Abstract
Background/Objective:
To examine diabetes prevalence, care, complications, and characteristics of veterans with a spinal cord injury or disorder (SCI/D).
Methods:
A national survey of veterans with an SCI/D was conducted using Behavioral Risk Factor Surveillance System (BRFSS) survey questions. Data were compared with national Centers for Disease Control and Prevention BRFSS data for veteran and nonveteran general populations.
Results:
Overall prevalence of diabetes in individuals with an SCI/D was 20% (3 times higher than in the general population). Veterans with an SCI/D and veterans, in general, had a higher prevalence of diabetes across all age groups; however, those with an SCI/D who were 45 to 59 years of age had a higher prevalence than other veterans. One fourth of the persons with an SCI/D and diabetes reported that diabetes affected their eyes or that they had retinopathy (25%), and 41% had foot sores that took more than 4 weeks to heal. More veterans, both with (63%) and without an SCI/D (60%), took a class on how to manage their diabetes than the general population (50%). Veterans with an SCI/D and diabetes were more likely to report other chronic conditions and poorer quality of life than those without diabetes.
Conclusions:
Diabetes prevalence is greater among veterans with an SCI/D compared with the civilian population, but is similar to that of other veterans, although it may occur at a younger age in those with an SCI/D. Veterans with an SCI/D and diabetes reported more comorbidities, more slow-healing foot sores, and poorer quality of life than those without diabetes. Efforts to prevent diabetes and to provide early intervention in persons with SCI/D are needed.
Keywords: Spinal cord injuries; Diabetes mellitus; Self-care, Behavioral Factor Surveillance System; Prevalence; Veterans Affairs
INTRODUCTION
Diabetes mellitus is a significant chronic illness in the United States. The prevalence of diabetes in the United States for persons of all ages was greater than 6% in 2002, with the prevalence increasing with age (1). Estimated prevalence of diabetes in the general veteran population was 20% in 2000 (2). Diabetes mellitus was the third most common diagnosis for veterans in the Veterans Affairs (VA) health care system in 2002 (3). Diabetes is also a significant problem in persons with spinal cord injury or disorder (SCI/D), a lifelong condition affecting from 250,000 to 400,000 individuals in the United States (4). Studies have reported rates of diabetes from 13% to 22% in persons with an SCI/D (5,6).
Many disorders that are related to age in the general population, such as carbohydrate intolerance, insulin resistance, lipid abnormalities, and heart disease, are thought to occur prematurely (7) and at a higher prevalence in persons with SCI/D (8). These disorders are likely to be related to metabolic changes, changes in body composition that result from paralysis, obesity, loss of lean tissue from denervation, and greater adiposity above and below the level of neurologic injury (8). People with diabetes, together with their health care providers, can make efforts to reduce morbidity and mortality by maintaining near-normal glucose levels; optimizing the management of risk factors such as hypertension, high cholesterol, and obesity; and diagnosing early and managing complications from diabetes. However, literature has indicated that veterans with diabetes have limited knowledge about diabetes and diabetes care (9).
There is limited population-based information on people with an SCI/D and diabetes. National data sources such as the Behavioral Risk Factor Surveillance System (BRFSS) do not differentiate the data to the specificity of SCI/D diagnosis. Therefore, the aim of this research was to capture comparable data on diabetes for a population of veterans with an SCI/D. Using these data, the objectives of this article were (a) to assess the prevalence of self-reported diabetes and diabetes-related care and complications in veterans with an SCI/D and to make comparisons with both the general veteran population and the general population, and (b) among veterans with an SCI/D, to compare demographic, injury, and behavioral characteristics and clinical conditions in those with and without diabetes.
METHODS
Design
An anonymous cross-sectional survey was conducted in October 2003 with a national population of 18,372 individuals with spinal cord dysfunction (SCI/D and multiple sclerosis [MS]). The 2003 BRFSS survey data, available from the Centers for Disease Control and Prevention (CDC), were downloaded for comparison of the SCI/D cohort with the general veteran population and with the general population. The study was approved by the Institutional Review Board at Edward Hines Jr. VA Hospital.
Participants
The survey was distributed to Paralyzed Veterans of America (PVA) members, which included veterans with spinal cord dysfunction who use VA health care services and those who do not use VA for health care. Individuals with MS were excluded for the purpose of this study because they may have unique characteristics related to their MS that are beyond the scope of this study. Because this paper focused on veterans who received care in the VA health care system, veterans who used non-VA care only were excluded. General veteran and general population participants included survey respondents from the 2003 BRFSS survey conducted by the CDC.
Instruments
The BRFSS survey is a standardized instrument that has been extensively used by the CDC. It is used to monitor relevant basic health and risk behaviors within the US general population (10). CDC BRFSS questions were incorporated into a survey developed for use in a national population of veterans with an SCI/D. Questions from the 2002/2003 CDC BRFSS questionnaires (11) were used to design the 72-item Spinal Cord Dysfunction Health Care Questionnaire (SCD-HCQ). To keep the SCD-HCQ short (at the request of PVA), only select BRFSS sections were used, and a few additional questions were added to gain an understanding of spinal cord injury–specific characteristics (eg, level and duration of injury, age when injured).
CDC Database
In addition to the SCD-HCQ developed specifically for use in the SCI/D population, the national 2003 CDC population-based BRFSS survey data (12) were downloaded, weighted to account for differences in the probability of selection among geographic regions, and analyzed for comparisons to veteran and general (non-veteran) populations. CDC BRFSS data are directly weighted for the probability of selection of a telephone number, the number of adults and the number of telephones in a household. Additional information on weighting, including the weighting formula, can be found in the CDC BRFSS codebook (13). (The SCD-HCQ was nationally distributed by mail, so observations were not weighted.)
Variable Definitions
Diabetes. Diabetes status was derived from answering yes to the following question: “Have you ever been told by a doctor that you have diabetes?” This item was asked on both the 2003 CDC BRFSS and the SCD-HCQ. Possible responses included yes; yes, during pregnancy only; or no. Respondents who indicated that they had gestational diabetes only (n = 8) were not included in the analysis for this study.
Veteran. Veteran status was determined from the CDC 2003 BRFSS data by answering yes to ever having served on active duty in the US Armed Forces and being either retired or discharged from military service. All individuals who received the SCD-HCQ were veterans.
VA Health Care User. VA health care users included individuals who indicated having received all or some of their health care from VA facilities in the past 12 months.
Analysis
CDC population-based BRFSS data for 2003 (12) were downloaded and used to compare diabetes prevalence by age category among the general population, general veteran population, and the SCI/D veteran population. Trends in diabetes prevalence were examined for each group using Cochran-Armitage trend tests.
Frequencies of diabetes-related practices and complications were calculated for individuals with diabetes and an SCI/D, and χ2 tests were used to make comparisons with individuals who reported having diabetes in the general veteran and the general population.
Among the SCI/D population, χ2 or t tests, where appropriate, were used to assess differences between individual demographic, injury, and behavioral characteristics among persons with and without diabetes. Odds ratios were calculated to examine differences in presence of clinical conditions and quality of life indicators among persons with and without diabetes. Separate logistic regression models adjusted for age, race, marital status, duration of injury, employment status, and education level were used to generate odds ratios and 95% confidence intervals for each clinical condition. To determine statistical significance, an α level of 0.01 was used. Statistical analyses were performed using SAS 9.1 (SAS Institute Inc, Cary, NC) and Stata Version 9 software (Stata Corporation, College Station, TX).
RESULTS
Among the 18,372 eligible veterans with spinal cord dysfunction to whom the survey was distributed, 5,690 responded (response rate = 31%). Of the 5,690 respondents, 1,437 were excluded because they had MS, and an additional 516 were excluded because they only received their care at non-VA facilities. Therefore, the population of veterans with an SCI/D who received some or all of their care at the VA during the prior 12 months included in this study was 3,737. A total of 228,083 individuals were identified in the CDC database, of which 6,433 comprised the general veteran group and 221,650 comprised the general population group.
A separate analysis was conducted to assess whether the PVA survey respondents were representative of the larger population of veterans with an SCI/D. This was accomplished by using VA administrative databases to capture demographic and injury data for individuals with an SCI/D who had used the VA health care system in 2003. The VA data revealed comparable characteristics of veterans with an SCI/D: 98% male (vs 97% of survey respondents), mean age of 58 years (vs 60 years for survey respondents); 56% had a paraplegic level injury (vs 52%); mean age at injury of 36 years (vs 36 years), and mean duration of injury of 21 years (vs 24 years). The most notable differences were in race and marital status: 70% of veterans with an SCI/D seen at VA facilities were white (vs 81% of survey respondents), and 46% were married (vs 57% of survey respondents).
Comparison of Veterans With an SCI/D, General Veterans, and the General Population
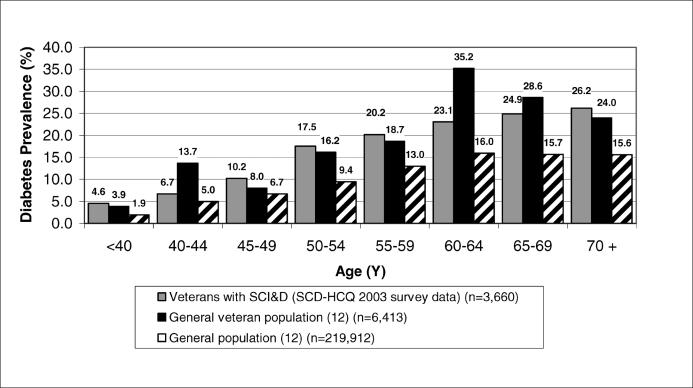
Figure 1 presents a comparison of diabetes prevalence by age groups for veterans with an SCI/D, the general veteran population, and the general population. The overall prevalence of self-reported diabetes in veterans with an SCI/D was 20%; nearly 3 times higher than the general population prevalence of 6.7% (P < 0.0001), but similar to that of other veterans (21%). In all 3 groups, the prevalence of diabetes increased with increasing age (Cochrane Armitage trend tests, P < 0.0001). Veterans, both with and without an SCI/D, had a higher prevalence of diabetes across all age groups. The general veteran group had a higher diabetes prevalence than veterans with an SCI/D in the 40 to 44 and 60 to 64-year age groups. Veterans with an SCI/D who were 45 to 49, 50 to 54, 55 to 59, and 65 to 69 years of age tended to be more likely to report diabetes than the general population.
Figure 1. Diabetes prevalence (%) by age group. Comparison of veterans with SCI/D, general veterans, and the general population.
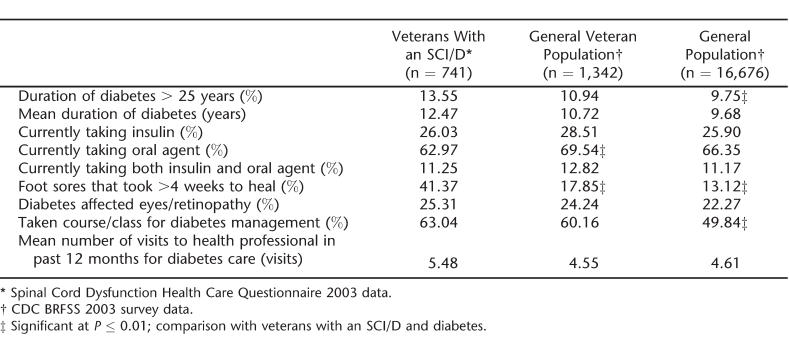
Table 1 presents a comparison of diabetes care management among the SCI/D veteran population, general veteran population, and the general population. Demographic characteristics of the 3 groups follow (detailed SCI/D characteristics are described in the next section). All groups were comprised of greater than 70% whites, and both veteran groups were comprised of more men than the general population. The general population was more likely to be employed (32%) than either veterans, in general, or veterans with an SCI/D (14% and 4%, respectively). However, veterans with an SCI/D were the most likely to have completed high school or beyond (89%) than either general veterans (86%) or the general population (77%) and more likely to be married (66%) than the general population (56%), but not other veterans (70%). The general population was younger (mean age = 57 years) than both veterans in general (66 years) and veterans with an SCI/D (64 years).
Table 1.
Diabetes-related Practices and Complications: Comparison of Veterans With SCI/D, General Veterans, and the General Population (With Diabetes)
Among veterans with an SCI/D, the mean duration of diabetes was 12 years (Table 1); there were no significant differences by group. A greater number of veterans with an SCI/D had diabetes for more than 25 years than the general population (P < 0.01). Nearly three quarters (73%) were diagnosed with diabetes after their spinal injury. Most respondents with an SCI/D and diabetes reported currently taking an oral agent (63%); however, this was less than oral agent use in general veterans (70%; P < 0.01). Twenty-six percent of persons with an SCI/D were currently using insulin, and 11% were using both insulin and an oral agent; this was similar to the general veteran and general populations. One quarter (25%) of persons with an SCI/D and diabetes reported being told by a doctor that diabetes has affected their eyes or that that they had retinopathy; this was not significantly different from the other two groups. Many more individuals with an SCI/D reported the occurrence of foot sores or irritations that took more than 4 weeks to heal (41%) compared with the general veteran group (18%, P < 0.01) and the general population (13%, P < 0.01). Higher percentages of veterans, both with (63%) and without an SCI/D (60%), than the general population (50%, P < 0.01) had taken a course or class on how to manage their diabetes. During the past year, the mean number of times that a veteran with an SCI/D saw a doctor, nurse, or other health professional for their diabetes was 5.5 times, whereas the general veteran population and the general population reported similar visits (4.6 for both), but these differences were not statistically different.
Comparison of Veterans With an SCI/D With and Without Diabetes
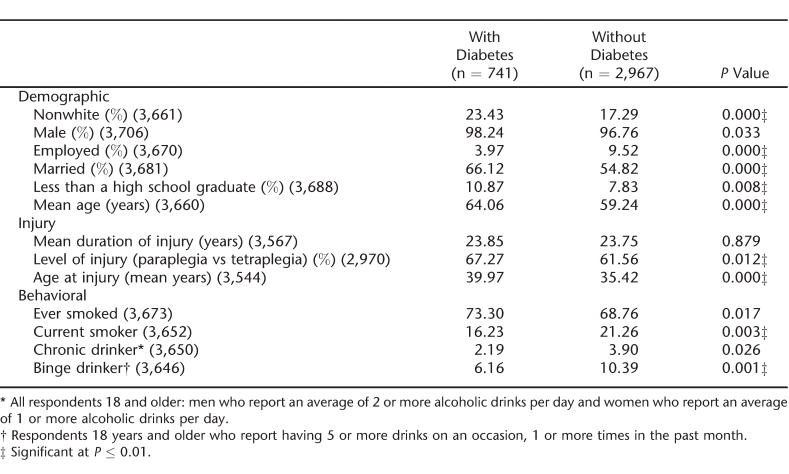
Demographic, injury, and health behavior characteristics of veterans with an SCI/D by diabetes status are listed in Table 2. Veterans with SCI/D and diabetes differed from those who reported that a doctor never told them that they had diabetes. Individuals with an SCI/D who had diabetes were more likely to be nonwhite (P < 0.0001), unemployed (P < 0.0001), married (P < 0.0001), older (P < 0.0001), and less educated (P = 0.008) than those without diabetes. There were no differences in the mean duration of injury between those with and without diabetes. Individuals with an SCI/D and diabetes were significantly more likely to have a paraplegic-level injury (P = 0.01) and tended to have been injured at an older age (P < 0.0001). Persons with diabetes and SCI/D were marginally more likely to have ever smoked cigarettes (marginal at 0.01 level, P = 0.017). However, persons without diabetes were significantly more likely to be current smokers (P = 0.003) and were more likely to be binge drinkers than veterans with an SCI/D who reported having diabetes.
Table 2.
Demographic, Injury, and Health Behavior Characteristics in Veterans With SCI/D by Diabetes Status
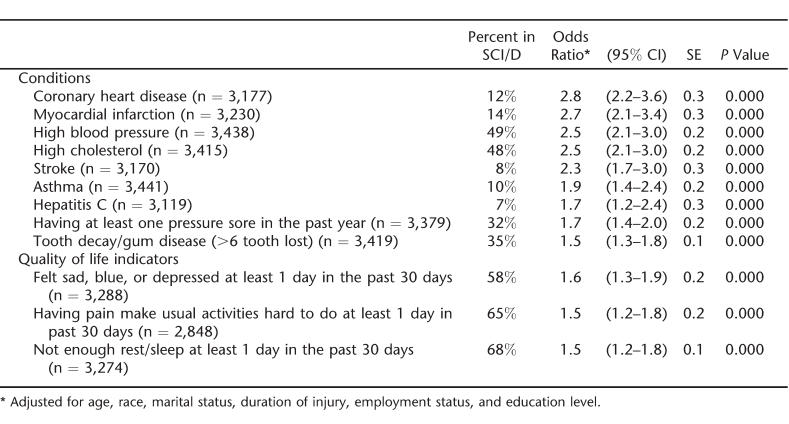
Odds ratios and 95% confidence intervals for clinical conditions among persons with an SCI/D and diabetes are presented in Table 3. Veterans with an SCI/D were more likely to report other clinical conditions if they had diabetes (independent of age, race, marital status, duration of injury, employment status, and level of education). Specifically, veterans with SCI/D and diabetes were nearly 3 times more likely to report coronary heart disease (P < 0.0001) and/or myocardial infarction (P < 0.001), 2.5 times more likely to report high blood pressure (P < 0.0001) and/or high cholesterol (P < 0.001), and 2 times more likely to report having had a stroke (P < 0.0001) than veterans with an SCI/D without diabetes. Asthma (P < 0.0001), hepatitis C (P < 0.0001), pressure ulcers (P < 0.0001), and tooth decay (P < 0.0001) were also more common in individuals with an SCI/D and diabetes. Sadness/depression, pain interfering with daily activities, and lack of and/or interrupted rest/ sleep were also significantly more likely to be reported by veterans with an SCI/D and diabetes than by those without diabetes.
Table 3.
Risk for Clinical Conditions and Quality of Life Indicators Based on Having Diabetes in Persons With SCI/D
DISCUSSION
The study findings show that there is a greater prevalence of self-reported diabetes among veterans with an SCI/D compared with the overall civilian population, but that overall diabetes prevalence is similar to that of other veterans. However, for those 45 to 59 years of age, diabetes prevalence was highest in veterans with an SCI/ D followed by general veterans and then the general population. This may lend some support to theories that suggest that there is an earlier onset of diabetes in persons with an SCI/D (7).
Overall, these numbers likely underrepresent the prevalence of diabetes in the SCI/D population; diabetes may be difficult to diagnose in persons with an SCI/D because symptoms are often masked. For example, myocardial ischemia may be silent because of the destruction of sensory pathways, and peripheral neuropathy may be difficult to distinguish from the effects of the cord lesion (14). Likewise, individuals with an SCI/D may not be aware of symptoms heralding diabetes because of the overlapping symptoms associated with their SCI/D. Additionally, the large number of comorbidities associated with having an SCI/D may preclude routine surveillance for diabetes in this vulnerable population.
Among those with diabetes, the most noteworthy difference between individuals with diabetes in the SCI/ D, general veteran, and general population groups is the extremely high percentage of foot sores that took longer than 4 weeks to heal reported by those with an SCI/D. This is not surprising when coupled with the neurogenic hypotension and venous stasis, often associated with spinal cord injury, which may result in diminished peripheral perfusion and subsequently reduced healing rates (15). Because pressure sores on the foot and heel are relatively common in individuals with an SCI/D, eg, Yarkony and Heinemann (16) found that, among persons with spinal cord injury, 15.9% of pressure sores were located on the heel and 4.5% on the foot, it is possible that the high occurrence of foot sores was associated with the spinal injury rather than the diabetes. Additionally, it is possible that foot sores may be underreported in persons with an SCI/D who may be less able to detect foot ulcers caused by paralysis. Regardless, it is known that comprehensive foot care can reduce limb-threatening complications and amputation rates (17,18). In addition to diabetes, reasons for increasing rates of dysvascular amputations include inadequately controlled hypertension and high cholesterol (19); as these findings indicate, persons with an SCI/D are at increased risk for both of these factors. Therefore, attention to foot care in persons with an SCI/D and diabetes is important to reduce further disability. Additional research is needed to identify challenges that may exist in foot care for individuals with both an SCI/D and diabetes.
The Healthy People 2010 objective of providing diabetes education to at least 60% of persons with diabetes has been met among veteran users of the VA health care system (20). Findings from this study suggest that receipt of diabetes education was reported by 50% of those with diabetes in the general population (12), 60% of veterans in general, and 63% of veterans with an SCI/D. It is worth mentioning that many veterans receive their health care both within and outside the VA, so some of their diabetes care may have been received outside of the VA. Reiber et al (21) found that, among male veterans with diabetes who used VA services, 65% received diabetes education; this was significantly higher than the 47% of those who did not use the VA. Therefore, although diabetes services could have been received anywhere, it is likely that the VA is highly conducive to the receipt of this service. Regardless of where education is received, literature suggests that an informed and motivated patient is necessary in managing diabetes and reducing the risk of complications (22), and it seems that veterans with diabetes may be better equipped for diabetes management than persons with diabetes in the general population.
Among those with an SCI/D, these study findings indicate that veterans with paraplegia were more likely to report diabetes than those with tetraplegia. In contrast, Bauman et al (23) found that subjects with tetraplegia were more frequently diagnosed with carbohydrate tolerance disorders than were those with paraplegia. Higher prevalence of diabetes associated with tetraplegia and presumably greater mobility limitation makes intuitive sense on consideration of the pathophysiology of diabetes and its relation to body composition and exercise. The higher prevalence of diabetes in persons with paraplegia in this study was unexpected and may be a factor of the severity of injury (eg, completeness), which was not obtainable from the current data sources. According to the recent study findings of one of the authors (24), it is also possible that risk factors for diabetes such as high blood pressure and obesity are more highly associated with paraplegia (vs tetraplegia), which could explain the higher prevalence of diabetes in persons with paraplegia in this study. It may also be related to physiologic changes that occur in tetraplegia but not paraplegia; therefore, symptoms are not readily apparent. For example, many people with tetraplegia have a blunted hunger sensation and may not manifest with diabetic symptoms of extreme hunger. Finally, it is possible that the use of fasting plasma glucose (FPG) and are less sensitive in persons with hemoglobin (Hb)A1c tetraplegia, resulting in underdiagnosis of diabetes in the tetraplegia population. The use of FPG and HbA1c are less sensitive than oral glucose tolerance tests in detecting lower levels of hyperglycemia (25). Data about the use of diagnostic tests after SCI/D are extremely limited.
In persons with an SCI/D, use of substances such as alcohol and cigarettes has been linked to increased general medical problems (26–28). The findings from this study indicated that veterans with an SCI/D and diabetes were less likely to be current smokers and binge drinkers than those without diabetes.
The American Diabetes Association recommends that if individuals choose to consume alcohol, daily intake should be limited to 1 drink for women and 2 drinks for men (29). The lower percentage of individuals with an SCI/D and diabetes who reported binge drinking suggests compliance with these recommendations. This could be attributable to being well informed and knowledgeable about alcohol consumption guidelines for persons with diabetes, because of the high percentage of individuals with an SCI/D and diabetes that reported having been exposed to diabetes management classes. Given the relatively high average number of visits to health professionals in the prior year for diabetes care or consultation among persons with an SCI/D (mean = 5.5 visits), it is also possible that the lower percentage of binge drinkers may be the result of being advised by health professionals to limit alcohol intake because of diabetes. Health professionals may advise this because increased alcohol intake has been shown to cause individuals to be less attentive to their health problems and to interfere with self-care practices (30).
Individuals with an SCI/D are at risk for many comorbid conditions (31), and those with diabetes are at significantly greater risk, particularly for those comorbidities associated with micro- and macrovascular diseases (8). The results of this study show that, among persons with an SCI/D, those with diabetes were more likely than those without diabetes to report many clinical maladies (including high blood pressure, high cholesterol, stroke, coronary heart disease, and myocardial infarction). This in agreement with literature for individuals with diabetes in the general population who are at increased risk for micro- and macrovascular complications (eg, peripheral arterial disease, coronary heart disease, and strokes) (14,32). Complications can often result in irreversible clinical outcomes, including lower extremity amputation and blindness (33), which lead to functional limitations that are particularly important to avoid in persons with an SCI/D.
Adding complexity, in persons with an SCI/D, many comorbid conditions exist with, are risk factors for, and/ or are related to the presence of diabetes. Cause-and-effect relationships are often unclear because the risk factors for and symptoms of many conditions are similar and related. For example, elevated blood pressures can often be attributed to autonomic dysreflexia, which potentially should be considered a separate risk factor for metabolic syndrome in those with an SCI/D. Nonetheless, individuals with an SCI/D and diabetes together with their health care providers can take steps to reduce the occurrence of diabetes complications by controlling their blood glucose, blood pressure, and blood lipid levels (1).
The study findings indicated that individuals with an SCI/D and diabetes were at greater risk for poor quality of life indicators than were those without diabetes. Individuals with diabetes and SCI/D reported more days in which they experienced debilitating pain, sadness/depression, and lack of enough rest or sleep than did those without diabetes. This is consistent with diabetes literature, in general, which holds that health problems associated with diabetes contribute to an impaired quality of life and considerable disability among people with diabetes (20). Thus, in defining guidelines for health care management in persons with an SCI/D, the impact of diabetes in combination with their SCI on overall health, mobility, and quality of life must be carefully considered.
CONCLUSION
In summary, research has shown that lifestyle changes can prevent or delay the onset of diabetes among high-risk adults. Because of the high prevalence of diabetes in persons with an SCI/D, ways of preventing or delaying the onset of diabetes need to be further explored. Because of increased risk factors for diabetes, cardiovascular, and cerebrovascular events in individuals with an SCI/D, modifiable risk factors, such as obesity, inactivity, blood pressure, and dietary factors, should be addressed. To reduce mortality and morbidity associated with these risk factors, periodic screening for carbohydrate and lipid abnormalities is recommended, with suitable therapeutic interventions when necessary (8). It is unclear what additional challenges are faced by individuals with both an SCI/D and diabetes. However, when persons with SCI/ D have diabetes, it is vital for both the patients and the health care provider to make every effort to manage and control diabetes and its related complications.
The diabetes prevalence question was framed “have you ever been told by a doctor that you have diabetes”; it is possible that some individuals were told that they had diabetes in the past but do not currently have diabetes. Self-reported diagnosis of diabetes may have been affected by the overall sensitivity and specificity of the diagnostic tests used by practitioners. Duckworth et al (25) and Bauman et al (23) found a much higher prevalence of diabetes when using the oral glucose tolerance test. Therefore, diabetes may be underdiagnosed in the SCI/D population, because FPG and HbA1c are more routinely used by practitioners than the oral glucose tolerance test. Data on obesity (body mass index), nutrition, and physical activity were not available for a comprehensive examination of diabetes related factors in the SCI/D population. SCI/D data were collected by a mail survey as opposed to the telephone, as used most often for the CDC-conducted BRFSS survey; therefore, response biases may have occurred. Differences may exist in responses that were asked in self-administered mail format vs interview format (34); however, it was not possible to address potential mode effects for this study.
The general veteran and general populations that were identified using CDC's secondary BRFSS data may have included individuals with SCI because this level of data was not available for exclusion. However, it is unlikely that this would skew the findings, given that, from fiscal year 1998 to fiscal year 2003, the overall number of veterans with an SCI/D to veterans overall (seen at a VA) was 0.32% (S.L.L.V. and S.M., unpublished data, March, 2005) and that the prevalence of SCI in the general population is 0.0009% [using 2005 estimates for the number of people in the United States with SCI of 250,000 (35) divided by US population in 2005 of 285,981,000 (36)]. These data are based on self-reported information and are subject to recall bias. Finally, the low response rate might have influenced the results. Nonetheless, the findings represent the largest sample of veterans with an SCI/D to have completed this behavioral risk assessment to date.
Acknowledgments
The authors thank the Paralyzed Veterans of America (PVA) for distributing this survey to their membership and the survey participants for their time and efforts.
Footnotes
This paper is based on work supported by the Spinal Cord Injury Quality Enhancement Research Initiative (SCI QUERI), Health Services Research and Development, Department of Veterans Affairs. This paper reflects only the authors' opinions and does not necessarily reflect the official position of the Department of Veterans Affairs.
REFERENCES
- Centers for Disease Control and Prevention. National Diabetes Fact Sheet: General Information and National Estimates on Diabetes in the United States 2003. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2004. [Google Scholar]
- Miller DR, Safford MM, Pogach LM. Who has diabetes? Best estimates of diabetes prevalence in the Department of Veterans Affairs based on computerized patient data. Diabetes Care. 2004;27:B10–B21. doi: 10.2337/diacare.27.suppl_2.b10. [DOI] [PubMed] [Google Scholar]
- Hayward R, Pogach LM. VA QUERI Diabetes Mellitus Report. Washington, DC: US Government Printing Office; 2002. [Google Scholar]
- National Spinal Cord Injury Association (NSCIA) Spinal cord injury statistics. Available at: http://www.spinalcord.org/html/factsheets/spinstat.php. Accessed October 20, 2005.
- Bauman WA, Adkins RH, Spungen AM, et al. Is immobilization associated with abnormal lipoprotein profile? Observations from a diverse cohort. Spinal Cord. 1999;37:485–493. doi: 10.1038/sj.sc.3100862. [DOI] [PubMed] [Google Scholar]
- Bauman WA, Spungen AM. Disorders of carbohydrate and lipid metabolism in veterans with paraplegia or quadriplegia: a model of premature aging. Metabolism. 1994;43:949–956. doi: 10.1016/0026-0495(94)90126-0. [DOI] [PubMed] [Google Scholar]
- Bauman WA. The endocrine system. In: Whiteneck GG, Charlifue SW, Gerhart KA, et al., editors. Aging With Spinal Cord Injury. New York: Demos Publications; 1993. pp. 139–157. [Google Scholar]
- Bauman WA, Spungen AM. Carbohydrate and lipid metabolism in chronic spinal cord injury. J Spinal Cord Med. 2001;24:266–277. doi: 10.1080/10790268.2001.11753584. [DOI] [PubMed] [Google Scholar]
- Murata GH, Shah JH, Adam KD, et al. Factors affecting diabetes knowledge in type 2 diabetic veterans. Diabetologia. 2003;46:1170–1178. doi: 10.1007/s00125-003-1161-1. [DOI] [PubMed] [Google Scholar]
- Powell-Griner E, Anderson JE, Murphy W. State-and sex-specific prevalence of selected characteristics—behavioral risk factor surveillance system, 1994 and 1995. MMWR CDC Surveill Summ. 1997;46:1–31. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Survey Questionnaire. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2002 and 2003. [Google Scholar]
- Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Survey Data. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2003. [Google Scholar]
- Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Operational and User's Guide. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2005. [Google Scholar]
- Schmitt JK, Schroeder DL. Endocrine and metabolic consequences of spinal cord injuries. In: Lin VW, Cardenas DD, Cutter NC, et al., editors. Spinal Cord Medicine: Principles and Practice. New York: Demos Medical Publishing; 2003. pp. 221–235. [Google Scholar]
- Priebe MM, Martin M, Wuermser LA, Castillo T, McFarlin J. The medical management of pressure ulcers. In: Lin VW, Cardenas DD, Cutter NC, et al., editors. Spinal Cord Medicine: Principles and Practice. New York: Demos Medical Publishing; 2003. pp. 567–589. [Google Scholar]
- Yarkony GM, Heinemann A. Pressure ulcers. In: Stover SL, DeLisa JA, Whiteneck GG, editors. Spinal Cord Injury: Clinical Outcomes From the Model System. Gaithersburg, MD: Aspen Publishers; 1995. pp. 100–119. [Google Scholar]
- Younes NA, Albsoul AM, Awad H. Diabetic heel ulcers: a major risk factor for lower extremity amputation. Ostomy Wound Manag. 2004;50:50–60. [PubMed] [Google Scholar]
- Caputo GM, Cavanagh PR, Ulbrecht JS, Gibbons GW, Karchmer AW. Assessment and management of foot disease in patients with diabetes. N Engl J Med. 1994;331:854–860. doi: 10.1056/NEJM199409293311307. [DOI] [PubMed] [Google Scholar]
- Dillingham TR. Trauma: crosscutting breakout session. Physical disabilities through the lifespan conference: limb amputations: epidemiology, outcomes, and implications for future research. Neurorehabil Neural Repair. 2005;19(suppl 1):82S–86S. doi: 10.1177/1545968304274030. [DOI] [PubMed] [Google Scholar]
- US Department of Health and Human Services. Healthy People 2010. Understanding and Improving Health and Objectives for Improving Health. Washington, DC: US Government Printing Office; 2000. [Google Scholar]
- Reiber GE, Koepsell TD, Maynard C, Haas LB, Boyko EJ. Diabetes in nonveterans, veterans, and veterans receiving Department of Veterans Affairs health care. Diabetes Care. 2004;27:B3–B9. doi: 10.2337/diacare.27.suppl_2.b3. [DOI] [PubMed] [Google Scholar]
- Glasgow R, Osteen V. Evaluating diabetes education—are we measuring the most important outcomes? Diabetes Care. 1992;15:1423–1432. doi: 10.2337/diacare.15.10.1423. [DOI] [PubMed] [Google Scholar]
- Bauman WA, Adkins RH, Spungen AM, Waters RL. The effect of residual neurological deficit on oral glucose tolerance in persons with chronic spinal cord injury. Spinal Cord. 1999;37:765–771. doi: 10.1038/sj.sc.3100893. [DOI] [PubMed] [Google Scholar]
- Weaver FM, Collins E, Kurichi J, et al. Obesity and high blood pressure in veterans with spinal cord injuries and disorders: risk factors for cardiovascular disease. Am J Phys Med Rehabil. In press. [DOI] [PubMed]
- Duckworth WC, Solomon SS, Jallepalli P, Heckemeyer C, Finnern J, Powers A. Glucose tolerance due to insulin resistance in patients with spinal cord injuries. Diabetes. 1980;29:906–910. doi: 10.2337/diab.29.11.906. [DOI] [PubMed] [Google Scholar]
- Davies DS, McColl MA. Lifestyle risks for three disease outcomes in spinal cord injury. Clin Rehabil. 2002;16:96–108. doi: 10.1191/0269215502cr443oa. [DOI] [PubMed] [Google Scholar]
- Hubbard JR, Everett AS, Khan MA. Alcohol and drug abuse in patients with physical disabilities. Am J Drug Alcohol Abuse. 1996;22:215–231. doi: 10.3109/00952999609001655. [DOI] [PubMed] [Google Scholar]
- Tate DG. Alcohol use among spinal cord-injured patients. Am J Phys Med Rehabil. 1993;72:192–195. doi: 10.1097/00002060-199308000-00004. [DOI] [PubMed] [Google Scholar]
- Franz MJ, Bantle JP, Beebe CA, et al. Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Diabetes Care. 2002;25:148–198. doi: 10.2337/diacare.25.1.148. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ. Drinking patterns and problems, drug use and health services utilization: a comparison of two regions in the US general population. Drug Alcohol Depend. 1999;53:231–237. doi: 10.1016/s0376-8716(98)00138-0. [DOI] [PubMed] [Google Scholar]
- Ditunno JF, Formal CS. Chronic spinal cord injury. N Engl J Med. 1994;330:550–556. doi: 10.1056/NEJM199402243300808. [DOI] [PubMed] [Google Scholar]
- McAlpine RR, Morris AD, Emslie-Smith A, James P, Evans JM. The annual incidence of diabetic complications in a population of patients with type 1 and type 2 diabetes. Diabet Med. 2005;22:348–352. doi: 10.1111/j.1464-5491.2004.01391.x. [DOI] [PubMed] [Google Scholar]
- Winer N, Sowers JR. Epidemiology of diabetes. J Clin Pharmacol. 2004;44:397–405. doi: 10.1177/0091270004263017. [DOI] [PubMed] [Google Scholar]
- Schwarz N, Strack F, Hippler HJ, Bishop G. The impact of administration mode on response effects in survey measurement. Appl Cogn Psychol. 1991;5:193–212. [Google Scholar]
- National Spinal Cord Injury Statistical Center. Facts and figures at a glance. Available at: http://www.spinalcord.uab.edu/show.asp?durki&=21446. Accessed March 29, 2006.
- Campbell P. United States Census Bureau: Population Projections: States, 1995–2025. Current population reports. Available at: http://www.census.gov/. Accessed March 29, 2006. [PubMed] [Google Scholar]