents Reporting Pain (n = 117)
Use of Pain Treatments
Oral Medication Use. Of the respondents reporting pain, the majority (all but 4; 96.6%) reported having taken at least one of the pain medications listed on the survey at some point in time. Most reported having tried more than one medication (mean and median number of medications tried, 3.97 and 4, respectively; range, 0–9). At the time of survey completion, 95 (81.2%) of the subjects with pain reported currently taking at least one of the survey medications, although the majority were taking more than one (mean and median number of medications taken at the time of survey completion were 1.82 and 2, respectively; range, 0–6).
Table 2 lists (a) the number and percent of patients with pain who reported ever having taken the oral medications listed on the survey; (b) the number and percent of patients who are currently taking the medications listed on the survey; (c) the average pain relief provided by these medications (as reported by those who have tried them); and (d) the length of time of any pain relief. As can be seen, the medications tried most often by these subjects were NSAIDs (tried by 83 [71%] of respondents with pain), and acetaminophen (tried by 82 [70%]). A little more than one half of the patients (43 and 45 of the sample, respectively) who had ever tried these are still taking these classifications of medications. All of the medications tend to provide pain relief for hours (but rarely provide relief for days or longer). Opioids produced the greatest degree of pain relief, on average (mean, 6.27 ± 3.05 on the 0–10 scale of pain relief), but these were also among the treatments that were least likely to be continued by those who tried them (25 of 68 [37%] of those who tried opioids continued to use them); only 21% of the survey respondents were currently using an opioid. Only one other medication was reported to have a similar effect on pain relief as opioids; mexiletine had an average relief rating of 6.0 ± 1.00, but only 3 patients with pain reported ever having tried this medication; 2 of these, or 67% of those who tried mexiletine, continued to use it. Dilantin (phenytoin) seemed to have the longest lasting effect on pain relief (with 57% reporting that relief lasts for hours and 43% reporting that it lasts for days), but it provided relatively little relief overall (mean, 2.58 ± 2.81). Tegretol (carbamazepine) seemed to provide the least relief overall (mean, 2.17 ± 2.92), but Dilantin (mean, 2.58 ± 2.81) and tricyclic antidepressants (mean, 2.90 ± 2.71) were also rated as providing relative little relief compared with some of the other medications.
Standard Pain Treatments. One hundred three (88%) of the respondents with pain reported that they had used at least one of the 8 specific (standard) pain treatments listed on the survey at some point in time, and 81 (69%) were currently using or being given at least one of the treatments. None of the 8 treatments listed provided a relief rating of 5 or more on the 0 to 10 relief scale, but 4 of them were rated as providing a relief rating of 4 or more on average: strengthening exercises, physical therapy, heat, and mobility or range of motion exercises. With the exception, perhaps, of counseling, the standard pain treatments tended to provide relief for only minutes or hours. The relief provided by strengthening exercises was rated as lasting for days by 26% of the respondents who had participated in this treatment, and counseling was rated as lasting for days by 40% and years by 20% of those who participated in this treatment. However, the pain relief provided by counseling tended to be relatively low on average (mean, 2.83 ± 3.06).
Alternative and Other Pain Treatments. Eighty-five (73%) of the respondents with pain reported that they had tried at least one of the 7 alternative pain treatments listed on the survey. Different alternative treatments had been tried by different numbers of respondent (Table 3); in descending order, these frequencies were massage (tried by 55%), marijuana (32%), acupuncture (28%), chiropractic manipulations (27%), biofeedback/relaxation training (23%), magnets (17%), and hypnosis (9%). The most relief was provided by massage (mean, 6.05 ± 2.47) and marijuana (mean, 6.62 ± 2.54), although chiropractic care was also among the treatments that provided greatest pain relief (mean, 5.00 ± 3.04). As with the other treatments, the relief provided by these treatments tended to last for minutes or, more often, hours. However, pain relief from massage and acupuncture lasted for days for a subgroup of about 25% of those who received these treatments. In patients who received chiropractic care, pain relief lasted for days in 41% and for weeks in 19%. Similarly, of those who received hypnotic treatment, the pain relief only lasted for days (33%) or weeks (17%), but the amount of relief provided by hypnotic treatment tended to be low (mean, 2.43 ± 3.16).
Nineteen patients reported having ever tried some other pain treatment (not specifically listed on the survey), and 15 of these were still receiving or participating in these other treatments. The other treatments that were written into the survey included other medications, exercise and increased activity, and rest and relaxation techniques. Of these, 10 (self-hypnosis, clonazepam, “staying busy and having a good attitude,” “healer,” “body energy work,” sex, epidural catheter, lying down, dorsal column stimulator, and yoga) were reported as providing relief ratings of 5 or greater on the 0 to 10 relief scale. Pain relief tended to last for hours for the great majority of these other treatments, although “body energy work” was reported to last for weeks by the subject who participated in this treatment, and aerobic exercise (relief rating, 4 on the 0–10 scale) and yoga (relief rating, 9) provided relief for days.
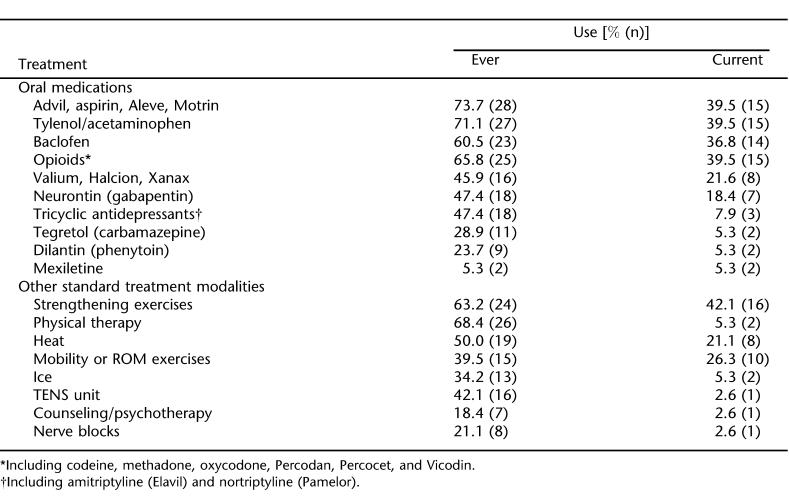
Pain Treatments Used by Respondents With Severe Pain. The frequencies with which patients with severe pain (average pain intensity reported as 7 or greater on the 0 to 10 scale, N = 38) used the pain treatments are reported in Tables 4 and 5. In only 4 instances did the rate of treatment use seem to vary in respondents with severe pain compared with respondents who did not report severe pain. Specifically, patients with severe pain reported the following: (a) a greater frequency of use of opioids [39.5% compared with 12.5%, χ2(1) = 9.44, P <0.01]; (b) a greater frequency of use of other pain treatments [21.1% vs 7.89.5%, χ2(1) = 3.04, P <0.10]; (c) less use of mobility or range of motion exercises [26.3% vs 44.3%, χ2(1) = 2.79, P <0.10]; and (d) less use of chiropractic care [2.6% vs 16.5%, χ2(1) = 3.44, P <0.10]. Otherwise, there was little difference in the frequency of pain treatment use between patients with and without severe pain.
Table 4.
Past and Current Oral Medications and Standard Treatments for Pain Among Participants Reporting Severe Pain (Average Pain Intensity Rating Greater Than or Equal to 7 on the 0 to 10 Scale, N = 38)
Table 5.
Past and Current Alternative and Other Treatments for Pain Among Participants Reporting Severe Pain (Average Pain Intensity Rating Greater Than or Equal to 7 on the 0 to 10 Scale, N = 38)
DISCUSSION
These findings indicate that a large number of pain treatments had been tried and were currently being used by these individuals with SCI and chronic pain. Importantly, many treatments that are now considered first-line treatments for chronic pain are not frequently used and are associated with only minimal levels of pain relief. For example, only about one third of those with pain had tried gabapentin. Less than one half of those who had tried it (45%; 17% of the entire sample) were still using it, and relatively low levels of pain relief were reported in response to this treatment. The lack of trying or the relatively high frequency of discontinuing this treatment among those who had tried this medication may have been caused by cost, overall lack of efficacy, intolerable side effects, lack of knowledge of this treatment among some treatment providers, or some combination of these. The reasons for not trying or for discontinuing use were not assessed for gabapentin or any other treatment in this survey study.
Baclofen provided about the same degree of pain relief as gabapentin, although slightly more of the sample had tried this medication (50%), and a greater number of patients who had tried this medication were still using it. Previous research has shown that intrathecal baclofen provides relief for musculoskeletal but not neuropathic pain (29). Also, research has shown that oral baclofen produces little pain relief in central pain syndromes (5). This previous research, when considered in light of these findings, suggests the possibility that muscle spasms or other nonneuropathic pain generators may be playing a role in the production of pain in some persons with SCI and chronic pain. Certainly, these findings suggest that baclofen should be considered if the patient presents with significant or bothersome pain that the clinician suspects may be musculoskeletal in origin.
As in our previous report (35), opioids were reported to provide the greatest degree of pain relief. However, although opioids had been tried by 58% of this sample, they were still being used by only 21% (ie, only a little over one third of the subjects who had tried opioids continued to take this class of drugs). Persons with severe pain, however, reported a greater frequency of use of opioids than those with mild or moderate pain. Only recently have registered clinical trials using opioids in SCI been reported. In one such study, Attal et al (41) used intravenous morphine or placebo in 15 patients (9 with SCI and 6 with stroke) with central pain and found no significant difference in pain relief in those given morphine compared with placebo. When oral morphine was subsequently given to those (n = 7) who had responded to intravenous morphine, only 3 patients (20%) continued with oral morphine more than 12 months. None of those who were nonresponders continued on morphine more than 6 months. The side effects of opioids, especially on bowel activity and mental clarity, the tolerance that may develop, and the addictive potential of opioids are significant issues that make their chronic use less desirable.
Of the 8 nonmedication standard treatment modalities, 69% of the sample reported that they were currently using at least one of these treatments. Pain relief was highest for those involving strengthening exercises or heat. Because the application of heat is contraindicated for areas of the body that are insensate, it is likely that heat is used for pain from musculoskeletal sources.
Of all the treatments rated, marijuana was reported to give the greatest pain relief. It had been tried by 32% and was being used currently by 23% of the sample. Most of those using marijuana reported hours of pain relief after treatment. Marijuana is also reported to reduce spasticity, which could contribute, at least in part, to pain relief in some patients (42). In 1976, Dunn and Davis reported that marijuana use in men with SCI decreased pain in 44% (43). A more recent survey from the United Kingdom found that a small number of persons with pain and SCI reported use of marijuana for pain (44). However, the use of marijuana for medical purposes remains very controversial in the United States.
The length of relief from pain from oral medications tended to be hours, which is generally what one would expect from such agents, with one notable exception. Antidepressants were reported to provide years of relief for about 10% of those who had tried them; however, the pain relief from antidepressants was modest. Counseling or psychotherapy also provided years of relief for 20% of the sample. However, only one person with severe pain was currently using counseling or psychotherapy. Of the 38 subjects with severe pain, medications were the most common form of treatment; however, the majority had received physical therapy or strengthening exercises, and 42% were currently doing strengthening exercises for pain relief. These results raise the possibility that exercise and physical activity may benefit persons with SCI and chronic pain; strengthening exercises may be particularly helpful for those with severe pain (pain intensity <7/10). However, given the descriptive nature of this study, conclusions regarding the casual impact of any treatment, including exercise, on chronic pain, cannot be made from these data. At most, the findings indicate that clinical trials of exercise treatment for chronic pain problems in persons with SCI are warranted.
This study has several methodological limitations. First, the response rate (49%) to the primary survey was low (36), which limits the generalizability of the findings. Also, the potential survey respondents were selected from a sample of individuals with SCI who had responded to previous surveys. This may also limit the generalizability of the findings to the degree that this sample may be not representative of all persons with SCI. In addition, the type of pain (eg, musculoskeletal vs neuropathic) that was experienced and relieved by each treatment is unknown. This makes it difficult to determine which treatment may have relieved or failed to relieve specific types of pain. However, studies indicate that most patients with SCI and chronic pain have more than 1 pain problem (16,38,45,46), so even if it were possible to know the specific type(s) of pain experienced by the participants, it would likely have been difficult to know which treatments alleviated (or did not alleviate) which pain problem. Finally, although we asked respondents to indicate which medications they had tried and were currently using, we did not assess the exact doses of these medications, nor could we have been certain that respondents provided accurate information about dose had we asked. Therefore, we cannot say whether adequate doses of any of the oral medications had been reached or whether medication treatments had been tried for a sufficient duration to be effective.
CONCLUSION
Despite the study's limitations, the findings provide additional information about the pain treatments tried by individuals with chronic pain and SCI and their efficacy. We found that persons with severe pain report some relief from the use of exercise. We also found that, although antidepressants did not provide high levels of pain relief, unlike most other medications, they can provide long-lasting relief for some of those patients who respond to these medications. Gabapentin had been tried by almost one half of those with severe pain but was discontinued by many. Future studies are needed to help determine the best combination of pain treatment modalities that can provide pain relief for long periods of time, because at present, recovery from SCI remains an unconquered challenge.
Footnotes
This study was supported by National Institutes of Health, National Institute of Child Health and Human Development, National Center for Rehabilitation Research grant P01 HD33988 and National Institute on Disability and Rehabilitation Research, Office of Special Education and Rehabilitative Services, US Department of Education grant H133N00003.
REFERENCES
- Cardenas DD, Bryce TN, Shem K, Richards JS, Elhefni H. Gender and minority differences in the pain experience of people with spinal cord injury. Arch Phys Med Rehabil. 2004;85:1774–1781. doi: 10.1016/j.apmr.2004.04.027. [DOI] [PubMed] [Google Scholar]
- Dalyan M, Cardenas DD, Gerard B. Upper extremity pain after spinal cord injury. Spinal Cord. 1999;37:191–195. doi: 10.1038/sj.sc.3100802. [DOI] [PubMed] [Google Scholar]
- Donovan WH, Dimitrijevic MR, Dahm L, et al. Neurophysiologic approach to chronic pain following spinal cord injury. Paraplegia. 1982;20:135–146. doi: 10.1038/sc.1982.27. [DOI] [PubMed] [Google Scholar]
- Frisbie JH, Aguilera EJ. Chronic pain after spinal cord injury: an expedient diagnostic approach. Paraplegia. 1990;28:460–465. doi: 10.1038/sc.1990.62. [DOI] [PubMed] [Google Scholar]
- Leijon G, Bolvie J. Pharmacological treatment of central pain. In: Casey KL, editor. Pain and Central Nervous System Disease: The Central Pain Syndrome. New York: Raven Press; 1991. pp. 257–266. [Google Scholar]
- Cardenas DD, Turner JA, Warms CA, Marshall H. Classification of chronic pain associated with spinal cord injuries. Arch Phys Med Rehabil. 2002;83:1708–1714. doi: 10.1053/apmr.2002.35651. [DOI] [PubMed] [Google Scholar]
- Bonica JJ. Introduction: semantic, epidemiologic, and educational issues. In: Casey KL, editor. Pain and Central Nervous System Disease. New York: Raven Press; 1991. pp. 13–30. [Google Scholar]
- Britell CW, Mariano AJ. Chronic pain in spinal cord injury. In: Walsh NE, editor. Physical Medicine and Rehabilitation: State of the Art Reviews. Philadelphia, PA: Hanley and Belfus; 1991. pp. 71–82. [Google Scholar]
- Botterell EH, Callaghan JC, Jousse AT. Pain in paraplegia: clinical management and surgical treatment. Proc R Soc Med. 1954;47:281–288. doi: 10.1177/003591575404700409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen MJ, McArthur DL, Vulpe M, Schandler SL, Gerber KE. Comparing chronic pain from spinal cord injury to chronic pain of other origins. Pain. 1988;35:57–63. doi: 10.1016/0304-3959(88)90276-X. [DOI] [PubMed] [Google Scholar]
- Davis L, Martin J. Studies upon spinal cord injuries (ii): the nature and treatment of pain. J Neurosurg. 1947;4:483–491. doi: 10.3171/jns.1947.4.6.0483. [DOI] [PubMed] [Google Scholar]
- Kaplan LI, Grynbaum BB, Lloyd KE, Rusk HA. Pain and spasticity in patients with spinal cord dysfunction. Results of a follow-up study. JAMA. 1962;182:918–925. doi: 10.1001/jama.1962.03050480024006. [DOI] [PubMed] [Google Scholar]
- Nepomuceno C, Fine PR, Richards JS, et al. Pain in patients with spinal cord injuries. Arch Phys Med Rehabil. 1979;60:605–609. [PubMed] [Google Scholar]
- Richards JS, Meredith RL, Nepomuceno C, Fine RR. Psychosocial aspects of chronic pain in spinal cord injury. Pain. 1980;8:355–356. doi: 10.1016/0304-3959(80)90079-2. [DOI] [PubMed] [Google Scholar]
- Rose M, Robinson JE, Ells P, Cole JD. Pain following spinal cord injury: results from a postal survey. Pain. 1988;34:101–102. doi: 10.1016/0304-3959(88)90187-X. [DOI] [PubMed] [Google Scholar]
- Turner JA, Cardenas DD, Warms CA, McClelland JM. Chronic pain associated with spinal cord injuries: a community survey. Arch Phys Med Rehabil. 2001;82:501–508. doi: 10.1053/apmr.2001.21855. [DOI] [PubMed] [Google Scholar]
- Standaert C, Cardenas DD, Anderson P. Charcot spine as a late complication of spinal cord injury. Arch Phys Med Rehabil. 1997;78:221–224. doi: 10.1016/s0003-9993(97)90267-7. [DOI] [PubMed] [Google Scholar]
- Farkash AE, Portenoy RK. The pharmacological management of chronic pain in the paraplegic patient. J Am Paraplegia Soc. 1986;9:41–50. doi: 10.1080/01952307.1986.11719623. [DOI] [PubMed] [Google Scholar]
- Fenollosa P, Pallares J, Cervera J, et al. Chronic pain in the spinal cord injured: statistical approach and pharmacological treatment. Paraplegia. 1993;31:722–729. doi: 10.1038/sc.1993.114. [DOI] [PubMed] [Google Scholar]
- Loubser PG, Donovan WH. Chronic pain associated with spinal cord injury. In: Narayan RK, Wilberger JE, Povlishock JT, editors. Neurotrauma. New York: McGraw-Hill; 1996. pp. 1311–1322. [Google Scholar]
- Cardenas DD, Warms CA, Turner JA, Marshall H, Brooke MM, Loeser JD. Efficacy of amitriptyline for relief of pain in spinal cord injury: results of a randomized controlled trial. Pain. 2002;96:365–373. doi: 10.1016/S0304-3959(01)00483-3. [DOI] [PubMed] [Google Scholar]
- Davidoff G, Guarracini M, Roth E, Sliwa J, Yarkony G. Trazodone hydrochloride in the treatment of dysesthetic pain in traumatic myelopathy: a randomized, double-blind, placebo-controlled study. Pain. 1987;29:151–161. doi: 10.1016/0304-3959(87)91032-3. [DOI] [PubMed] [Google Scholar]
- Levendoglu F, Ogun CO, Ozerbil O, Ogun TC, Ugurlu H. Gabapentin is a first line drug for the treatment of neuropathic pain in spinal cord injury. Spine. 2004;29:743–751. doi: 10.1097/01.brs.0000112068.16108.3a. [DOI] [PubMed] [Google Scholar]
- Drewes AM, Andreasen A, Poulsen LH. Valproate for treatment of chronic central pain after spinal cord injury: a double-blind cross-over study. Paraplegia. 1994;32:565–569. doi: 10.1038/sc.1994.89. [DOI] [PubMed] [Google Scholar]
- Finnerup NB, Sindrup SH, Bach FW, Ohannesen I, Jensen TS. Lamotrigine in spinal cord injury pain: a randomized controlled trial. Pain. 2002;96:375–383. doi: 10.1016/S0304-3959(01)00484-5. [DOI] [PubMed] [Google Scholar]
- Arner S, Meyerson BA. Lack of analgesic effect of opioids on neuropathic and idiopathic forms of pain. Pain. 1988;33:11–23. doi: 10.1016/0304-3959(88)90198-4. [DOI] [PubMed] [Google Scholar]
- Boivie J. Central pain. In: Wall PD, Melzack R, editors. Textbook of Pain. New York: Churchill-Livingstone; 1994. pp. 871–892. [Google Scholar]
- Herman RM, D'Luzansky SC, Ippolito R. Intrathecal baclofen suppresses central pain in patients with spinal lesions: a pilot study. Clin J Pain. 1992;8:338–345. [PubMed] [Google Scholar]
- Loubser PG, Akman NM. Effects of intrathecal baclofen on chronic spinal cord injury pain. J Pain Symptom Manage. 1996;12:241–247. doi: 10.1016/0885-3924(96)00152-2. [DOI] [PubMed] [Google Scholar]
- Rapson LM, Bieman IM, Bharatwal N, et al. Acupuncture treatment of pain in SCI. J Spinal Cord Med. 1995;18:133. [Google Scholar]
- Nayak S, Schoenberger NE, Shiflett SC. Acupuncture in the treatment of pain following spinal cord injury. Abstract #8. J Spinal Cord Med. 1998;21:358. [Google Scholar]
- Krauss HH, Godfrey C, Kirk J, Eisenberg DM. Alternative health care: its use by individuals with physical disabilities. Arch Phys Med Rehabil. 1998;79:1440–1447. doi: 10.1016/s0003-9993(98)90241-6. [DOI] [PubMed] [Google Scholar]
- Wainapel SF, Thomas AD, Kahan BS. Use of alternative therapies by rehabilitation outpatients. Arch Phys Med Rehabil. 1999;8:1003–1005. doi: 10.1016/s0003-9993(98)90102-2. [DOI] [PubMed] [Google Scholar]
- Nayak S, Matheis RJ, Agostinelli S, Shifleft SC. The use of complementary and alternative therapies for chronic pain following spinal cord injury: a pilot survey. J Spinal Cord Med. 2001;24:54–62. doi: 10.1080/10790268.2001.11753556. [DOI] [PubMed] [Google Scholar]
- Warms CA, Turner JA, Marshall HM, Cardenas DD. Treatments for chronic pain associated with spinal cord injuries: many are tried, few are helpful. Clin J Pain. 2002;18:154–163. doi: 10.1097/00002508-200205000-00004. [DOI] [PubMed] [Google Scholar]
- Jensen MP, Hoffman AJ, Cardenas DD. Chronic pain in individuals with spinal cord injury: a survey and longitudinal study. Spinal Cord. In press. [DOI] [PubMed]
- Jensen MP, Karoly P. Self-report scales and procedures for assessing pain in adults. In: Turk DC, Melzack R, editors. Handbook of Pain Assessment. 2nd ed. New York: Guilford Publications; 2001. pp. 15–34. [Google Scholar]
- Turner JA, Cardenas DD. Chronic pain problems in individuals with spinal cord injuries. Semin Clin Neuropsychiatry. 1999;4:186–194. doi: 10.153/SCNP00400186. [DOI] [PubMed] [Google Scholar]
- Jensen MP, Smith DG, Ehde DM, Robinson LR. Pain site and the effects of amputation pain: further clarification of the meaning of mild, moderate, and severe pain. Pain. 2001;91:317–322. doi: 10.1016/S0304-3959(00)00459-0. [DOI] [PubMed] [Google Scholar]
- Serlin RC, Mendoza TR, Nakamura Y, Edwards KR, Cleeland CS. When is cancer pain mild, moderate or severe? Grading pain severity by its interference with function. Pain. 1995;61:277–284. doi: 10.1016/0304-3959(94)00178-H. [DOI] [PubMed] [Google Scholar]
- Attal N, Guirimand F, Brasseur L, Gaude V, Chauvin M, Bouhassira D. Effects of IV morphine in central pain: a randomized placebo-controlled study. Neurology. 2002;58:554–563. doi: 10.1212/wnl.58.4.554. [DOI] [PubMed] [Google Scholar]
- Malec J, Harvey RF, Cayner JJ. Cannabis effect on spasticity in spinal cord injury. Arch Phys Med Rehabil. 1982;63:116–118. [PubMed] [Google Scholar]
- Dunn M, Davis R. The perceived effects of marijuana on spinal cord injured males. Paraplegia. 1974;12:175. doi: 10.1038/sc.1974.28. [DOI] [PubMed] [Google Scholar]
- Ravenscroft A, Ahmed YS, Burnside IG. Chronic pain after SCI. A patient survey. Spinal Cord. 2000;38:611–614. doi: 10.1038/sj.sc.3101073. [DOI] [PubMed] [Google Scholar]
- Stormer S, Gerner HJ, Gruninger W, et al. Chronic pain/dysesthesiae in spinal cord injury patients: results of a multicare study. Spinal Cord. 1997;35:446–455. doi: 10.1038/sj.sc.3100411. [DOI] [PubMed] [Google Scholar]
- Anke AG, Stenehjem AE, Stanghelle JK. Pain and life quality within two years of spinal cord injury. Paraplegia. 1995;33:555–559. doi: 10.1038/sc.1995.120. [DOI] [PubMed] [Google Scholar]