Abstract
Background:
Bladder calculi are the second most common urological complication in those with spinal cord injury (SCI). Detection and removal of bladder stones are important to prevent possible complications.
Objective:
To determine the accuracy of bladder stone detection based on catheter encrustation in asymptomatic individuals with SCI.
Design:
Prospective cohort study.
Methods:
Cystoscopy findings in persons with SCI who were noted to have catheter encrustation at the time of catheter removal for their scheduled cystoscopy were used in this prospective study. Indwelling catheters were examined for encrustation at the time of removal as they were being prepared for cystoscopy. Cystoscopy was performed, and the presence or absence of bladder stones was noted.
Main Outcome Measures:
Presence or absence of bladder stones detected with cystoscopy in those with precystoscopy catheter encrustation.
Results:
Forty-nine individuals with indwelling catheters were evaluated. Overall, 17/49 (35%) individuals in this study had bladder stones. Catheter encrustation was noted in 13 patients. Of these 13 patients, 11 also had bladder stones. In other words, a positive result for catheter encrustation had a positive result for bladder stones 85% of the time. Thirty-six individuals had no catheter encrustation. Of these, 6 (16%) were found to have bladder stones.
Conclusions:
Encrustation of a catheter is highly predictive of the presence of bladder stones. This suggests that cystoscopy should be scheduled in a person undergoing a catheter change if catheter encrustation is noted.
Keywords: Spinal cord injuries, Neurogenic bladder, Bladder stones, Cystoscopy, Urethral catheter, Suprapubic catheter
INTRODUCTION
Indwelling urethral catheters are assuming a more important role in bladder management in individuals with spinal cord injury (SCI). This is caused in large part by shortened lengths of hospital stay after acute SCI and by a trend toward an increased likelihood of cervical injuries since 1994 (1). Because of these factors, people are often discharged from the hospital while their bladders are still in spinal shock. Those with poor hand function are unable to perform intermittent catheterization, so indwelling catheters are frequently used. It is especially difficult for a woman to catheterize herself, particularly with a high-level injury with adductor spasticity.
Bladder stones are the second most common urological complication in those with SCI (2,3). Approximately 36% of patients with indwelling catheters develop bladder stones within 8 years (4). Failure to detect bladder stones may lead to catheter blockage and bladder distention with the potential of autonomic dysreflexia in those with thoracic injuries at T6 or in those with recurrent urinary tract infections, hematuria, and/or recurrent catheter blockage (2). An individual will often report blockage of his catheter.
Unfortunately, there is currently no practical non-invasive method to detect bladder stones. Ultrasound requires distention of the bladder with water or normal saline, a technique that risks the development of autonomic dysreflexia or bacteremia (5). Abdominal radiographs detect approximately 20% of bladder stones in individuals with SCI (6). While computerized tomography (CT) would be expected to be accurate at detecting bladder stones, it is not a practical screening modality because of radiation exposure and high costs (7).
It was noted incidentally in our urology clinic that a large percentage of individuals who had catheter encrustation during routine annual urological evaluations were also found to have bladder stones detected during cystoscopy. This study was undertaken to determine the accuracy of predicting bladder stones based solely on catheter encrustation.
METHODS
As part of a hospital quality assurance study, the effectiveness of predicting bladder stones based on catheter encrustation was prospectively evaluated. Individuals with SCI who were undergoing cystoscopy were included in this study. Inclusion criteria for this study included routine annual evaluation of individuals with an indwelling catheter or follow-up of patients who had an indwelling catheter and recently had bladder stones removed. Exclusion criteria included individuals who had had a history of a new catheter put in within a week of their cystoscopic evaluation, because it takes about a week or more for catheters to become encrusted. Therefore, this group could have had catheter encrustation on a previous catheter change that would not have been detected by the authors at the time of this catheter change (8). All individuals in this study had their catheters changed at intervals of no more than 4 weeks. Those with recent bladder stones were usually switched to a 2-week catheter change.
Parameters recorded included urethral vs suprapubic catheter, the length of time since the catheter was last changed, whether or not the catheter was encrusted with stones, and whether or not bladder stones were found during cystoscopy. Stones were confirmed by stone analysis.
RESULTS
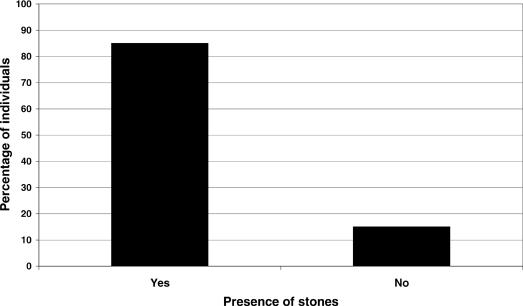
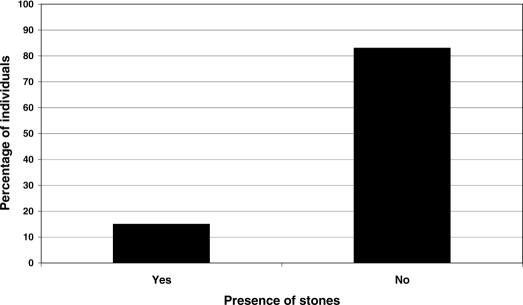
Forty-nine individuals with indwelling catheters were evaluated. Overall, 17/49 (35%) individuals in this study had bladder stones. Catheter encrustation was noted in 13 patients. Of these 13 patients, 11 also had bladder stones. In other words, a positive result for catheter encrustation had a positive result for bladder stones 85% of the time (Figure 1). Thirty-six individuals had no catheter encrustation. Of these, 6 (16%) were found to have bladder stones (Figure 2).
Figure 1. The percent of individuals with catheter encrustation who had bladder stones.
Figure 2. The percent of individuals with no catheter encrustation who had bladder stones.
DISCUSSION
Bladder stones frequently occur in individuals with indwelling catheters (3,9). They often form as a result of catheter encrustation (10,11). When a catheter is inserted into the bladder, it acts as a foreign body, and bacteria attach to it, initiating formation of a biofilm. This biofilm is composed of sheets of organisms that cover the catheter and secrete an extracellular matrix of bacterial glycocalyces and host proteins. Urinary crystals such as struvite and calcium phosphate are also incorporated into this biofilm (12–14). This process is accelerated by urease-producing bacteriuria, especially Proteus mirabilis, because urease alkalinizes the urine and promotes crystallization of struvite and calcium phosphate (15).
Encrustation of the internal lumen of the catheter often leads to catheter blockage (12–14). Changing the catheter would be expected to resolve the blockage. However, some pieces of stone fragments may be left behind in the bladder, even if the catheter is initially irrigated in an attempt to unblock the catheter. Catheter encrustation can also occur on the external balloon and catheter. On deflation of the bladder and removal of the catheter, small pieces of stone drop off the catheter and remain in the patient's bladder (Figure 3). These stone fragments serve as a nidus for further stone growth. Stone fragments left in the bladder from either situation can at any time be drawn up into the catheter and cause catheter obstruction, resulting in bladder distention and its attendant complications (16).
Figure 3. Example of multiple bladder stones being produced as an encrusted suprapubic catheter balloon is being deflated. The picture is taken through a cystoscope visualizing the catheter balloon through the urethra. The arrow shows the border of only one of the many stones.
The “gold standard” to detect bladder stones is through the use of cystoscopy (2,17). It has the advantage of also being used to remove the stones at the time of detection. However, this is an invasive procedure. If possible and practical, a noninvasive procedure would be preferred to determine who needs cystoscopy. However, bladder stone detection using noninvasive methods in those with SCI is difficult. Ultrasound has serious risks because it requires the bladder to be distended, which can cause autonomic dysreflexia or bacteremia (5). Another frequently used modality is abdominal radiographs. However, it has recently been reported that 80% of bladder stones are not detected by radiographs (6). This is because of a number of factors such as the small size and composition of bladder stones. Bladder stones are difficult to detect on radiographs because they are usually composed of a high percentage of organic matrix of bacterial glycocalyces and host proteins. Moreover, there may be increased abdominal gas in those with SCI, and the bladder stones are frequently thin with an eggshell appearance. There are no studies discussing the accuracy of CT scans at detecting bladder stones. CT scanning would be expected to be accurate; however, it is not practical as a screening modality because of radiation exposure and high costs (7). This study shows that catheter encrustation provides an excellent correlation with the presence of bladder stones. According to this study, if encrustation is present, there is an 85% (11/13) chance that bladder stones are also present. Therefore, if at any time a catheter is noted to be encrusted, a person should be scheduled for cystoscopy.
Cystoscopy is still recommended during an annual evaluation even if there is no catheter encrustation. This is because there are a small number of individuals who had bladder stones who did not have catheter encrustation. In addition, individuals may have had undocumented catheter encrustation sometime during the past year or other types of foreign bodies such as a pubic hair, which may have accidentally been pushed into the bladder during a catheter change.
CONCLUSION
Encrustation of a catheter at time of removal (change) is highly predictive of bladder stones. This study suggests that those with catheter encrustation should be scheduled for cystoscopy for definitive treatment (removal) of the bladder stones.
Acknowledgments
We thank Cecilia Jalacan, RN for her assistance with data collection.
Footnotes
This study was supported by the United Spinal Association.
REFERENCES
- Nobunga AI, Go BK, Karunas RB. Recent demographic and injury trends in people served by the model spinal cord injury care systems. Arch Phys Med Rehabil. 1999;80:1372–1382. doi: 10.1016/s0003-9993(99)90247-2. [DOI] [PubMed] [Google Scholar]
- Linsenmeyer TA, Stone JM, Stein S. Neurogenic bladder and bowel dysfunction. In: DeLisa JA, editor. Rehabilitation Medicine Principles and Practice. 4th ed. Philadelphia, PA: Lippincott-Raven; 2004. pp. 1619–1653. [Google Scholar]
- Cardenas D, Farrell-Roberts L, Sipski M, Rubner D. Management of gastrointestinal, genitourinary and sexual function. In: Stover SL, DeLisa JA, editors. Spinal Cord Injury—Clinical Outcomes From the Model Systems. Gaithersburg, MD: Aspen Publication; 1995. pp. 120–145. [Google Scholar]
- DeVivo MJ, Fine PR, Cutter GR, Maetz HM. The risk of bladder calculi in patients with spinal cord injuries. Arch Intern Med. 1985;145:428–430. doi: 10.1001/archinte.145.3.428. [DOI] [PubMed] [Google Scholar]
- Binard JE, Persky L, Lockhart JL, Kelley B. Intermittent catheterization the right way! (volume vs time-directed) J Spinal Cord Med. 1996;19:194–196. doi: 10.1080/10790268.1996.11719432. [DOI] [PubMed] [Google Scholar]
- Linsenmeyer MA, Linsenmeyer TA. Accuracy of bladder stone detection using abdominal x-ray after spinal cord injury. J Spinal Cord Med. 2004;27:438–442. doi: 10.1080/10790268.2004.11752234. [DOI] [PubMed] [Google Scholar]
- Brenner DJ, Elliston CD. Estimated radiation risks potentially associated with full-body CT screening. Radiology. 2004;232:735–738. doi: 10.1148/radiol.2323031095. [DOI] [PubMed] [Google Scholar]
- Park YI, Linsenmeyer TA. A method to minimize catheter calcification and bladder stones in individuals with spinal cord injury. J Spinal Cord Med. 2001;24:105–108. doi: 10.1080/10790268.2001.11753564. [DOI] [PubMed] [Google Scholar]
- Ord J, Lunn D, Reynard J. Bladder management and risk of bladder stone formation in spinal cord injured patients. J Urol. 2003;170:1734–1737. doi: 10.1097/01.ju.0000091780.59573.fa. [DOI] [PubMed] [Google Scholar]
- Favazza T, Midha M, Martin J, Grob BM. Factors influencing bladder stone formation in patients with spinal cord injury. J Spinal Cord Med. 2004;27:252–254. doi: 10.1080/10790268.2004.11753756. [DOI] [PubMed] [Google Scholar]
- Linsenmeyer TA, Ottenweller J. Bladder stones following spinal cord injury in the Sprague-Dawley rat. J Spinal Cord Med. 2003;26:65–68. doi: 10.1080/10790268.2003.11753663. [DOI] [PubMed] [Google Scholar]
- Hedelin H, Eddeland A, Larsson L, Pettersson S, Ohman S. The composition of catheter encrustations, including the effects of allopurinol treatment. Br J Urol. 1984;56:250–254. doi: 10.1111/j.1464-410x.1984.tb05382.x. [DOI] [PubMed] [Google Scholar]
- Stamm WE. Catheter-associated urinary tract infections: epidemiology, pathogenesis, and prevention. Am J Med. 1991;91:65S–71S. doi: 10.1016/0002-9343(91)90345-x. [DOI] [PubMed] [Google Scholar]
- Nickel JC, Ardern D, Downey J. Cytologic evaluation of urine is important in evaluation of chronic prostatitis. Urology. 2002;60:225–227. doi: 10.1016/s0090-4295(02)01733-8. [DOI] [PubMed] [Google Scholar]
- Mobley HL, Warren JW. Urease-positive bacteriuria and obstruction of long-term urinary catheters. J Clin Microbiol. 1987;25:2216–2217. doi: 10.1128/jcm.25.11.2216-2217.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohler-Ockmore J. Chronic urinary catheter blockage. Nurs Stand. 1991;30:5, 26–28. doi: 10.7748/ns.5.44.26.s37. [DOI] [PubMed] [Google Scholar]
- Linsenmeyer TA, Culkin D. APS recommendations for the urological evaluation of patients with spinal cord injury. J Spinal Cord Med. 1999;22:139–142. doi: 10.1080/10790268.1999.11719561. [DOI] [PubMed] [Google Scholar]