Abstract
Background/Objective:
Salmonella spondylodiskitis is an uncommon type of vertebral infection. The aim of this study was to present a case of progressive paraplegia caused by Salmonella spondylodiskitis and epidural abscess after endoscopic cholecystectomy.
Methods:
The patient underwent posterior instrumentation and posterior fusion between T6 and T12, hemilaminotomies at levels T8-T9-T10, and drainage of the abscess. Through a left thoracotomy, anterior T8–T10 corpectomy, debridement, anterior stabilization, and fusion were conducted.
Results:
Fifteen months later, final follow-up showed no complications secondary to the vertebral and hip surgeries, and neurological status improved to Frankel grade E. Laboratory investigations showed no evidence of Salmonella infection.
Conclusion:
Immunocompromised patients who undergo endoscopic intervention are vulnerable to Salmonella infections. One must consider Salmonella infection in those who develop acute progressive spondylodiskitis.
Keywords: Salmonella spondylodiskitis, Epidural abscess, Vertebral infection, Osteomyelitis, Paraplegia, Systemic lupus erythematosus, Immunocompromised state
INTRODUCTION
Spondylodiskitis is a rare condition that represents about 2% of all cases of osteomyelitis. It can be caused by either specific or nonspecific pathogens. Predisposing conditions include: diabetes mellitus, systemic diseases, pulmonary infections, renal deficiency treated with hemodialysis, immunodeficiency, and abdominal surgery. Salmonella spondylodiskitis is an uncommon type of vertebral infection. This report presents a case of a woman with systemic lupus erythematosus (SLE) who was undergoing immunosuppressive treatment. After endoscopic cholecystectomy, she developed acute, progressive paraplegia caused by spondylodiskitis and epidural abscess.
CASE REPORT
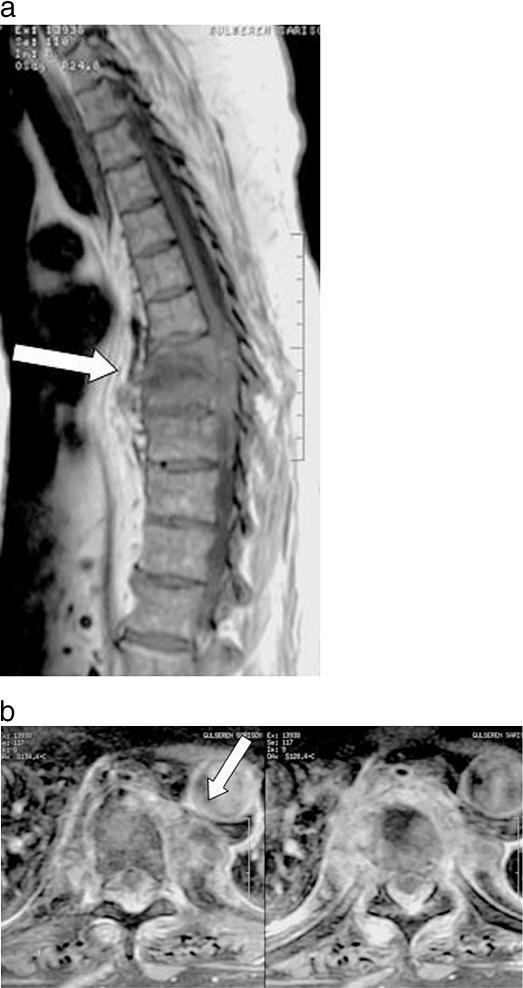
A 53-year-old female patient with SLE was followed for 1 year in a rheumatology clinic. For initial treatment for SLE, she received cyclophosphamide 500 mg intravenously, every 3 weeks for 5 months plus 80 mg/day, which was gradually decreased to 28 mg/day as the treatment continued. She underwent laparoscopic cholecystectomy 2 months before this report. One week later, she began complaining of leg pain that increased gradually in severity. She developed an abscess over the left trochanter major that was surgically drained. Salmonella was identified from the culture that was obtained from this abscess. At this point, she was admitted to our clinic with a neurological deficit of Frankel grade C. Because of pain, she was unable to lie supine for the past month and had to position herself by leaning over a box while sitting. Her pain did not respond to analgesic medication, including narcotics. Direct radiographic examination revealed no abnormalities. Magnetic resonance imaging (MRI) studies were conducted that showed spondylodiskitis compressing the spinal cord at levels T8, T9, and T10 anteriorly and posteriorly (Figure 1). Laboratory studies showed a white blood cell count of 7,200/mm3, and Grubel-Widal agglutination tests were positive at 1:320 titration; there were no signs of anemia.
Figure 1. Sagittal (a) and axial (b) MRI studies showing spondylodiskitis compressing the spinal cord at levels T8, T9, and T10, anteriorly and posteriorly.
Surgical Treatment
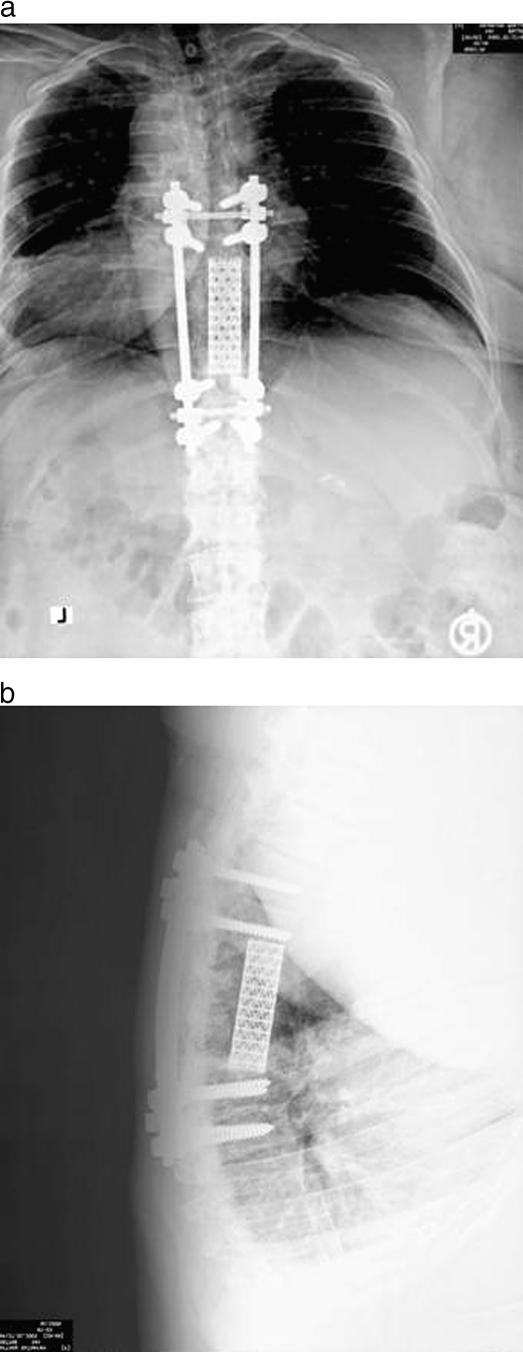
Posterior instrumentation and posterior fusion were performed between T6 and T12, hemilaminotomies were done at levels T8, T9, and T10, and the epidural abscess was drained. Through a left thoracotomy, T8–T10 anterior corpectomy, debridement and anterior stabilization, and fusion were conducted (Figure 2). Culture of tissue and abscess contents obtained during surgery confirmed infection by Salmonella typhimurium. Histopathological investigations revealed nonspecific infection.
Figure 2. Postoperative anteroposterior (a) and lateral (b) radiographs of this patient, who underwent posterior instrumentation and posterior fusion between T6 and T12, hemilaminotomies at levels T8, T9, and T10, and drainage of the abscess, followed by anterior T8–T10 anterior corpectomy, debridement and anterior stabilization, and fusion.
The patient received parenteral ciprofloxacin 400 mg twice a day for 6 weeks in addition to her SLE treatment regimen. A rehabilitation program was started immediately after surgery, and her neurological status improved to Frankel D within 2 months. At 2 months postoperatively, she fell while using the parallel bars during rehabilitation, and developed a displaced femoral neck fracture on the right and a nondisplaced femoral neck fracture on the left. Her rehabilitation program was resumed after right total hip replacement, as well as in situ fixation of the left hip through cannulated screws. Fifteen months later, final follow-up showed no complications secondary to the vertebral and hip surgeries, and her neurological status had improved to Frankel E. Laboratory investigations showed no evidence of Salmonella infection.
DISCUSSION
Infectious processes of the intervertebral disks and vertebral bodies are uncommon disorders. Spondylodiskitis accounts for nearly 2% of all bony infections (1). Although spondylodiskitis more commonly develops after surgical interventions, it also can develop spontaneously without prior surgery. It is encountered usually in patients with diabetes mellitus, systemic diseases, pulmonary diseases, and renal deficiency requiring hemodialysis; in patients who had organ transplantation; and in immuno-compromised patients (1). Spondylodiskitis can be caused by either specific or nonspecific agents. Spondylodiskitis caused by Salmonella is encountered very rarely (2).
Salmonella osteomyelitis is associated with sickle cell anemia or immunocompromised states (3,4). In osteo-myelitic patients without sickle cell anemia, the rate of Salmonella osteomyelitis is approximately 0.5%, and about one fourth of these patients develop vertebral involvement (5). Salmonella osteomyelitis can also be encountered in the absence of high-risk underlying medical conditions (2,6). S typhimurium and S enteritidis are the most common species and usually spread to the spine hematogenously. The most common spinal region involved is the lumbar region, and there is male predominance. The usual clinical manifestations and laboratory findings are high fever, dorsal or back pain, leukocytosis, and elevated erythrocyte sedimentation rate. Some cases follow a silent and insidious course (3,4). The diagnosis is made through direct identification of the pathogen from bone or paravertebral tissues.
S typhi can cause osteomyelitis at a single focus, but rarely, it may cause osteomyelitis with multiple osseous involvements (7). Our patient had multiple infectious foci at the T8-T9-T10 dorsal vertebrae, as well as at the left trochanter major. Salmonella infections usually present with early prodromes including gastrointestinal involvement, fever, and systemic findings. To our knowledge, only a few cases of neurological involvement caused by Salmonella spondylodiskitis have been reported in the English medical literature (8,9). Interestingly, this patient presented with progressive paraplegia.
Treatment consists of combined surgical and medical modalities. Emergent surgical intervention is needed in patients with neurological compromise. To eradicate Salmonella infection, medical treatment should be continued for 6 to 8 weeks in addition to surgical treatment. Ciprofloxacin is the antibiotic of choice for treating Salmonella infections (5). We performed aggressive surgical debridement and fusion, followed by ciprofloxacin therapy for 6 weeks. Early and mid-term follow-up showed eradication of Salmonella infection and maintenance of surgical stabilization.
CONCLUSION
Patients who undergo endoscopic intervention are vulnerable to Salmonella infection. This pathogen should be considered in cases of acute, progressive spondylodiskitis. MRI is the preferred means of detecting epidural abscess caused by Salmonella spondylodiskitis, a complication that may lead to early neurological compromise.
REFERENCES
- Maiuri F, Iaconetta G, Gallicchio B, Manto A, Briganti F. Spondylodiskitis. Clinical and magnetic resonance diagnosis. Spine. 1997;22:1741–1746. doi: 10.1097/00007632-199708010-00012. [DOI] [PubMed] [Google Scholar]
- Govender S, Parbhoo AH, Rasool MN, Maharaj J. Salmonella typhi spondylitis. J Pediatr Orthop. 1999;19:710–714. [PubMed] [Google Scholar]
- Acharya S, Bhatnagar P. Salmonella spinal osteomyelitis: a case report and review of literature. Neurol India. 2004;52:499–500. [PubMed] [Google Scholar]
- Wu KC, Yao TC, Yeh KW, Huang JL. Osteomyelitis in patients with systemic lupus erythematosus. J Rheumatol. 2004;31:1340–1343. [PubMed] [Google Scholar]
- Santos EM, Sapico FL. Vertebral osteomyelitis due to Salmonella: report of two cases and review. Clin Infect Dis. 1998;27:287–295. doi: 10.1086/514668. [DOI] [PubMed] [Google Scholar]
- Sucato DJ, Gillespie R. Salmonella pelvic osteomyelitis in normal children: report of two cases and a review of the literature. J Pediatr Orthop. 1997;17:463–466. [PubMed] [Google Scholar]
- Toth F, Szabo G, Abed R, Lovasz G. Multifocal simultaneous Salmonella typhi osteomyelitis in an immunocompetent adult. Scand J Infect Dis. 2002;34:770–772. doi: 10.1080/00365540260348590. [DOI] [PubMed] [Google Scholar]
- Akagi S, Shimada H, Kato I, Saito T, Ogawa R. Cervical spondylitis and epidural abscess caused by Salmonella enteritidis with tetraplegia. Orthopedics. 1998;21:1289–1291. doi: 10.3928/0147-7447-19981201-11. [DOI] [PubMed] [Google Scholar]
- Ben Taarit CH, Turki S, Ben Maiz H. Infectious spondylitis. Study of a series of 151 cases. Acta Orthop Belg. 2002;68:381–387. [PubMed] [Google Scholar]